Sexually Transmitted Infections Research Interest Group
LSHTM is a world-leader for STI and HIV research, and a WHO Collaborating Centre for Sexually Transmitted Infections.
STIRIG aim to:
- raise awareness of STI and HIV related research being conducted at LSHTM
- increase cross-disciplinary and cross-Faculty work on STIs including HIV
- develop internal and external collaborations
- maximise funding opportunities
- champion the next generation of STI and HIV researchers
Leadership team
|
Sarah Harman Faculty of Epidemiology and Population health |
Emma Harding-Esch Faculty of Infectious and Tropical Diseases |
Emma Slaymaker Faculty of Epidemiology and Population health |
|
Daniel McCartney Faculty of Infectious and Tropical Diseases |
Peter Weatherburn Faculty of Public Health and Policy |
Richard Hayes Faculty of Epidemiology and Population health |
|
Philippe Mayaud Faculty of Infectious and Tropical Diseases |
Michael Marks Faculty of Infectious and Tropical Diseases
|
Pitchaya Peach Indravudh Faculty of Public Health and Policy |
|
Aiofe Doyle Faculty of Epidemiology and Populations Health |
Matthew Chico Faculty of Infectious and Tropical Diseases
|
Matthew Quaife Faculty of Public Health and Policy
|
|
Amanda Gabster Faculty of Infectious and Tropical Diseases |
Yunia Mayanja LSHTM MRC/UVRI Uganda |
Clare Broad LSHTM/St George’s University of London |
How to 'Decolonise' MSc Summer Research Projects at LSHTM
A collaborative workshop series by STIRIG and Decolonising Global Health at LSHTM
Facilitated by STIRIG, in collaboration with Decolonising Global Health (DGH-LSHTM), this new workshop series aims to bridge the gap between theoretical understanding of decolonisation and its practical application in the LSHTM MSc Summer Projects. The first workshop of the series was successfully hosted in December, tailored to the challenges of the brainstorming and ideas phase of MSc Summer Projects, reflecting the research stage most Masters students were currently facing. It employed a modified, beginner-friendly journal club format that was designed to be accessible to all early-career researchers.
Understandably, the term decolonisation has many different interpretations, definitions and applications. STIRIG's student representatives approached the concept of 'decolonising' research, specifically 'decolonising' MSc Summer Projects, through the interpretation of actively working to challenge and combat the inequity and injustices that exist in research systems and processes, as a consequence of colonial legacies. Whilst the practical applications of decoloniality will look very different in different research contexts and disciplines, the workshops throughout this series aim to offer a platform for students to start to explore possible implications for their MSc Summer projects.
Throughout this first workshop of the series, it was acknowledged that with the privilege of producing research within a higher education institution, such as LSHTM, comes significant power. Research produced at LSHTM may go on to influence policy, direct innovations, promote discourse and shape the way knowledge is produced, communicated and understood. Research not only describes the world, but it has the potential to shape how others see the world. With this immense privilege, comes the responsibility to take active steps to address colonial research legacies through each stage of the MSc Summer Project process, especially given the pivotal role these projects can play in shaping the academic and research trajectory of these participants.
The discussion focused on a recently published piece of HIV research, facilitating student engagement with a real-world research example. By focusing on HIV and sexual health research, a key area within public health research, the workshop provided a practical lens through which students could explore the complexities of decolonisation in a specific context, laying the groundwork for broader applications in diverse research areas. Through the students’ exploration of power dynamics, cultural biases, and ethical considerations specific to decolonising sexual health research, the students gained valuable insights that could guide their decision-making process during the brainstorming phase.
STIRIG's student representatives sought to make these decolonisation principles tangible and applicable specifically to the participants' MSc research endeavours. To achieve this, they worked closely with DGH-LSHTM to develop a simple decolonial brainstorming framework based on current literature regarding decolonial research principles. Throughout the session, students were given the opportunity to apply this framework to the piece of HIV research presented in the journal club allowing for a nuanced exploration of real-world applications, as well as to their own research ideas. This framework offered MSc students a potential place to start when considering decoloniality applications in their MSc Summer Project.
The discussions throughout this workshop illustrated the importance of creating a space for collaborative analysis of the implications of colonial legacies throughout the entire research process. Whilst this first workshop focussed on the initial stage of the student's research journey, it set the stage for future STIRIG + DGH workshops in this series that will address subsequent stages of MSc Summer Projects. STIRIG aims to offer targeted workshops that address the unique challenges and opportunities presented at each stage, ensuring continuous support to explore decoloniality where possible throughout the Summer Project research process.
Rosie Matthews
STIRIG Student Rep
STIQ Day
January 14th marked STIQ (Sexually Transmitted Infection Question) Day, an educational day of observance highlighting the need to ask questions, foster a stigma-free environment, address misinformation, and emphasize the importance of comprehensive reproductive health education covering sexually transmitted infections.
We are in an era where information is available at our fingertips, and the sexual health landscape can be difficult to navigate due to the prevalence of misinformation on online platforms. Young people who are the most digital are especially susceptible to these mixed messages, and may be left vulnerable by a lack of comprehensive sexual and reproductive health education covering topics surrounding sexually transmitted infections and prevention methods.
According to the World Health Organization, roughly 1 million sexually transmitted infections are acquired each day globally, and STIs are on the rise. Education disruptions during the COVID-19 pandemic mean young people may have missed out on vital sexual and reproductive health education that could have addressed misinformation on STIs and given young people valuable resources to protect themselves.
Coming from a background in education, holding a passion to increase information on STIs in sexual and reproductive health education, I want to remind us on STIQ Day:
-To address stigma surrounding STIs in your community.
-To consider donating or supporting local NGOs working in STIs.
-To check in with young people in your community and start a conversation.
A reminder to never stop asking questions about STIs - to learn more, share more, and grow a healthier society.
(Kaja Swenson, STIRIG Student Rep 23/24)
Become a STIRIG Student Rep!
It’s important to us to develop our student community and ensure that your views and experiences are incorporated into our work – championing the next generation of STI and HIV researchers is one of our core objectives. We’re seeking to appoint up to three student representatives for the coming academic year to work closely with our co-directors on the following:
- Identifying key areas of interest for STIRIG seminars and helping to organize
- Suggesting themes and co-producing at least two newsletters
- Developing student specific activities e.g. journal clubs, feedback sessions, blog-writing
- Communicating STIRIG activities to your networks and other students
If you’re interested in becoming a student rep please submit the following to stirig@lshtm.ac.uk by 5pm on Sunday 8th October.
- CV
- A short email outlining
- What you’d like to achieve from the role
- Relevant experience
- One idea for a possible event or activity
- Which MSc you are taking
Each issue spotlights our research on sexually transmitted infection, and the latest STI-related news.
LSHTM was designated as a WHO Collaborating Centre for STIs in May 2021. The key objectives are to:
1. Support the development, implementation and evaluation of STI diagnostic strategies
2. Assist WHO in activities that aim to improve STI prevention and control and sexual and reproductive health (SRH) services in key and vulnerable populations for STIs including HIV
3. Provide support to WHO in activities related to elimination of STIs and their sequelae
The STI Research Interest Group (STIRIG) is a community of staff and students who are interested in research related to STIs, including HIV. We work closely with the WHO Collaborating Centre for STIs at LSHTM and aim to raise awareness of STI-related research being conducted at LSHTM.
LSHTM students and staff can join our internal membership list to get LSHTM-specific updates – you can sign up for membership with your LSHTM email address here. We also have a newsletter that anyone can access (you don’t have to have an LSHTM email address) – you can sign up for this here.
Are you interested in being an MSc student representative for STIRIG? Student representatives will work together in a team to identify and organise key areas of interest for LSHTM students, including seminars, activities and communications – advocating for the issues that are important to the student community. We're asking anyone who's interested to send an email to stirig@lshtm.ac.uk with the title: STIRIG Student Reps – MSc, by Friday 16th October.
9-10th January 2020 at the London School of Hygiene & Tropical Medicine
Antimicrobial resistance (AMR) in sexually transmitted infections (STIs) is a major public health threat, with Neisseria gonorrhoeae being designated as a “high priority antibiotic resistant pathogen” by the World Health Organization (WHO).
A two day conference was organised by LSHTM's STI Research Interest Group (STIRIG), co-hosted with LSHTM’s AMR Centre, Bristol Health Partners’ Sexual Health Improvement Programme Health Integration Team (SHIP), Public Health England (PHE) and the World Health Organization (WHO). Around 160 participants attended the conference at LSHTM in person and 60 viewers from around the globe followed the conference via livestream.
Conference objectives were:
-
To develop a network to share knowledge and experiences of effective strategies and bottlenecks for tackling STI AMR, both locally and globally
-
To identify bottlenecks and solutions for tackling STI AMR and
-
To develop a short- and long-term action plan on STIs and AMR.
Eight session covered topics such as surveillance, treatment guidelines, new diagnostic and treatment initiatives, antibiotic stewardship, and vaccines. Each session was followed by a panel discussion.
Speakers were world class experts from a broad range of disciplines including social sciences, natural sciences, medicine and public health. STIRIG delivered on its diversity pledge (adapted from the Lancet’s Diversity Pledge) with high representation of gender and ethnic diversity among its speakers, including colleagues from low and middle-income countries. The conference ended with a very thought-provoking and inspiring discussion on current gaps and future opportunities of AMR in STI control.
The full programme can be found here and recordings of presentations are available here.
Please follow @STIRIG_LSHTM on twitter and join one of our regular events (https://www.lshtm.ac.uk/research/centres-projects-groups/stirig)
Meeting of the 21st IUSTI World Congress, Bangkok
1-4 December 2020
- Deadline for abstracts and scholarships submissions: 31 July 2020
24th Meeting of European Congress on Sexually Transmitted Infections and HIV / AIDS
3-5 September 2020, Bucharest
- Abstract submission deadline: 1 June 2020
- Early Bird registration deadline: 1 June 2020
An opportunity for MSc students to come and meet potential supervisors to discuss summer projects. Bring your own lunch!
- Date: Tuesday 10 December 2019
- Time: 1-2pm
- Venue: Keppel Street room LG24
For further enquiries, please contact: Sarah Harman at sarah.harman@lshtm.ac.uk
Joint Meeting of the 23rd ISSTDR & 20th IUSTI Congress 14-17 July, 2019 in Vancouver, Canada.
- Abstract Submission Deadline: EXTENDED to 1 February 2019 (23:59 PST)
- Scholarship Application Deadline: January 25, 2019 (23:59 PST)
30 June - 2 July
Registration is OPEN! Natsal at BASHH: The Natsal team will be hosting a stand at the BASHH Annual Conference. As part of preparations to ensure the new wave of Natsal is ‘fit-for-purpose’ ahead of interviews starting in 2021, we’re keen to get stakeholders’ input – so we need you!
Please do pop by to find out more about this internationally-renowned study, what the new wave will focus on, how it will be done – and why, and importantly, to add your voice as to the questions that you think Natsal-4 needs to ask. If you can’t make it to our stand, then you can still participate in Natsal’s online consultation which will be going live in July.
Tallinn, Estonia
5-7 September 2019
The 33rd IUSTI-Europe Congress on Sexually Transmitted Infections.
23-27 March 2020
Barcelona, Spain
The 33rd International Papillomavirus Conference & Basic Science, Clinical and Public Health Workshops.
Abstract Submission is open. The deadline is 10 September 2019.
The WHO and Find (Foundation for Innovative New Diagnostics) are having a public consultation.
They are requesting feedback on two target product profiles for improved antimicrobial stewardship of gonorrhea treatment.
SHIP was set up as a Bristol Health Partners Health Integration Team in 2013. It brings together UK experts from across disciplines to improve the sexual health of people in the region and reduce STIs. The team supports the commissioning of evidence-based sexual health services.
SHIP and STIRIG are strategic partners. Read about our 2018-19 successes.
To enquire about the role, please email Katy Turner.
The Health and Social Care Committee has made five recommendations for a new national strategy to the government.
European Society for Microbiology and Infectious diseases (ESCMID) has extended their Mycoplasma Study Group to include chlamydia in 2019. Members of this group can (i) receive information related to this study group, (ii) increase their chlamydia network, and (iii) be eligible for opportunities linked to the ESCMID study group, such as specific grants for starter projects as well as postgraduate courses. You must be a member of ESCMID before joining the group.
Call for applications for an STI PhD studentship. The Sexually Transmitted Infections Research Foundation (STIRF) has awarded a 3-year PhD studentship at the University of York, called “HPV vaccination for preventing cervical and other HPV-associated cancers: Comparing the knowledge and understanding of factors influencing initiation and completion of the UK and Ugandan school-based vaccination programme”. Deadline for applications 14th March 2019.
We are delighted to introduce our logo competition for all students at the School, both in London and around the world. The deadline for entries is 15 December 2018 and all entries should be sent to stirig@lshtm.ac.uk. See here for more information and the competition rules.
The Sexually Transmitted Infections Research Foundation (STIRF) has awarded a 3-year PhD studentship at the University of York, UK called “HPV vaccination for preventing cervical and other HPV-associated cancers: Comparing the knowledge and understanding of factors influencing initiation and completion of the UK and Ugandian school-based vaccination programme”.
The Sexual Health Improvement Programme (SHIP), which Dr Emma Harding-Esch is Honorary Co-Director of, co-hosted with BASHH an open meeting in Bristol on “Preparing Sexual Health Services for the Challenge of Antimicrobial Resistant (AMR) bacteria”.
STI-related research projects and collaborations at LSHTM
Collaborations
- WHO Collaborating Centre for Sexually Transmitted Infections
LSHTM is one of eight WHO Sexually Transmitted Infection (STI) Collaborating Centres worldwide. The Centre works with the WHO Global HIV, Hepatitis and STIs Programme (HHS), the UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), and a network of international collaborators on activities to improve the prevention, control and management of STIs worldwide.
The key objectives of the Centre are to
1. Support the development, implementation and evaluation of STI diagnostic strategies, including point-of-care tests (POCTs); training; health systems research; laboratory capacity building; and advise on research/validation, test performance, process and impact evaluations.
2. Assist WHO in activities that aim to improve STI prevention and control and sexual and reproductive health (SRH) services in key and vulnerable populations for STIs including HIV (support normative work [e.g. guidelines]; generate evidence to inform policy and programmes including STI prevalence and surveillance, sexual behaviour, SRH service access and use; and training).
3. Provide support to WHO in activities related to elimination of STIs and their sequelae, including cervical cancer, and mother-to-child-transmission of STIs including HIV, hepatitis and syphilis.- Health Protection Research Unit in Blood Borne and Sexually Transmitted Infections
The National Institute for Health Research (NIHR) Health Protection Research Unit in Blood Borne and Sexually Transmitted Infections is led by University College London in partnership with Public Health England and LSHTM. The unit aims to conduct state-of-the-art research to improve the health of the population, and to help develop practical policy guidelines for those working in health protection.
The NIHR HPRU has received almost £3.7 million to undertake collaborative research that addresses the key health protection priorities for the prevention and control of STIs and BBVs, notably understanding risk and risk reduction, reducing the burden of under-diagnosis, and improving care and management of those diagnosed with infections.
There are three research themes
- Theme A: Understanding risk and risk reduction for STIs and BBVs
- Theme B: Reducing the burden of undiagnosed STIs and BBVs
- Theme C: Improving the care and management of people with STIs and BBVs
LSHTM investigators
- Theme A: Understanding risk and risk reduction for STIs and BBVs
- SHIP (Sexual Health Improvement Programme)
The Sexual Health Improvement Programme (SHIP) was set up as a Bristol Health Partners Health Integration Team in 2013. It brings together experts from across disciplines to improve the sexual health of people in the region and reduce STIs, supporting the commissioning of evidence-based sexual health services. Our priorities are: increasing uptake of HIV testing; improving STI testing and responding to antimicrobial resistant (AMR) infections; increasing patient and public involvement in sexual health and ending stigma; ending domestic violence; reducing health inequalities; implementing informatics and digital transformation; developing a national network for sexual health improvement. A major focus for the next three years will be evaluating and developing strategies, including vaccination, for combating the development of antimicrobial resistance (AMR) in STIs.
Stay up-to-date with our newsletter
LSHTM investigator
- The Applied Diagnostic Research and Evaluation Unit (ADREU)
The Applied Diagnostic Research and Evaluation Unit (ADREU) based at St George’s, University of London (SGUL) is a proven multi-institutional and multi-disciplinary group including experts in clinical medicine, diagnostic evaluations, epidemiology, public health, social science, basic and translational science. ADREU provides a comprehensive service to facilitate the development and evaluation of rapid diagnostics for STIs, other infectious diseases and antimicrobial resistance for both academic institutions and industry. ADREU offers bespoke diagnostic accuracy evaluations, from proof-of-concept projects to late-stage evaluations, providing data for regulatory approval for our collaborating partners in academia and industry. With close links to Public Health England and LSHTM, ADREU combines real word situations with leading academic insight to evaluate novel commercial technologies, providing feedback on the clinical and social impact that STIs and rapid STI diagnostics can have on all aspects of the healthcare system, from patients to healthcare professionals.
LSHTM investigator
Staff-led research projects
- safetxt: A randomised controlled trial of an intervention delivered by mobile phone messaging to reduce STI in young people
The NIHR-funded safetxt Trial is a single blind randomised controlled trial to evaluate the effect of a safer sex intervention delivered by text message on chlamydia and gonorrhoea infection at 12 months. The intervention targets partner notification, condom use and getting tested before unprotected sex with a new partner (1).
Over 5900 participants aged 16-24 have been recruited from 50 GU and Sexual and Reproductive Health services across the UK.Full recruitment is crucial to provide trials with sufficient power to detect intervention effects, yet only 56% of publicly funded trials in the UK achieve their target sample size.
Mixed methods supported by evidence from behavioural science were used to maximise recruitment including meetings with site staff to enable new services to learn from experienced recruiters, monthly newsletters to highlight major achievements, competitions to develop engagement and motivation and certificates for staff who achieve recruitment milestones.
The questionnaire follow-up of participants is closely monitored and is currently 88.2% at 4 weeks and 77.1% at 1 year. The return of test kits at 1 year is 71.8%. Steps taken to improve follow up rates include: simplified test kit instructions, clear postage instructions, and a prize draw entry for participants who return test kits (2).
The safetxt collaboration between 50 GU and Sexual and Reproductive Health services and the trial management team is on target to recruit 6250 participants on time by December 2018. The trial is due to report in 2020.
LSHTM investigators
Caroline Free, Ona McCartney, Rebecca French, Kaye Wellings
References
Free C, McCarthy O, French RS, Wellings K, Michie S, Roberts I, et al. Can text messages increase safer sex behaviours in young people? Intervention development and pilot randomised controlled trial. Health Technol Assess 2016;20(57)
McCarthy O, French RS, Roberts I, Free C. Simple steps to develop trial follow-up procedures. Trials. 2016;17:28. doi:10.1186/s13063-016-1155-1- TracVac: A phase I adjuvant Chlamydia trachomatis vaccine
TracVac builds on the results of a phase I clinical trial (NCT02787109) of an adjuvanted Chlamydia trachomatis vaccine (CTH522; Olsen et al 2015, JID PMID2578320) developed by Statens Serum Institut (SSI), Copenhagen. TracVac (www.trachoma-vaccine.org) is a 4 partner (LSHTM, Imperial College London, Commissariat à l’Energie Atomique et aux Energies Alternatives, Paris and SSI) EU sponsored consortium that will expand the C. trachomatis serotype coverage of CTH522 and investigate the immunization regimen required for the optimal induction of protective responses at mucosal surfaces that include the eye. C. trachomatis infection of the eye causing trachoma remains the leading cause of blindness due to any infection. The immunological routes of C. trachomatis protection and pathogenesis in both the eye and urogenital tract are believed to share common features. There are currently no chlamydial vaccines licenced for human use. We expect that study of trachoma can serve as a useful and translatable model for C. trachomatis vaccine development in addition to the delivery of vaccine that protects against ocular infection. We are using novel Human B cell cloning technologies to select neutralizing and protective epitopes from trachoma ‘resistant’ individuals. We have identified 'resistant' individuals from longitudinal cohort studies. The selected epitopes will be incorporated into the next generation recombinant vaccine. Antibody neutralization and cellular responses to the vaccine constituents are being further tested on a wider scale in longitudinal trachoma cohort studies established LSHTM from The Gambia and Tanzania. By the end of the study we aim to deliver a vaccine that covers both urogenital and ocular C. trachomatis infection for further clinical development in 2020.
LSHTM investigators
Martin Holland; Harry Pickering
- iGugu: Prevalence of STIs among young people in South Africa: A nested survey in a health and demographic surveillance site
iGugu means precious, and is short for Ukuvikela impilo yetho yokuzalana eyigugu, Zulu for "protecting our precious reproductive health."
Adolescents and young adults are particularly vulnerable to sexually transmitted infections (STIs). The first strategic direction of the WHO Global Health Sector Strategy on Sexually Transmitted Infections 2016-2021 is to collect information on STI prevalence and incidence across representative populations. There is also evidence that bacterial vaginosis (BV) is a risk factor for poor birth outcomes and STIs including HIV. The collection of BV prevalence may therefore also be important. However, developing new cohorts for dedicated STI/BV prevalence studies may not be realistic, particularly in sub-Saharan Africa, where the impact of STIs/BV and their consequences may be greatest. Therefore, nesting STI/BV surveys within networks of health and demographic surveillance sites (HDSSs) could be an efficient way of providing data to better understand STI epidemiology among adolescents and young people in high HIV prevalence settings.
We carried out a nested STI/BV survey among 1,342 adolescent and young people in an HDSS in KwaZulu-Natal, South Africa, between October 2016 and January 2017. Potential participants were contacted at home and invited to participate. Participants were interviewed, and samples were collected for STI/BV testing.
We showed that this study was feasible within the 3.5-month time period: 1,171/1,342 (87%) individuals had ≥1 attempted home visit, of whom 790 (67%) were successfully contacted (1).
The study was acceptable: among those contacted and eligible, 447/645 (69%) enrolled. Both men and women reported few problems with sample collection. We report a high burden of STIs/BV in this population, particularly of chlamydia (5% in men and 11% in women), herpes simplex virus type 2 (17% in men and 29% in women), and BV (42% in women).
Nested STI/BV surveys in HDSSs can be feasible and acceptable; however, more survey time is needed to ensure that all potential participants are visited and contacted. These studies should be carried out in conjunction with studies to measure STI/BV prevalence in high-risk populations (e.g. female sex workers) to provide robust prevalence estimates.
These data are essential to advocate, fund, plan, implement, and evaluate interventions for STI prevention and control among adolescents and young people. Strategies for the prevention and control of chlamydia, herpes simplex virus type 2, and BV are needed in this population.
LSHTM Investigators
Suzanna Francis; Kathy Baisley
References
Francis SC, Mthiyane TN, Baisley K, Mchunu SL, Ferguson J, Smit T, Gareta D, Dlamini S, Mutevedzi T, Seeley J, Pillay D, McGrath N, Shahmanesh M. Prevalence of Sexually Transmitted Infections among Young People in South Africa: A Nested Survey in a Health and Demographic Surveillance Site. PLOS Medicine, 2018; 15(2):e1002512
- Systematic Review: Novel testing technologies, strategies and approaches for testing populations at high risk of STIs in EU/EEA countries
In 2012, the European Centre for Disease Prevention and Control (ECDC) published the technical report “Novel approaches to testing for sexually transmitted infections, including HIV and hepatitis B and C in Europe”. This report was a comprehensive review of testing technologies and strategies across Europe. Almost six years later, there have been a number of developments in the field, and an updated review is required.
We are carrying out a critical appraisal via a systematic literature review of novel STI testing technologies, strategies and approaches for detecting Chlamydia trachomatis, Neisseria gonorrhoeae, Treponema pallidum, Mycoplasma genitalium, and Trichomonas vaginalis, in at-risk populations. The objectives are to: describe novel (since 2011) STI testing strategies and approaches and determine how they impact on access to testing, testing coverage, and linkage to care; describe what testing technologies are used in these novel strategies and approaches; describe the impact of novel testing technologies, approaches and strategies on reporting to public health surveillance programmes; highlight quality assurance needs and risks; and highlight their feasibility and acceptability. Gaps in knowledge and data availability will also be identified to highlight future research needs.
LSHTM investigators: Emma Harding-Esch; Suzanna Francis
Research degree student projects
- Factors associated with sexual behaviour and sexually transmitted infections among adolescents in Comarca Ngäbe-Buglé, Panama
PhD Student: Amanda Gabster
PhD supervisors: Philippe Mayaud and Beniamino Cislaghi
The aim of Amanda’s PhD is to describe the factors that contribute to sexual behaviour and sexually transmitted infections (STI) outcome among adolescents (14-19 years) of the indigenous region called the Comarca Ngäbe-Buglé (CNB), Panama, in collaboration with the Gorgas Memorial Institute for Health Studies in Panama. The PhD employs mixed methods. In the first stage, qualitative methods were used to describe gender norms, other social norms, and parenting styles of adolescent and parents of adolescents of CNB. Results from this stage informed the study tools for the second stage. In the second stage was a cross-sectional study with two-stage cluster sampling. It was carried out with 700 adolescents to investigate the association of social norms, parenting styles, and sexual behaviours, with STIs. The prevalence of the following STIs and reproductive tract infections were measured: HIV, syphilis, hepatitis B virus, human T-lymphotrophic virus, herpes simplex virus type 2, chlamydia, gonorrhea, high-risk human papillomavirus (women only) and bacterial vaginosis (women only). This study is the first to explore the factors related to adolescent sexual health in CNB. Based on the results of this research, governmental and non-governmental agencies will work towards targeted, culturally competent, sexual health interventions for indigenous adolescents of the Comarca Ngäbe-Buglé. Funding for this project was obtained from Panama's National HIV/STI/Viral Hepatitis Program and support from the Gorgas Memorial Institute for Health Studies.
- Inflammation and the vaginal microbiota in Zambian Women with Female Genital Schistosomiasis and their potential role in HIV acquisition
PhD Student: Amy Sturt
PhD Supervisors: Amaya Bustinduy, Emily Webb and Suzanna Francis
The overall aim of Amy’s PhD research is to explore the potential role of female genital schistosomiasis (FGS), sexually transmitted infections (STI), and the vaginal microenvironment in HIV acquisition. Female genital schistosomiasis (FGS) affects over 45 million women worldwide, mostly in sub-Saharan Africa. FGS is caused by an infectious agent, the waterborne parasite Schistosoma haematobium. Genital tract morbidity is caused by inflammation from egg-deposition that leads to mucosal erosion and granulomatous reaction. There is cross-sectional evidence of increased HIV prevalence in S. haematobium infected women. Amy’s research takes place in Livingstone, Zambia where eligible women were recruited from communities within HPTN071 (PopART) that are also endemic for infection with S. haematobium. The vaginal microbiota in FGS have not yet been evaluated and literature evaluating the association of FGS and STI is limited. As non-optimal cervicovaginal microbiota and STI have both previously been associated with HIV acquisition, Amy is evaluating the association between FGS and vaginal dysbiosis or STI (including chlamydia, gonorrhea, trichomoniasis, infections with Mycoplasma genitalium and Herpes simplex virus types 1 and 2). This may provide further evidence to strengthen the understanding of the mechanism of the association of FGS with HIV acquisition. Amy also plans to evaluate HIV incidence rates in women with and without FGS.
- The epidemiology of, and risk factors for, oro-genital and anal human papillomavirus infections among sexually active Nigerians: A mixed methods study
PhD Student: Imran Morhason-Bello
PhD Supervisors: Deborah Watson-Jones and Suzanna Francis
Imran’s PhD aims to describe risk factors for genital, oral and anal sexual intercourse, and association of these behaviours with the prevalence of genital, oral and anal human papillomavirus (HPV) infections among different heterosexual populations in Ibadan, Nigeria. The first part of the PhD was a systematic review of reported oral and anal sex among heterosexual adolescents and adults in sub-Saharan Africa. This review informed the mixed methods study which enrolled adolescent girls and young women from the general populations and brothel-based female sex workers (FSW). Stage 1 of the study included formative research to explore the knowledge, socio-cultural interpretations, local terminologies, and personal experiences with different sexual behaviours within the community. Results from this stage informed the tools for Stage 2. Stage 2 was a cross-sectional survey using household sampling of adolescents/young adult females, and brothel sampling of FSWs. During the cross-sectional survey, face-to-face interviews, clinical examination and collection of samples were carried out. A blood sample was collected for HIV testing. Samples from the oral cavity, the genital area (vulva, cervix and penis) and anal canal was collected for HPV DNA genotyping in the laboratory. The research was support by University of Ibadan, Ibadan, Nigeria.
- Detecting sexual bridges: rapid genome-mapping of sexually transmitted infections among female sex worker and non sex worker populations in Ecuador
PhD Student: Claire Broad
PhD Supervisors: Phil Cooper (SGUL/LSHTM), Tariq Sadiq (SGUL), Ken Laing (SGUL)
Claire’s PhD is a part of the MRC London Intercollegiate Doctoral Training Partnership (MRC LID) between St George’s University of London (SGUL) and LSHTM. The aim of this project is to estimate the prevalence of sexually transmitted infections (STIs) among female sex workers in Quininde and Las Golondrinas, Ecuador, and to demonstrate a system of surveillance that identifies sexual transmission clusters and potential sexual transmission ‘bridges’ within the general population. In Latin America, like many low- and middle-income countries, control of STIs is limited to syndromic management and there are a lack of reliable testing platforms, lack of knowledge surrounding STIs and unregulated antibiotic usage, e.g. self-medication. In Ecuador, surveillance strategies are limited and rely on disease case reporting of STI syndromes; few laboratory diagnosed STI prevalence data are available for common infections such as chlamydia and gonorrhoea. It is important when implementing public health interventions to understand whether an outbreak in a high risk population, such as female sex workers, will lead to infection ‘bridging’ and affect the wider population. Surveillance systems that incorporate methods such as whole genome sequencing (WGS) can be used to identify strain types, geographical clustering and antimicrobial resistance patterns within a population. WGS enables targeted capture of specific bacterial genomes; however, culture is usually required to provide sufficient pathogenic material and reduce interference from other bacterial or human DNA. For STIs such as chlamydia and infection with Mycoplasma genitalium, culture techniques are specialised, expensive and have varying success rates. Enrichment methods (e.g. using hybridization or ‘bait’ capture, bypassing culture and amplifying bacterial genomes directly from clinical samples) are an attractive resource for field settings and LMICs. The main output from the thesis will be to optimise enrichment and amplification methods to allow direct sequencing from clinical samples which have been collected from sex worker and non-sex worker populations in rural regions of Ecuador.
- Epidemiology of sexually transmitted infections (STIs) in a cohort of transgender women in São Paulo, Brazil
DrPH Student: Daniel McCartney
DrPH Supervisor: Philippe Mayaud
Daniel’s DrPH project aims to assess the prevalence and incidence of sexually transmitted infections (STIs) among transgender women in São Paulo, Brazil, including chlamydia, gonorrhoeae, trichomoniasis, Lymphogranuloma venereum (LGV) and infection with Mycoplasma genitalium through laboratory diagnosis of self-collected samples from anorectal, oropharyngeal and neovaginal sites. This project is nested within an ongoing cohort study of transgender women by the Santa Casa de São Paulo School of Medicine, and a preliminary study was conducted to assess the acceptability of providing self-collected samples among a sample of transgender women enrolled in the cohort study.
While recommendations for serologic screening (for HIV, syphilis and hepatitis) and management of confirmed STIs do not differ from those for non-transgender people, specific considerations are required when screening for other STIs, as transgender people differ in hormone use, history of gender-affirming surgical procedures, and patterns of sexual behaviours and practices. Often conflated with men who have sex with men (MSM), transgender women have been underrepresented in epidemiological studies of STIs.
Research findings will have important policy and public health implications in Brazil and internationally for improving STI screening of this often over-looked and underserved population and inform specific STI-related recommendations for transgender women including screening and syndromic management for anorectal, oropharyngeal and neovaginal infections and syndromes.
- Assessing the effect of economic shocks on HIV, STIs and Risky Sexual Behaviours
PhD Student: Henry Cust
PhD Supervisors: Dr Tim Powell-Jackson (LSHTM), Dr Aurélia Lépine (University College London) and Dr Rosalba Radice (City, University of London)
Henry’s PhD aims to better understand the circumstances in which FSWs have unprotected (condomless) by modelling the decision to have unprotected sex as a rational economic decision to earn additional money in times of need among female sex workers (FSWs). Economic shocks, where the finances of a household dramatically changes due to a change in income or a change in expenditures is one explanation as to why FSWs choose to have unprotected sex. Additional money earned from unprotected sex is used to make up the difference between regular earning and their income after a shock. This “risk premium” for unprotected sex can be as high as 81% in low and middle income countries.
Henry’s PhD will contribute to this area of research by providing new evidence from two unique settings, one in urban Senegal with a dataset of FSWs collected in Dakar over a two-year period. Sex work is legal in Senegal on the condition FSWs attend and pass a monthly health check for STIs. He will explore the evidence that economic shocks lead to risky sexual behaviours and STIs. Second, Henry is using a dataset from Karnataka state in southern India, which collected information from a group of sex workers predominantly from the devadasi background where sex work is culturally accepted. He will study the effects of economic shocks in both of these settings, including the different responses when the shocks are anticipated and unanticipated to see how risky sexual behaviours differ. He will also evaluate the effectiveness of interventions designed to protect against economic shocks such as personalised savings accounts.
- Pharyngeal gonorrhoea as a driver of antimicrobial resistance; how can we better control it?
PhD Student: Victoria Miari
PhD Supervisors: Richard Stabler and David Mabey
Vicky is a clinical scientist at LSHTM and carrying out a staff PhD. Her PhD has several strands, all relating back to pharyngeal gonorrhoea. She first looked at patients with multi-site gonorrhoea and found that 15% of those patients carried different gonococcal strains in different anatomical sites which has an impact on detection of antimicrobial resistant (AMR) gonococcal strains and surveillance of those strains. She is also in the process of evaluating antimicrobial compounds that could potentially treat gonorrhoea – some compounds are novel and some are existing ones used in a new way.
Antimicrobial resistant gonorrhoea has been on the public health radar for some time now. More recently, ‘super gonorrhoea’ has crossed into mainstream news, especially with the recent multi-drug resistant (MDR) case. These MDR gonococcal strains have been surfacing spontaneously since 2011 and since then, no new antimicrobials have been approved to reliably treat gonorrhoea. She has evaluated the activity of closthioamide (CTA), a new antimicrobial class, against several strains of N. gonorrhoeae, and although very effective in vitro, CTA is at the early stages of development and could be years before it is available as a treatment. This research was published in Antimicrobial Agents and Chemotherapy. She is also evaluating chlorehexidine, readily available within dental mouthwashes, to be used topically as a gargle.
This is particularly important; pharyngeal gonorrhoea is difficult to treat. She has found that chlorhexidine has high efficacy against gonorrhoea; the median minimum bactericidal concentration is approximately 65 fold less than the concentration in commercial mouthwashes. Chlorhexidine also appears to be rapidly bactericidal against gonorrhoea, taking less than a minute to kill 10 million bacteria. Vicky is continuing to research chlorhexidine and the next stages will be to perform a randomised controlled trial of a gargle to treat pharyngeal gonorrhoea.
She has written an editorial for Sexually Transmitted Infections about the role of topical antiseptics. As a clinical scientist she is also developing a diagnostic molecular test, able to detect live bacteria in human specimens. She hopes that this test will enable clinicians to detect AMR strains much faster, by reducing the test of cure time period. Lastly, she is further interested in genetic exchange between N. gonorrhoeae and commensal Neisseria species in the pharynx and is preparing cross sectional study to measure the carriage of resistant commensals in MSM.
STI-related publications since September 2018
Training and courses
- Control of STIs: LSHTM study module (D1 slot)
- Principles of STD/HIV Research: A 2-week course held annually in July by the University of Washington Centre for AIDS and STDs
- The NHS has an e-learning programme, eHIV-STI
- The British Association of Sexual Health and HIV (BASHH) has a list of UK based training courses and meetings.
- Faculty of Sexual and Reproductive Healthcare (FSRH) is a faculty of the Royal College of the Obstetricians and Gynaecologists publishes education and training opportunities.
- US Center for Disease Control and Prevention (CDC) online training in STDs
- The Royal College of Nursing (RCN) Sexual Health Education & training resource have published their new sexual health resources:
- Sexual and reproductive health: education, training and career progression in nursing and midwifery publication
- A new education directory to highlight the training and qualification requirements for nursing staff working in sexual health
Guidelines
- WHO Global Strategy on STIs and WHO treatment guidelines
- International Union against STI (IUSTI) European STI Guidelines
- Guidelines for the British Association of Sexual Health and HIV (BASHH)
- US Center for Disease Control and Prevention (CDC) 2015 STD Guidelines
Professional societies
- British Association of Sexual Health and HIV (BASHH) membership information
- International Union against STI (IUSTI) membership information
- American STD Association membership information
- International Society for Sexually Transmitted Diseases Research (ISSTDR)
Other resources
- Up-to-date information on point-of-care diagnostic tests for STIs
- Publications from the UK Parliament Health and Social Care Committee's Sexual Health Inquiry
- Public Health England (PHE) has an ongoing Sexual Health Campaign. A range of resources are available on the PHE Campaign Resource Centre
- US Center for Disease Control and Prevention (CDC) training slides for STDs
Newsletter
Want the latest news in STIRIG? Internal and external colleagues are invited to subscribe to our newsletter mailing list. Each issue spotlights our research on sexually transmitted infection, and brings you the latest STI-related research, news, events and publications. You can also read the newsletter online (current and previous issues).
Subscribe to our newsletter mailing list
Membership
Subscribe to our membership list (LSHTM staff and students only)
If you are a staff member or a student at LSHTM why not become a member of STIRIG via SYMPA? You can:
- join and collaborate with a group of STI researchers from different disciplines at LSHTM
- raise the profile of your research on the STIRIG website, newsletter and Twitter feed
- access other members with specific expertise to improve the quality of proposals
- hear about conferences, publications, funding opportunities, resources and changes in STI guidelines
- Please ensure you subscribe to both lists!
Privacy notice
Why subscribe to our mailing lists?
Subscribe to our mailing list for the latest updates from the STIRIG including:
- Exciting STI-related research news
- Seminars, events and networking opportunity listings
- New publications
- Activities
- Opportunities and jobs
- Short courses
What emails will you receive?
You will receive a newsletter every two months and occasional update emails on key upcoming events, publications, major stories etc.
Terms and conditions
You can unsubscribe from the mailing list at any time. Every communication we send out includes information on how to do so.
For more information on how we use your data, please see our privacy notice for mailing list recipients. There is also further information on our approach to privacy and security on our Data Protection pages.
Every year we recruit two to three STIRIG student reps to help develop our student community and ensure that student views and experiences are incorporated into our work – championing the next generation of STI and HIV researchers is one of our core objectives. Student reps work closely with our co-directors on the following:
• Identifying key areas of interest for STIRIG seminars and helping to organize
• Suggesting themes and co-producing at least two newsletters
• Developing student specific activities e.g. journal clubs, feedback sessions, blog-writing
• Communicating STIRIG activities to networks and other students
Student reps are recruited at the start of each academic year, and details are available at the student welcome fair and posted on the updates page of our website.
STIRIG students share their work and tips below
- Omar Chidiac
-
Thesis title
"Epidemiology of Neisseria gonorrhoeae in Europe: A systematic review, meta-analysis, and meta-regression"Overview
Neisseria gonorrhoeae (NG) is a major cause of serious reproductive health sequelae worldwide. Knowing its prevalence and incidence can help target interventional programs for key populations such as sex workers, men who have sex with men (MSM), and sexual contacts. The overarching aim of this study was to comprehensively characterize the epidemiology of gonorrhea across Europe. This entailed systematically reviewing prevalence and incidence studies of gonorrhoea aimed by estimating pooled mean prevalence by anatomical site, population type, and assay used, and by identifying possible predictors of gonorrhea prevalence and between-study heterogeneity.Top tip
To start, you must really know what interests you. As you outline your project, it is important to get appropriate guidance from your supervisor and experts in the field. It is very important to write as you go, highlighting key statements you encounter, which will prove to be useful at the end of your project when writing the discussion part.MSc course
Infectious Diseases (DL)Year of course
2021How did you identify your project? (e.g. Did you approach your supervisor with an idea? Did you select it from a list?)
I approached my supervisor with a deep interest to carry out an epidemiological study on sexually transmitted infections (STIs). My supervisor helped me pick a project that I would be able to finish in a one-year timeframe.What are you doing now?
I am currently working at the Infectious Diseases Epidemiology Group temporarily until I travel to pursue my Ph.D. in Epidemiology with a focus on Infectious Diseases.How has your project helped your post-MSc life?
My work experience was focused on the genetic and epigenetic aspects of diabetes and its complications. With an aim to transition to a field of research I am passionate about, I enrolled in this MSc Infectious Diseases in 2018. This program allowed me to develop my knowledge in the biology and epidemiology of infectious diseases and prepared me to go for higher education and pursue my Ph.D. in this field.
- Motoyuki Tsuboi
-
Thesis title
"Prevalence of syphilis among men who have sex with men: a global systematic review and meta-analysis from 2000-20"Overview
The WHO Global Health Sector Strategy aims to reduce worldwide syphilis incidence by 90% between 2018 and 2030. To achieve this goal, interventions that target high-burden groups, including men who have sex with men (MSM), will be required. However, there are no global prevalence estimates of syphilis among MSM to serve as a baseline for monitoring or modelling disease burden. We therefore aimed to assess the global prevalence of syphilis among MSM using the available literature.In this global systematic review and meta-analysis, we searched MEDLINE, EMBASE, LILACS, and AIM databases, and Integrated Bio-Behavioral Surveillance (IBBS) reports to identify syphilis point prevalence data between Jan 2000 and Feb 2020 among MSM who were tested by biological assay. We used random-effects models to generate pooled prevalence estimates across the eight regions of the Sustainable Development Goals (SDGs). We calculated risk of study bias based on Appraisal tool for Cross-Sectional Studies, and stratified results based on low versus high risk of bias. This study was registered with PROSPERO (CRD42019144594).
We received 4,339 records, 228 IBBS reports, and 10 articles from other sources. Of these, 345 prevalence data points from 275 studies across 77 countries were included. The global syphilis prevalence among MSM between 2000 and 2020 is 7.5% (95% CI 7.0-8.5), ranging from 1.9% (95% CI 1.0-3.1) in Australia and New Zealand to 10.6% (95% CI 8.5-12.9) in Latin America and the Caribbean.
Our findings presented the global syphilis prevalence among MSM between 2000 and 2020 is alarmingly high. Achieving the goal of reducing global syphilis incidence by 90% by 2030 will require sustained commitment to interventions that can accelerate syphilis prevention, screening, and treatment in this population.
Top tip
First of all, clear objectives and feasibility of study plan are the most important because of the limited time for summer project. Since I conducted this study as a team in collaboration with other master students for second review, frequent and regular communications with other students and our supervisor was also essential and valuable to share our visions and clarify any questions with each other. Considering the high burden of systematic review and meta-analyses, I believe a goal of your project is not submission as a summer project. If possible, it should be publication on academic journals which is also meaningful for your career in global health.MSc course
Tropical Medicine and International HealthYear of course
2018/2019What are you doing now?
I am now working as a medical officer at National Center for Global Health and Medicine in Tokyo, Japan. Because of my background, infectious disease clinician, I have participated in various sorts of COVID-19 responses including health check-up for charter flight returnee, response to outbreaks on cruise ships, and management of accommodation facilities for COVID-19 patients with mild or no symptoms. What I learned during the master course, such as epidemiology, statistical methods, and infectious disease control, was quite helpful. I am also trying to contribute to global health in the field of infectious diseases consistently.How has your project helped your post-MSc life?
Through this project, I have learned a lot, including practical methods for systematic review & meta-analysis and many advantages of work in a study team from multiple organisations. Also, I reconfirmed the importance of discussions among different professionals. I believe this wonderful experience helps me grow as a global health specialist.
- Sarah Fortna
-
Thesis title
"Barriers and solutions to the scale-up of curable STI management: Perspectives of pregnant women, healthcare providers, and policymakers in Mwanza, Tanzania"Overview
Pregnant women and their babies are among those most vulnerable to STI/RTI complications. The goal of this project was to identify barriers and solutions to antenatal care access and participation, especially in regard to STI testing and care. Focus group discussions with pregnant women and in-depth interviews with pregnant women, healthcare providers, and policymakers took place prior to my joining the project. I was lucky to spend time in Mwanza, Tanzania, where I worked to identify trends at the individual, sociocultural, environmental, and health systems levels which contribute to the current state of care and associated recommendations for improvement. My colleague ran a project parallel to this, using the interview responses to identify barriers and solutions to malaria care in pregnancy.Top tip
Identify a supportive supervisor and a project you are really interested in/passionate about.MSc course
Control of Infectious DiseasesYear of course
2018What are you doing now?
I'm a second year medical student in the United States.How has your project helped your post-MSc life?
I plan to specialise as an infectious diseases physician.
- Ellie Clarke
-
Thesis title
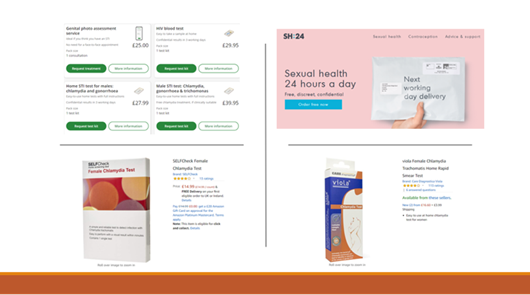
"Online tests for STIs, friend or foe? A scoping review and analysis of providers"Overview
My project was an analysis of STI tests available to order online, that users complete themselves at home. These are an increasingly popular option, however the standard of tests and the quality of care provided can vary. I conducted a scoping review, to map the literature available for STIs, as well as gathering information on online tests available in the UK. I sent questionnaires to providers, collated information from websites and compared it to national guidelines. The results showed that although there is a lot of literature and providers, care is often substandard and test quality may not be sufficient. This project let me explore an interest in STIs whilst learning skills such as literature reviewing, and I really enjoyed working on such a relevant and important topic.Top tip
Be open to projects that are outside of your comfort zone – you will learn some really helpful skills. Also, write as you go! Will definitely make it less stressful at the end.MSc course
Control of Infectious DiseasesYear of course
2019Screenshot of a presentation given after graduating. Contains pictures of different providers of online tests
What are you doing now?
Now I am a vaccine tracking officer with Public Health England collating data on Flu and Covid vaccination uptake.How has your project helped your post-MSc life?
Although not directly related to my current role, completing my project gave me a wide variety of academic skills and exposure to a new field within public health. Also, I have been able to continue work on the topic after graduating from LSHTM which has been good to bring more attention to the issue and also network with others in the field.
- Hester Allen
-
Thesis title
"Analysis of the link between antiretroviral therapy and syphilis in MSM in England 2008-2017"Overview
The aim of my project was to explore the hypothesis that there was an immunological link between the use of antiretroviral therapy (ARV) for HIV and the incidence of syphilis among men who have sex with men (MSM), following a resurgence in syphilis in the UK among MSM in the last two decades. Considerable emphasis has also been put on antiretroviral (ARV) therapy causing changes in sexual behaviour amongst MSM, particularly increasing risky sexual behaviour. To explore this, I obtained an honorary contract with the HIV/STI teams at Public Health England (PHE) and carried out an analysis of STI and HIV surveillance data held by PHE. Using matched HIV and STI data to identify STI diagnoses among MSM diagnosed with HIV, I carried out a multivariable random effects poisson model to look at the incidence of syphilis compared to gonorrhoea and chlamydia during periods when individuals were on and off ARV treatment, adjusting for demographic factors and a proxy measure for high risk sexual behaviour. The results showed that there was no evidence of an increased risk of syphilis in MSM receiving ART and high-risk sexual behaviour markers were the main risk factors for syphilis. This project let me learn more about syphilis and STIs in general, which have always interested me and to understand how surveillance data is collected and can be used and this is an area I still work in. I really enjoyed working on such a relevant and important topic.
https://sti.bmj.com/content/early/2020/11/10/sextrans-2020-054603Top tip
Be open to projects that involve skills that you don’t feel you are very strong at – I had very little STATA and analytical experience before this project and really enjoyed learning these skills while carrying it out. Keep regular communication with your supervisor throughout and persevere with writing the project up for publication once you have finished.MSc course
Public Health general streamYear of course
2017Here is a presentation of my summer project findings I gave at the joint British association of HIV and STI and British HIV association annual conference 2018 in Edinburgh.
What are you doing now?
After my MSc I joined the HIV/STI team at Public Health England as a scientist working on the surveillance of antimicrobial resistant gonorrhoea and STI outbreak investigation. I now work as a Principal Epidemiological scientist in the PHE COVID-19 Epidemiology cell, part of the National COVID-19 Response Centre where I work on the surveillance of COVID-19 associated mortality and post-acute outcomes of COVID-19.How has your project helped your post-MSc life?
My project has helped my career immensely, it gave me hands on experience of working with national surveillance data and gave me the opportunity to carry out novel epidemiological analysis independently. It also gave me the opportunity to experience working within a public health body and understand more about the work that goes on in these organisations.
- Ajay Rangara
-
Thesis title
"Evaluation of VIA, HPV DNA, careHPV and Cervical Cytology as primary screening methods for HPV detection & prevention of cervical cancer in Ghana: which is more cost-effective?"Overview
The study was a primary ingredients-based cost analysis and cost effectiveness evaluation of different HPV-DNA testing technologies that could be used as a primary screening test to screen for high-risk HPV infections. It compared VIA, PAP smear, care-HPV, Gene Xpert and Quantitative DNA sequencing tests. A decision tree was constructed in TreeAge Pro Healthcare software that modelled the implementation pathway of different tests in the Ghanaian health system. The costs that informed the analysis was collected from five health sites in Ghana, including a tertiary care hospital, primary care center and mobile health clinic. Key probabilities were obtained from a targeted literature review search and several stakeholder interviews were conducted to obtain specific insights into challenges in Ghana. The modelling exercise identified GeneXpert as a potential future candidate for primary screening, although VIA is very cheap it has unacceptably low sensitivity and variability, which is widely used in many LMICs.Top tip
Setting out clear objectives with your supervisor, making sure you and them share the same vision and think how the outcome of your thesis will affect your career in the future; and that it is important to take calculated risks – such as travelling to a country to conduct a study – which will give you tremendous insights that you would lose out on if you were doing a systematic review or secondary data analysis. But ultimately, the decision rests with how you see your thesis shaping the start of your career in public health.
- Bronwyn Neufeld
-
Thesis title
Investigating the Relationship between Female Genital Schistosomiasis and Sexually Transmitted Infections in Zambian Women Using Field-Applicable Diagnostic Assays.
Overview
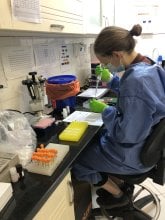
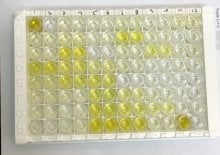
Female genital schistosomiasis (FGS) is a neglected parasitic disease resulting from infection with Schistosoma haematobium. Women with FGS have been found to be at greater risk of STIs including HIV, HPV and Trichomonas vaginalis (TV), though little is understood about precise interactions. Data on coinfection of FGS and STIs is limited in Zambia, and therefore there is a need for larger scale prevalence surveys using field appropriate diagnostic tools. My project was nested in the Zipime Weka Schista study in Zambia (https://www.lshtm.ac.uk/research/centres-projects-groups/zipime-weka-schista) and involved using field-applicable diagnostic assays to determine the prevalence of FGS and seroprevalence of Schistosoma across two communities in Zambia, as well as investigating any associations with STIs (HIV, HPV and TV). Findings included a higher observed prevalence of high-risk HPV in women with FGS compared to those without, though this association was not found to be statistically significant, demonstrating a need for larger scale longitudinal studies. This project allowed me to combine my interests in parasitology and sexual and reproductive health and gain further experience in both laboratory work and data analysis.
Top tip
You get out of what you put into the summer project – use this time to gain new skills in areas you may not be familiar with, and really dive into your interests. Don’t be afraid to approach potential supervisors who work in your areas of interest with your own ideas rather than selecting a project from a list.
MSc course
Medical Parasitology
Year of course
2021-2022
Me in the lab performing serological testing for Schistosoma.
Example of completed serological test (ELISA) where yellow colour change indicates seropositivity.
Recruitment set up in the field for sample collection.
How did you identify your project? (e.g. Did you approach your supervisor with an idea? Did you select it from a list?)
I approached my supervisor as I was aware of her previous work on FGS, and was hoping to find a project that combined both parasitology and STIs.
What are you doing now?
I am currently working as a technician for the Public Health Agency of Canada at the JC Wilt Infectious Diseases Research Centre, on various sexually transmitted and blood borne infection (STBBI) related projects.
How has your project helped your post-MSc life?
I think my project has helped me immensely in my post-MSc life. On a skills level, I use a lot of the laboratory skills I gained during the project in my current job. I also feel conducting my project allowed me to gain valuable insight into what kind of work I’d like to be engaged in, and feel much more confident in the direction I want my future career to take.
- Marie Williamson
-
Thesis title
Association between phone ownership and STI treatment uptake in youth in Zimbabwe in a community prevalence survey: secondary data analysis of the endline survey of a cluster randomised trial
Overview
My thesis analysed youth diagnosed with STIs using laboratory-based testing from a household-delivered survey of an endline survey of a trial looking at the impact of community-based STI testing and treatment on population STI prevalence in youth in Zimbabwe. Molecular STI testing has the potential to reduce undiagnosed and untreated STIs in low-resource settings where syndromic STI management is standard practice. However, results feedback can be very challenging, particularly in settings without routine follow-up. I analysed the proportion of participants who received treatment and whether mobile phone ownership influenced the outcome using logistic regression and adjusted for potential confounders.
Top tip
Start writing and getting feedback from your supervisor early, particularly the discussion for which the content can be anticipated earlier than you think!
MSc course
Public Health – general stream
Year of course
2021-2022
How did you identify your project? (e.g. Did you approach your supervisor with an idea? Did you select it from a list?)
The project came from the MARCH list and was adapted based on the logistical challenges of laboratory STI diagnostics and data available.
What are you doing now?
I’m back to my day job as a registrar in sexual health and HIV medicine in East London, hopefully bringing fresh energy and new perspectives on sexual health. Alongside clinical work, I am working on a project collaborating with Positive East an HIV NGO to promote holistic care of people living with HIV.
How has your project helped your post-MSc life?
This project helped me grasp epidemiological and statistical concepts that are hard to understand without using real world data that you care about and are interested in! I look at research for treatment decisions and journal clubs with a different eye now. The MSc has given me research skills with which to develop my interest in promoting health equity in marginalised populations in sexual health and HIV.
- Kevin Martin
-
Thesis title
Knowledge, attitudes, and practices of youth towards sexually transmitted infections and STI testing in Harare, Zimbabwe
Overview
Sexually transmitted infections (STIs) such as chlamydia, gonorrhoea, trichomoniasis and syphilis can lead to infertility, pre-term delivery, still birth and an increased risk of transmission of HIV. STIs disproportionately affect those in low income countries, such as Zimbabwe. In settings with limited resources, the World Health Organization recommends “syndromic management” for the management of STIs. This entails providing treatment for most infections that may be the cause of the symptoms or signs that a patient has. However, in addition to treating for infections that may not be present, thus contributing to antimicrobial resistance, this method will also miss individuals with asymptomatic infections. As the majority of STIs are asymptomatic, this is very problematic and contributes to ongoing STI transmission. As a result, there is increasing interest in the use of diagnostic STI tests in these settings.
Of note, young people are particularly susceptible to STIs. In Zimbabwe, youth aged between 15 and 24 comprise 18.9% of the population. Those under 15 make up a further 40.3%. Therefore, failure to appropriately address adolescent health now will lead to significant problems in the future.
I was based in Harare for six weeks, performing a sub-study within the CHIEDZA Trial. CHIEDZA is a cluster randomised trial, aiming to determine the impact of an integrated community-based package of HIV services, sexual and reproductive health services and general health counselling for 16 to 24 year olds. STI testing for chlamydia and gonorrhoea infections were offered as part of this package of services. My aim was to explore the facilitators and barriers to accepting STI testing among Zimbabwean youth. Hopefully, this information will be helpful when STI testing is implemented more widely in the future.
To do this, I conducted interviews and questionnaires across four different sites in Harare. I was made to feel incredibly welcome by the CHIEDZA team, all of whom were extremely committed to providing healthcare to youth. I heard from young people about the challenges they face in accessing sexual health care. This included the associated stigma, costs and frequent lack of knowledge about STIs, which granted me an insight into the likely future barriers to providing STI testing.
I really enjoyed my time in Zimbabwe. In addition to visiting a spectacular country, it enabled me to use the skills I had developed throughout my masters programme. I believe this experience has helped me become a more well-rounded researcher, and I feel better equipped to work in similar settings in the future.
Top tip
Try and build on your thesis, with other outputs like presentations and publications. You will already have put in a lot of work into your thesis, and so you should try and make the most of it! This is especially important if planning a career in academia. Furthermore, if you enjoyed working with your supervisors and want to keep working with them, let them know and see if you can build further on your work.
MSc course
Tropical Medicine & International Health
Year of course
2018/2019
How did you identify your project? (e.g. Did you approach your supervisor with an idea? Did you select it from a list?)
I approached my TMIH MSc group tutor Dr Michael Marks for advice about projects related to STIs. He suggested contacting Professor Rashida Ferrand, who was leading the CHIEDZA trial and which was about to start incorporating STI testing into the intervention. I then developed my project with Dr Marks, Professor Ferrand, and Professor Katharina Kranzer, as my supervisors.
What are you doing now?
I am back in Zimbabwe doing a PhD that builds on my MSc thesis, with the same three supervisors. Between my MSc and my PhD, I continued to work with colleagues in Zimbabwe, to develop further groundwork for my PhD proposal. The aim of my PhD project is to evaluate a strategy of point-of-care testing for STIs including chlamydia, gonorrhoea, trichomoniasis, syphilis, and Hepatitis B with comprehensive case management including partner notification in antenatal settings in Harare Province, Zimbabwe. This will include a mixed methods process evaluation and cost-effectiveness evaluation, to understand acceptability, feasibility, and cost-effectiveness of the testing strategy.
How has your project helped your post-MSc life?
My project has had a huge impact on my post-MSc career and life trajectory. In addition to helping me develop as a researcher, it also introduced me to an incredible team at The Health Research Unit Zimbabwe (THRU ZIM). As a result, I have been able to use my project as a springboard into further research projects and a PhD.
- Lauren Hall
-
Surveillance is a critical component of effective disease control programmes, and during my summer research project I was able to participate in a study evaluating syphilis control and surveillance programming in South-Western Uganda. Undiagnosed and untreated Treponema pallidum infection (the cause of syphilis) during pregnancy risks being transmitted from the mother to her baby resulting in fetal loss, stillbirth and other adverse pregnancy outcomes, such as the baby being born with organ abnormalities known as congenital syphilis. Syphilis is the second leading cause of preventable infant mortality worldwide, despite global recommendations for universal screening programs during pregnancy. Under the stewardship of the World Health Organization (WHO), effective elimination of mother to child transmission (eMTCT) of syphilis (and HIV and hepatitis B) programmes include achieving indicators of 95% syphilis testing at first antenatal visit and 95% of women with positive tests effectively treated with penicillin, so as to bring down the rate of congenital syphilis to less than 50 cases/100,000 live births.
Lauren at the Lukaya Health Centre III, Kalungu District, South West Uganda
The primary aim of the research project that I joined (at the MRC/UVRI & LSHTM Uganda Research Unit) was to evaluate the effectiveness of the introduction of a novel dual HIV and syphilis point-of-care test rolled out at antenatal clinics in achieving the first two indicators of the eMTCT programme. Using a before-and-after evaluation design, I helped collect and analyse data from antenatal clinic patient records of health facilities selected through a two-stage cluster random sampling in two districts in South Western Uganda. We compared the rates of testing, positive reactions and treatment among antenatal clinic attenders (N=2000) in the 9-months before (January 2018-September 2018) and 9-months after (January 2019-present) the introduction of a dual HIV/syphilis test kit instead of separate test kits. We also tracked the possible effect of syphilis screening by looking at maternity records of the same health facilities, documenting potential syphilis attributable birth outcomes and HIV infection rates.
Finally, we collected data on the management of sexually transmitted infections (STI), particularly patients with genital ulcer disease, seen at the clinics to make some inferences about the community burden attributable to syphilis, and the adequacy of treatment offered.
Lake Victoria
My interest in STI research was cultivated prior to my joining the Masters at the London School of Hygiene & Tropical Medicine. By attending the Control of STI module and meetings of the STIRIG group, I learned of current School field research opportunities and of the MRC/UVRI & LSHTM Uganda Research Unit. After the whirlwind of final exams, the rush of participating in primary data collection highlighted the conclusion of my Masters’ experience, applying skills I had developed during my module courses. Arriving in Uganda before commencing data collection and leaving two months later with the research underway, I got the hands-on experience in research, and gained a depth in surveillance research and evaluative strategies in STI global indicators.
After initially meeting with the research team, I settled in at the UVRI (Uganda Virus Research Unit) research center headquarters in Entebbe where the MRC/UVRI & LSHTM Unit is located. After a few short weeks, we headed into rural areas for surveying corresponding health facilities, and I was able to contribute to the field collection activities for the remainder of my two months. Study data collection used Open Data Kit (ODK) software on tablets provided by the Open Research Kits group, and I gained valuable coding experience outside of the analysis for my final project.
The data collection team on their way to collect data in Kalungu District, Uganda. (L-R, Damalie, Lauren, and Allan)
Collecting primary research data during the course may not suit all MSc students, but it constitutes an invaluable experience for those contemplating starting a research career overseas. As a fledgling researcher, I also experienced personal nadir points - like when data collection wasn’t going to schedule or visible health inequity daily. Yet, if my summer project had been too conscripted the inquisitive nature that I developed in Uganda, the project taught me key elements of critical analysis and reasoning, as well as quick thinking and adaptation - all very useful to help develop or adapt a research protocol to answer unexplored questions in the field. The summer project allowed me to develop independent reasoning while participating in a cohesive research group at the MRC/UVRI & LSHTM Uganda unit, which will help me going forward in the future.
Entering data for ODK tablets (L-R, Allan, and Damalie)
Highlights of my summer project included getting to explore the places and people of Uganda. I developed lasting friendships with researchers and health facility workers and got to explore Uganda during my weekends off.
Allan entering data
- Vivian Wan-Cheong Yim
-
Thesis title
“I Have No Idea What to Choose”: A Mixed Methods Study of Parental Decision-making for HPV Vaccination and Vaccine Hesitancy Among Chinese Parents in Chengdu, China
Overview
In China, over 170 women die from cervical malignancy every day. The substantial morbidity and mortality associated with the disease pose a significant threat to the health of reproductive aged women. Despite the introduction of HPV vaccines into the Chinese market in 2016, uptake is low (<3%) among adolescent girls. Vaccine hesitancy, defined as a decision-making process leading to delay or refusal of vaccination despite availability of services is a major reason for low uptake. There is scant literature examining the decision-making process behind parents’ decision to delay HPV vaccination for adolescents, and fewer still looking at this in the Chinese context. This mixed methods study aimed to fill in the gap by exploring how Chinese parents came to the decision to delay HPV vaccination and identifying potential individual and contextual factors of hesitancy using behavioural health theories. Quantitative data was collected using surveys, followed by a qualitative component using focus group discussions and semi-structured interviews. We hope the findings will inform future vaccine promotion and advocacy campaigns.
Top tip
Start as early as possible to give yourself plenty of time to explore possible projects with different supervisors. Starting early will also give you valuable time to deal with any issue that may crop up down the road. If you don’t know where to begin, think of a topic you’ve always been fascinated with or can see yourself working on it in the future. Don’t be afraid to be ambitious! This is the opportunity to step outside of your comfort zone, gain new skills and make mistakes under a controlled, supervised environment.
How did you identify your project?
I was interested in the control of STIs, especially HPV and cervical cancer prevention. To collate a list of potential supervisors, I looked at the list of existing projects posted by STIRIG and past projects of interest in the library, then reached out to them for an in-depth conversation about my research interests and goals. One supervisor connected me to my current supervisor and her research team because their work aligned with my interests, and I knew I wanted to be a part of the work they were doing.
What are you doing now?
I am currently working as a medical doctor (OBGYN) in Hong Kong.
How has your project helped your post-MSc life?
Previously I had no experience in either qualitative or mixed methods approaches, so this Project definitely expanded my research skills set. This research topic has also been one of significant interest to me for a long time, and it has been a pleasure to collaborate with a wonderful team who is as passionate about the topic as I am. We’re currently in the process of preparing the manuscript for submission. Finally, this Project offered a valuable glimpse into the world of academia.


































![[WEBINAR] HIV: Diverse challenges among children and women in Asia and Africa](/sites/default/files/styles/event_listing/public/HIV_%20Diverse%20challenges%20among%20children%20and%20women%20in%20Asia%20and%20Africa%20%283%29.png?itok=V1sipAqn)