Umoya omuhle team present preliminary results including context, methods and key findings of the project to date.
A collection of resources relating to TB infection prevention and control, ranging from international guidelines to research papers.
Umoya omuhle is a three-year study that began in 2017 and uses a whole systems approach to look at infection prevention and control for drug-resistant tuberculosis in clinical settings of South Africa in an era of decentralised care. The name, Umoya omuhle, means good air in Zulu, and embodies the project vision of bringing a ‘breath of fresh air' to current thinking on infection prevention and control.
Umoya omuhle is a collaborative partnership between institutions in the United Kingdom and South Africa and involves people from many different research backgrounds and specialities.
The project is organised around a set of seven research questions looking at various aspects of TB infection prevention and control in healthcare facilities, with an aim to improve it.
Umoya omuhle: Infection prevention and control for drug-resistant tuberculosis in South Africa in the era of decentralised care: A whole systems approach
Umoya omuhle is a three-year study that began in 2017, and looks into the transmission of drug-resistant tuberculosis (DR-TB) in South African clinics. The name, Umoya omuhle, means good air in Zulu, and embodies the project vision of bringing a ‘breath of fresh air' to current thinking on infection prevention and control.
South Africa has one of the highest burdens of DR-TB, with more than 19,000 people diagnosed in 2016 according to WHO. Since 2011, its management has been increasingly decentralised to primary healthcare clinics.
Transmission of the disease happens in hospitals and clinics in South Africa, but no one knows how much clinical exposure contributes to this. What is known is that it is difficult to achieve and maintain implementation of existing guidelines for airborne infection prevention and control in health facilities. The physical design of clinics, organisation of care pathways inside the clinic, and the way health workers perceive the risks of tuberculosis may contribute to this.
Download a summary of our project here.
- Aims
-
Our programme takes a whole systems approach to develop interventions to interrupt DR-TB in primary healthcare facilities in South Africa.
This interdisciplinary project will look at the social, biological, and infrastructural dynamics of DR-TB transmission, and the implementation of infection prevention and control in clinics in the provinces of Western Cape and KwaZulu-Natal, South Africa. It aims to inform, develop, and project the potential impact of health systems intervention in facilities in these areas.
- Approach
-
The project approach sees the clinic as a dynamic site of interactions between policies, practices, and patients. We will focus on four areas of research to get a full picture of the environment that they operate in, including:
- Policy analysis to investigate how policies on infection and prevention control for DR-TB have evolved and are practiced in primary healthcare clinics
- Epidemiological studies to assess how much transmission in these clinics contributes to the existence of DR-TB at the community level
- Spatial mapping, workflow and infrastructural assessments to examine the role of clinic design, organisation of DR-TB transmission and general care and working practices that inhibit or foster infection and prevention control
- Ethnographic research to elucidate health worker and patient ideas about risk and responsibility
Mathematical and economic modelling can inform the design of interventions to reduce the risk of transmission of infections within health facilities by exploring the potential impact and cost-effectiveness of an intervention aiming to reduce the risk of transmission.
These models critically depend on the accuracy of assumptions about key parameters affecting transmission risk. Parameters include the number of contacts made per visit, the probability that a clinic attendee is infectious, and the probability that contact results in transmission, which for an airborne pathogen will depend on variables including proximity, contact duration and rate of air change. In turn, the parameters are driven by the movement of people within clinics, and therefore how clinics organize their appointments and manage queues/outpatient waiting areas.
- Outputs
-
Planned outputs for this research include the design of a health systems intervention package that reduces the transmission of DR-TB within healthcare clinics in South Africa with guidelines on behavioural and organisational changes required, and an assessment of the economic impact of an intervention on the health system, healthcare workers, patients, and the wider community.
- Funding
-
This project contributes to the GCRF challenge areas of ‘Equitable Access to Sustainable Development’ and ‘Good Governance and Social Justice’ by promoting locally appropriate, systems-based approaches to sustainable health and wellbeing for both patients and health workers in South African health facilities.
The funding was awarded under the GCRF Tackling Antimicrobial Resistance: behaviour within and beyond the healthcare setting call. These grants are funded by the Economic and Social Research Council (ESRC) working in partnership with the Department of Health.
The support of the ESRC is gratefully acknowledged.
The project is partly funded by The Antimicrobial Resistance Cross Council Initiative supported by the seven UK research councils in partnership with other funders.
Umoya omuhle is a collaborative research project between institutions in the UK and South Africa.
Umoya omuhle inaugural meeting - November 2017, Durban, South Africa. L-R: Karina Kielmann, Hayley MacGregor, Ipeleng Sehunelo, Alvera Swartz, Anna Voce, Alison Swartz, Lindiwe Mvusi, Alison Grant, Anna Vassall, Tom Yates, Jacqui Ngozo, Kathy Baisley, Nicky McCreesh, Indira Govender
Alison Grant (LSHTM, Africa Health Research Institute [AHRI]) is the principal investigator and a clinical epidemiologist. She initially trained as an infectious diseases physician, and has worked for over 20 years on projects aiming to improve care for people with HIV in South Africa, and particularly TB prevention and treatment.
Karina Kielmann (Queen Margaret University [QMU]) is the co-principal investigator, and a medical anthropologist with training in anthropology and public health. She has 15 years of experience of applying social science theory and methods to global health issues, in particular strengthening of health systems for tuberculosis and HIV care.
Kathy Baisley (LSHTM, AHRI) is a statistician. Her research interests include the epidemiology of HIV and other sexually transmitted infections in sub-Saharan Africa, with a focus on design and analysis of intervention trials.
Fiametta Bozzani (LSHTM) is a health economist. Her work is mainly in the area of economic evaluation, with a practical focus on supporting decision-making on resource allocation in low- and middle-income countries.
Adrienne Burrough (LSHTM) is the project financial and administrative manager with experience in administering and managing both overseas and UK projects and writing funding proposals.
Chris Colvin (University of Cape Town [UCT]) is a medical anthropologist. His research interests include the interface between communities and health systems in the context of HIV/AIDS, TB and maternal and child health.
Idriss Kallon (UCT) is a social scientist. His background is in social and health science; sociology and public health, and his research is on continuity of care for patients diagnosed with TB referred from hospitals in South Africa.
Aaron Karat (LSHTM) is a TB epidemiologist. His research interests include clinical and health systems interventions to reduce morbidity and mortality in people with HIV and/or TB and methods used to estimate mortality in resource-limited settings.
Hannah Keal (AHRI) is a communications manager. Her interests are in science communication and public engagement.
Indira Govender (LSHTM) is a clinical research fellow. She is a public health medicine specialist based in South Africa with clinical, management and research experience.
Rein Houben (LSHTM) is an epidemiologist and mathematical modeller. His focus is on applying mathematical models to address academic questions, inform policy decisions and enable capacity building. His academic research focuses on latent infection and socio-economic determinants.
Claire McLellan (QMU) is an institute officer. Her interests are in higher education communications, particularly around research project dissemination.
Nicky McCreesh (LSHTM) is a mathematical modeller. Her research looks at how spatial data can improve TB care and control intervention impact, and how contact data can be used to understand potential transmission sites and inform infection control interventions.
Hayley MacGregor (Institute of Development Studies) is a medical anthropologist. Originally trained as a doctor in South Africa, her research interests include poverty and illness/disability, citizen mobilisation in health provisioning, and ethnography of biomedical research and health technologies.
Alex Pym (AHRI) initially trained as a physician, before conducing the first clinical trials ever for MDR-TB. In 2011, he established a lab in KwaZulu-Natal focused on mechanisms of antibiotic resistance and tolerance in M. tuberculosis, which he currently runs.
Janet Seeley (LSHTM, AHRI) is a social anthropologist. Her research interests are the social aspects of health, particularly HIV across the life course and impact on communities, lives and livelihoods, as well as poverty, social protection, mobility and migration.
Alison Swartz (UCT) is a social scientist trained in social anthropology and public health. Her research has focused on community health workers, the synthesis of qualitative data for qualitative systematic reviews and more recently, youth, gender identity and sexual partnerships.
Anna Vassall (LSHTM) is a health economist. Her research interests are in the priority setting and economic evaluation for HIV, TB and sexual reproductive health, as well as 'real world' evaluation methods.
Anna Voce (University of KwaZulu-Natal) is a public health practitioner. Her research interests are in the public health aspects of reproductive and maternal health, in health systems strengthening, and in health system leadership, particularly in South Africa.
Richard White (LSHTM) a mathematical modeller. He leads the TB Modelling Group and is Director of the TB Modelling and Analysis Consortium. His research focus is the mathematical and statistical modelling of the transmission and control of infectious diseases, particularly TB and HIV.
Tom Yates (University College London) is a clinician and epidemiologist. His research focuses on the transmission of Mycobacterium tuberculosis in high burden settings.
Gimenne Zwama (QMU) is a social scientist. She has 5 years of experience conducting action research in low- and middle-income countries, mostly in South Africa, particularly on increasing health care accessibility for marginalised communities.
Umoya omuhle is organised into a set of seven research questions around TB infection prevention and control.
- Describe the policy and systems context.
- Estimate the contribution of healthcare facilities in DR-TB transmission.
- Examine the effect of clinic design and working practices.
- Understand healthcare workers perceptions of risk and responsibility.
- Design whole-systems interventions to improve TB infection prevention and control.
- Use mathematical modelling to look at the effect of possible interventions on transmission.
- Estimate the costs and economic impact of proposed interventions.
Key terms
RQ: Research question
DR-TB: Drug-resistant tuberculosis
IPC: Infection prevention and control
HCW: Healthcare worker
Project summary document
A summary of the results of the Umoya omuhle project, written for staff at the clinics where the work was done. The summary includes our work to understand why TB is transmitted within clinics and what can be done to reduce transmission.
Preliminary results
A summary look at the preliminary results from the Umoya omuhle project, as of March 2021.
Research Brief
A digestible summary of how system dynamics modelling is used to understand the drivers of TB transmission in primary healthcare clinics
"How to reduce TB transmission in health clinics and public spaces" infographic
A poster-style infographic to show the most effective ways to reduce TB transmission in health clinics and public spaces including post offices and banks.
Download the infographic for free.
Workshop report: measuring and modifying patient flow and waiting times in South African primary health care clinics.
This report summarises the findings of a participatory workshop to share knowledge and to develop methods to measure and modify patient flow in South African primary health care (PHC) clinics. Held in August 2019 in KwaZulu-Natal, South Africa, the workshop was part of the Umoya omuhle study, a multidisciplinary initiative funded by the Economic and Social Research Council (ESRC) of the United Kingdom (UK), taking a whole systems approach to tuberculosis (TB) infection prevention and control (IPC) in South African PHC clinics.
Why we need randomized controlled trials (RCTs) to find the best ways to treat COVID-19
By Indira Govender
In epidemics, our health facilities can become hotspots. Here’s what to do about it
By Indira Govender, Karina Kielmann & Alison Grant.
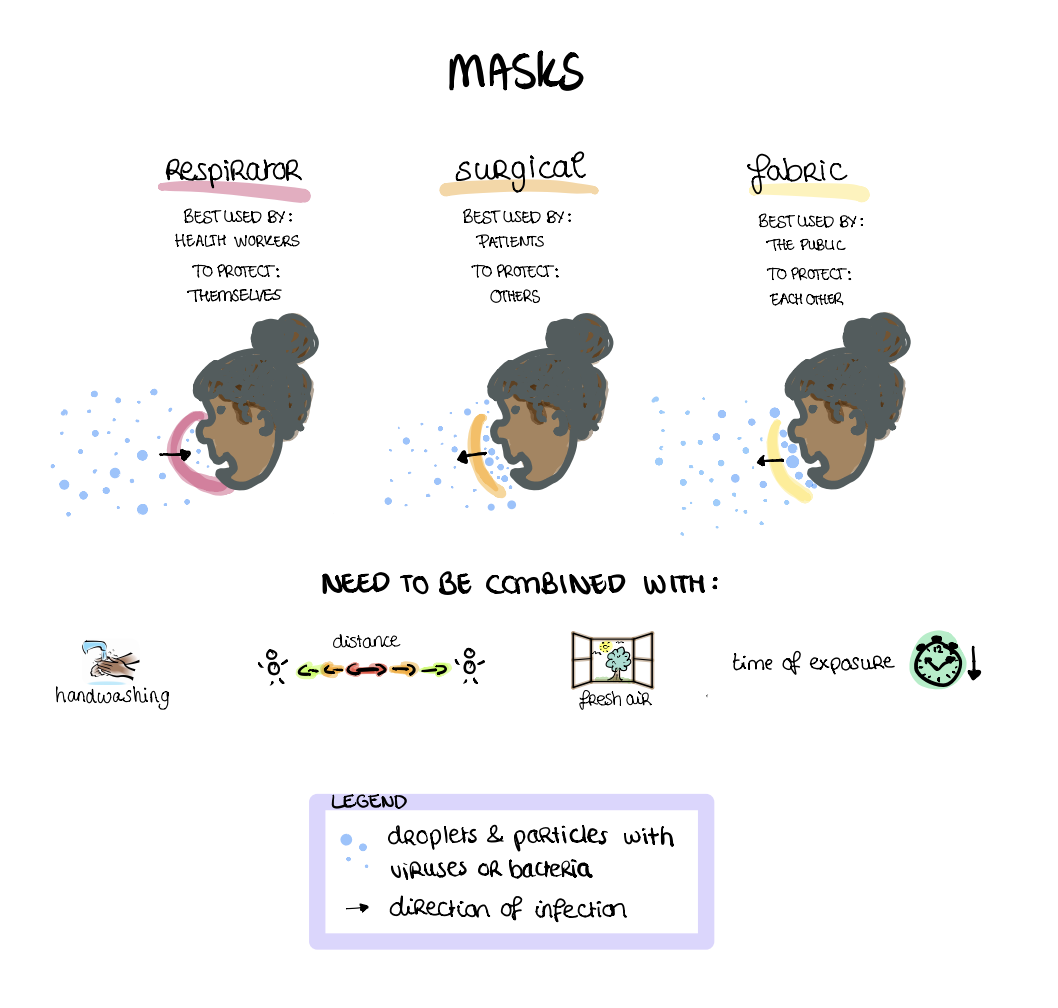
"Face masks: How do they work?"
Infectious diseases like TB and COVID-19 travel through the air via variously sized droplets and particles. Masks filter the air in different ways to offer various forms of protection from infectious diseases.
Newsletters
Find relevant literature on whole systems approaches to infection prevention and control for drug-resistant tuberculosis in South Africa in the era of decentralised care:
2019
January newsletter
March newsletter
2018
March newsletter
April newsletter
May newsletter
June newsletter
July & August newsletter
September newsletter
Poster Summary
To answer this question, we analysed the Ideal Clinic Initiative Framework, tuberculosis infection prevention and control guidelines and our clinic ethnography data of four selected primary health care facilities in KwaZulu-Natal, South Africa. Find out what opportunities and challenges the implementation of health system reform can bring for the prevention and control of TB at South African primary health care facilities. Presented by Gimenne Zwama at the 6th Global Symposium on Health Systems Research.
By Gimenne Zwama
World Bank photo
It is sometimes hard to imagine life before the COVID-19 pandemic. More than a year ago, we were driving across the beautifully lush South African province of KwaZulu-Natal to visit different health facilities. For our research project Umoya Omuhle, which translates to “good air” from isiZulu, we were interested in improving ways to prevent the bacteria that cause TB from being transmitted through the air at health facilities. At that time, conversations about infection prevention and control measures were not trending as they are today. However, the World Health Organization had already long-established recommendations for ways to prevent the transmission of TB in health facilities. One of which you will certainly have become familiar with: wearing a mask.
During the first three days we spent at each of the six primary health care facilities, it quickly became clear that wearing a surgical mask (for patients) or respirator (for health care workers) was the exception, not the rule. When asked, health care workers often became slightly embarrassed. They know that they are supposed to wear a respirator to protect themselves, but find them suffocating and unbearable to wear in hot temperatures (to which you may be able to relate to by now). There is also stigma among patients and staff towards surgical masks and respirators, particularly if they are only worn by one or a few patients and staff members. An added problem is that the effective use of respirators requires trying on different shapes and sizes through “fit-testing”, but none of the facilities we visited had the capability to do this.
If, at this time, you would have told us that a year later masks would become a familiar sight on the streets and even an appealing source of revenue to the retail industries, we would have been very surprised. To date, a quick Google search shows that the estimated global COVID-19 death toll has surpassed half a million over a 7-month period (though likely to be an underestimate). Strikingly, 1.5 million people died from TB in 2018, and this has been a roughly consistent yearly pattern of the past two decades. Could this pandemic be an opportunity for the return of the mask to prevent TB?
But how effective is mask-wearing for TB and COVID-19? The lack of evidence on the effectiveness of masks in filtering the air we breathe has previously limited the ability to implement strict rules around any type of mask wearing. This lack of clarity coupled with the uncomfortable and fidgety experience of wearing a respirator or mask in stuffy, overcrowded clinics has led to problems with mask-wearing. Let’s discuss the current evidence on what we know, and what we don’t know about mask-wearing for disease protection.
We know that TB bacteria and COVID-19 viruses can move through the air via variously sized droplets and particles. TB bacteria are known to spread in small droplets and can hang around and travel in the air, like specs of dust, after being coughed up. The disease spreads when another person breathes them in – this is known as airborne transmission. In contrast, the virus that causes COVID-19 is mostly carried in bigger, heavier droplets, which settle on surfaces and are then transferred from a person’s hands to their mouth, nose, or eyes. However, recent evidence suggests that COVID-19 may be also spread via the airborne route, similar to TB.
Different types of masks can effectively filter the air of most droplets and bigger particles by collecting them on the mask surface when breathing, talking, laughing, singing, coughing or sneezing. We know that respirators, known as N95 or FFP2/3 masks, protect the wearer from breathing in both large and small droplets containing viruses and bacteria. Although they cannot filter all the tiny particles, they are particularly helpful in high-risk healthcare settings. Surgical masks protect other people from the person wearing the mask coughing, sneezing or breathing out bigger droplets. These are therefore best used by patients and are known to halve the risk of spreading TB. Less is known about the effectiveness of fabric or paper masks, and although they work similarly to surgical masks, they are thought to be less protective. They can, however, provide some protection to others if the fabric or paper used is dense, layered and fits snugly onto the face of the wearer. These are therefore best used by the public, those who do not experience any symptoms but may unknowingly be infected and potentially infectious.
In short, we know that none of these masks are 100% perfect in preventing COVID-19 and TB, but wearing something that covers your mouth and nose is likely to reduce the risk of you passing disease to other people. Because the particles and droplets collect on the mask surface, it is crucial to properly and regularly wash your hands to protect yourself, especially immediately before and after you use any type of mask. Physical distancing is another important measure, especially for COVID-19 prevention. Distancing reduces the opportunity to inhale potentially dangerous particles as there is more time for bigger particles to settle on the ground before reaching you. Opening the windows or being outside means that potentially infectious particles are quickly dispersed and are less likely to be inhaled. And, painfully, the less time you spend with others, the less you potentially expose yourself and others.
It is crucial that we continue the conversation on mask-wearing and ‘clear the air’ long after this pandemic. TB is already an existing threat to millions of lives and will continue to burden health systems of many low- and middle-income countries, such as South Africa. The COVID-19 pandemic response gives us an opportunity to establish stronger health systems and practices for sustainable TB prevention, and perhaps change embedded habits around infectious disease control. It’s now time to listen and learn from this pandemic and do our best to protect those most vulnerable to infectious diseases.
More information about fabric masks.
Credit - hand washing cartoon.
Three researchers from Umoya Omuhle feature in LSHTM Viral's podcast, explain the complex links between TB transmission, COVID-19 and the role human behaviour in controlling infectious diseases.
The way people act and behave inside health clinics can impact the spread of infectious diseases like COVID-19, TB and Ebola. Understanding how this happens is essential for effective, long-lasting public health solutions. We speak to Alison Swartz, Aaron Karat and Karina Kielmann who work through a 'systems approach' that includes social science, anthropology and epidemiology in infection prevention control in South Africa.
After presenting her research proposal to a panel of examiners during her upgrading, Chloe will be continuing her exiting research on TB control in South Africa.
Why is this important?
It is becoming increasingly apparent that a wider view of TB control is needed, not only for TB treatment today but for TB management in the future. In particular, studying the historical and anthropological elements to infection prevention and linking this to the space in which TB is controlled and treated. Taking a wide approach to research in this area can also help us to understand government responses to public health crises, such as the South African national epidemics of TB and drug-resistant (DR)-TB, and highlight notable contextual and historical issues that play a part in public health treatment and response.
What will Chloe’s project look at?
Chloe will focus on the rural community setting of Mtubatuba in the South African province of KwaZulu-Natal (KZN) and pay particular attention to the space of the primary care clinic. This work will be attached to Umoya Omuhle, which is based in the Western Cape and KZN provinces. Umoya Omuhle demonstrates a pragmatic approach to the public health problem of TB and Drug resistant-TB and is channelled through the established policy of Infection Prevention Control (IPC).
The specific question Chloe will address is: How do histories of South African TB control, public health systems and spatial realities continue to shape contemporary responses to this disease, especially now in its increasingly drug-resistant state?
Chloe will consider the issue of TB control and study the previous attempts to limit drug-resistance. She will use the concept of ‘infrastructure’ to examine how these dimensions intersect within a primary care clinic in rural KwaZulu-Natal and investigating how histories relate to infrastructure of public health work. To study this, she will use a mixture of ethnographic and historical methods, document collection and analysis, observation, and oral histories.
The Umoya omuhle project held a successful expert workshop on TB transmission in South African primary healthcare facilities from the 6th – 7th August in Durban, South Africa. TB is a key health priority for South Africa. Preventing TB, and drug-resistant TB, transmission in health facilities is essential, but implementation of well-established guidelines to prevent TB transmission in clinics remains suboptimal. The workshop gathered the perspectives of policymakers and practitioners in South Africa using a method called group model building. The process explored the drivers of TB and drug-resistant TB transmission in health facilities to understand the challenges to policy implementation, and participants' views on potential solutions. The workshop outputs will inform development of novel interventions; we will explore the potential impact of these interventions in modelling work over the next year.
Long clinic waiting times are a potential driver of TB transmission. On Thursday 8th August, a workshop on ‘patient flow’ in primary healthcare facilities gathered stakeholders' perspectives concerning methods to measure waiting times, and potential ways to reduce the time patients spend in primary health clinics.
We recently held an expert workshop on TB transmission in South African primary healthcare facilities, gathering perspectives from policymakers and practitioners.
The Umoya omuhle team attended their third investigators' meeting in Ballito, South Africa. The four-day meeting reviewed project progress to date, reviewing qualitative and quantitative data from 12 health care facilities in KwaZulu-Natal and the Western Cape provinces. The investigators also met with the project reference group which included Ms Jacqui Ngozo, Director of TB programmes, KwaZulu-Natal Department of Health; Dr Vanessa Mudaly, a senior medical officer for health programmes at the HAST Directorate in the Western Cape Provincial Government; Professor Helen Schneider, a public health specialist and health systems and policy researcher from the University of the Western Cape and Dr Thiloshini Govender, a public health medicine specialist and occupational health physician at the King Dinuzulu Hospital.
The aim of this meeting was to consider and prioritise, based on evidence obtained to date, possible interventions to reduce transmission of tuberculosis in primary healthcare facilities in South Africa. The project will employ an innovative approach - system dynamics modelling - to engage policymakers and practitioners to identify, design, and prioritise potential interventions at a meeting in August.
[L-R Anna Voce; Gimenne Zwama; Karin Diaconu, Sanj Karat; Idriss Kallon; Jacqui Ngozo; Indira Govender; Hayley MacGregor; Alison Grant; Alison Swartz; Thilo Govender; Tom Yates; Nicky McCreesh; Fiamma Bozzani. Photo: Adrienne Burrough]
Health systems webinar: Applying a ‘whole systems’ approach to infection prevention & control in primary health care clinics in South Africa
Watch the webinar recording.
View the webinar slides.
The Umoya omuhle project team present critical reflections from the project including, understanding complexity, assessing infrastructure, generating evidence through system dynamics modelling and designing whole system interventions.
Preliminary results webinar: Infection prevention and control for DR-TB in South Africa in the era of decentralised care - a whole systems approach
Read the webinar summary document.
Umoya omuhle team present preliminary results including context, methods and key findings of the project to date.