This series is written in partnership with Dr Catherine Wedderburn, a Wellcome Trust Clinical Research Fellow at the London School of Hygiene & Tropical Medicine and the University of Cape Town. On World AIDS Day, we spoke to her about her research in South Africa examining the effects of HIV and antiretroviral therapy exposure in uninfected children born mothers living with HIV.

What is the difference between HIV and AIDS?
HIV (human immunodeficiency virus) is a virus that damages your immune system making it harder to fight everyday infections and disease. It can lead to a condition called AIDS (acquired immunodeficiency syndrome). AIDS develops when HIV has caused serious damage to the body’s immune system.
What is antiretroviral therapy?
Antiretroviral therapy (ART) involves a combination of HIV medicines that are taken daily.
ART is very successful in controlling HIV infection, keeping the virus at extremely low levels in the body. This stops progression of HIV disease and is recommended for everyone who has HIV. ART cannot cure HIV, but regimens are able to keep people living with HIV healthy, prevent progression of the disease, and stop onward transmission.
Is it possible to avoid transmitting HIV from mother to baby?
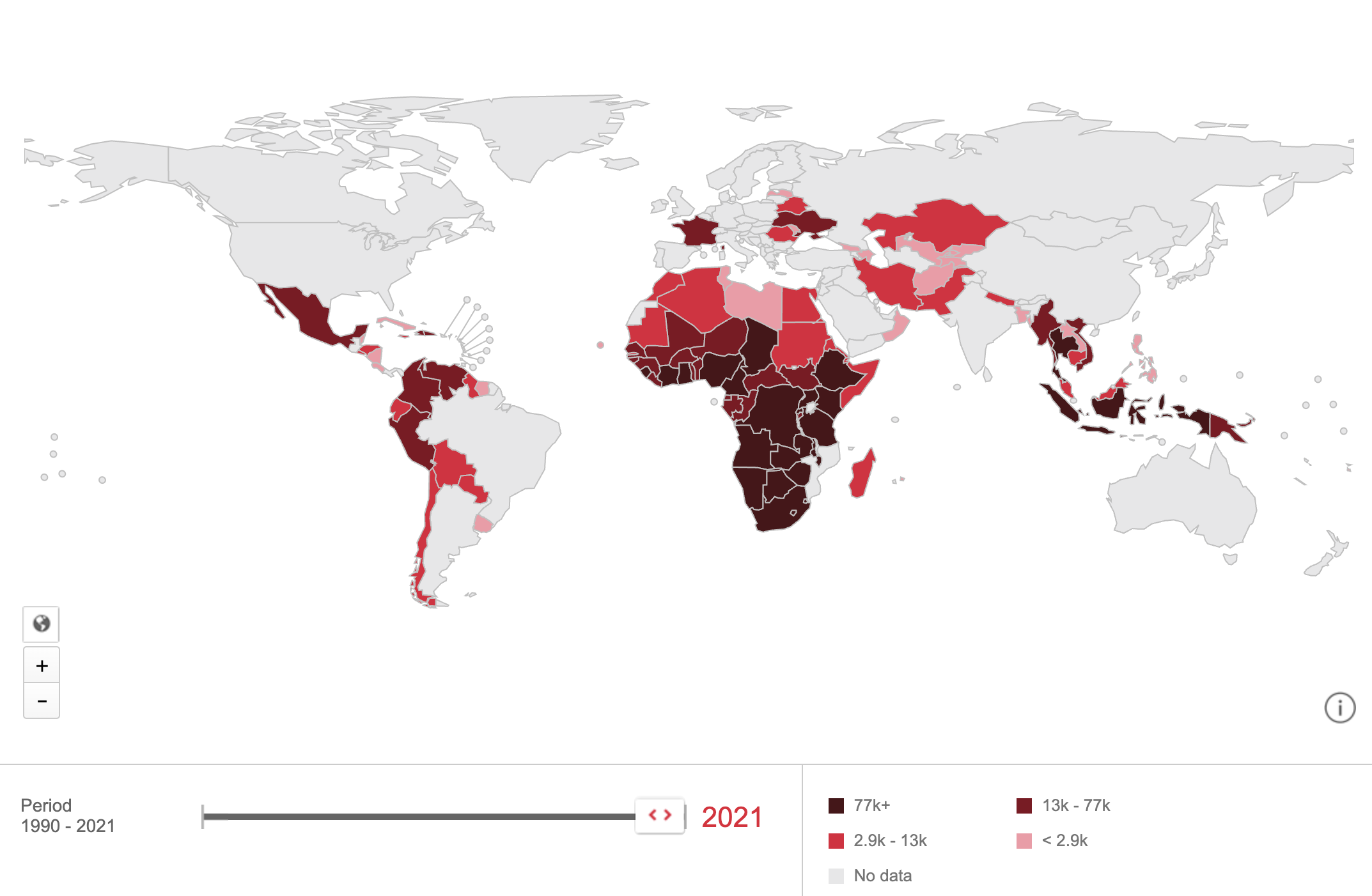
Yes! Every year, more than 1.3 million babies are born to women living with HIV, 90% of whom live in sub-Saharan Africa. Without any interventions, up to 40% of children born to women living with HIV became infected, however, the expanded use of antiretroviral therapy in pregnancy has reduced the risk of vertical transmission by suppressing the virus; with this intervention less than 5% of HIV-exposed children become infected. This is one of the biggest success stories of the HIV epidemic response.
Who are this vulnerable population?
Children who are HIV-exposed and uninfected (HEU) are those who are born to mothers living with HIV but who are not infected themselves. Most of these children are also exposed to antiretroviral drugs in pregnancy and through breastfeeding. Given the continued high numbers of pregnant women living with HIV, this population is growing and there are an estimated 15.9 million HIV-exposed uninfected children worldwide. South Africa has the highest number of children who are HIV-exposed uninfected of any country in the world at 4.1 million (25% of the global HEU population). To put this in context, it means approximately a quarter of all South African children have been exposed to HIV.
Are HIV-exposed children who remain uninfected still affected?
The reduction in vertical transmission of HIV is a huge leap forward for global health. However, being exposed to the virus and medication in utero in any capacity potentially has consequences. Children who are HIV-exposed uninfected have increased illness early in life and are more likely to be hospitalised and die than HIV-unexposed children. In addition, current evidence suggests children who are HIV-exposed uninfected are at risk for adverse growth and developmental outcomes, with the poorest outcomes being reported in low and middle-income countries.
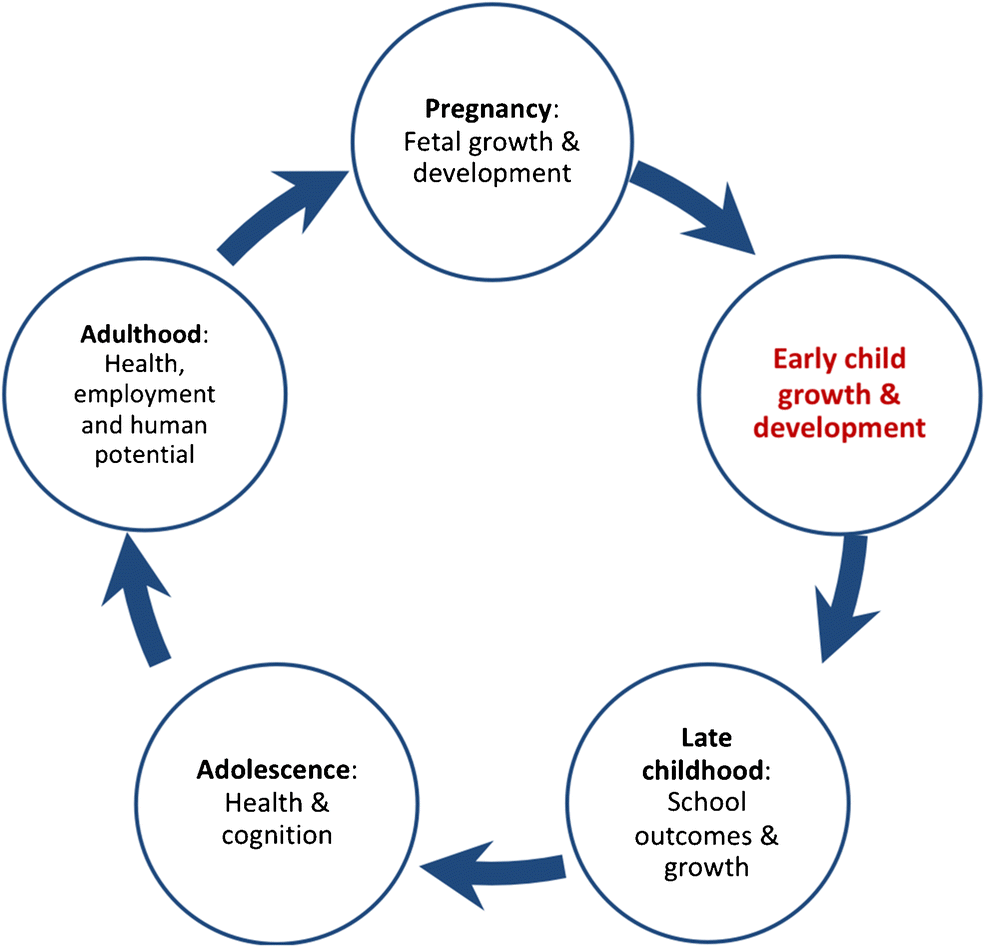
Worldwide, there is a growing focus on ensuring that all children not only survive but thrive and are able to live full lives. With this in mind, it is critical to have a full understanding of the impact of HIV and ART exposure on child development, particularly brain development, so that appropriate and focussed interventions can be put in place to improve child health outcomes. Any early growth or developmental problems may have a long-term impact on later school, employment, and health outcomes.
Why are children who are HIV-exposed and uninfected vulnerable?
The exact mechanism(s) underlying the pathological effects of HIV ‘exposure’ remains an unanswered question. Is it because of HIV exposure to the developing foetus? Is it because the mother’s immune system is influencing neurodevelopment? Is it due to antiretroviral toxicity? Or is it an environmental or psychosocial mechanism?
It is likely that multiple factors come into play, and more work will need to be done to fully understand these associations. Investigating the mechanisms behind impaired development is important to prevent future developmental delay. Research is gradually filling in the gaps to build an understanding of the complex combination of HIV-related variables and illness, ART exposure and side effects, and socioeconomic factors. Some of these areas of research will be explored in subsequent blogs.
What are the next steps?
Strengthening interventions that prevent HIV transmission to both women and their children remains critical. Preventing HIV transmission to women will reduce the number of children born HIV-exposed, and for individual children it is far better to be exposed to HIV than infected with HIV. HIV infection progresses considerably faster in children than adults and targets the neurological system in particular; without ART, 50% of children with HIV will die before their 2nd birthday.
Given the growing population of children who are HIV-exposed uninfected, this group now needs to become a public health priority. Why? Because even a small impact on growth and neurodevelopment in this group would have a large effect on the population of countries with high HIV prevalence, and potentially substantially impact human capital in the future.
Read Catherine and colleagues’ paper Growth and Neurodevelopment of HIV-Exposed Uninfected Children: a Conceptual Framework.
Resources/Further reading
LSHTM's short courses provide opportunities to study specialised topics across a broad range of public and global health fields. From AMR to vaccines, travel medicine to clinical trials, and modelling to malaria, refresh your skills and join one of our short courses today.