To access this blog in French, please click here.
On 3 January 2020, the day after the Minister of Health of Senegal issued guidelines for the proper management of medical emergencies, a woman died while being urgently transported to hospital.
Madeleine Ngom gave birth to twins in the local health post in Sanghé after an uncomplicated labour. Soon after, she started feeling dizzy and bleeding heavily. She needed to be referred urgently to the regional hospital, less than 15 kilometres away in the regional capital of Thiès.
What should have been a simple, quick, and lifesaving journey turned out to be the opposite.
The health post ambulance wasn’t available because the person responsible was away from the facility. Even if it had been available, the family were unable to raise the 10,000 CFA (around £13) needed to make use of it. The local Catholic mission lent their car to transport Madeleine; when this car broke down, she was moved to a second car, but this one also broke down. Shortly after, the car got stuck in traffic as they reached Thiès – without an ambulance siren, they were unable to get through. She passed away before reaching the hospital.
Madeleine’s story isn’t an isolated case, it illustrates many of the challenges faced by women giving birth in rural areas of Senegal. And it highlights an urgent need for change.
Bringing more births into facilities – but are primary care facilities enough?
Access to care during childbirth has expanded over the last few decades in sub-Saharan Africa. In Senegal, the proportion of births taking place in health facilities increased from 47% in 1992 to 80% in 2016. This is an impressive achievement, considering it represents a three-fold increase in the absolute number of births accommodated by an underfunded health system.
Health posts, like the one Madeline gave birth in, are small facilities usually staffed by one nurse and one midwife. Like other countries in sub-Saharan Africa, Senegal has encouraged women to give birth in public, primary care facilities such as these health posts, run by the Ministry of Health. This policy seems to have worked: in Senegal, most of the rise in facility births over the last 25 years was driven by health posts, in which now half of all facility births take place.
But health posts aren’t a perfect solution. Findings from our recent study show that 30% of rural health posts have no midwife, and most health posts are unable to provide the full range of basic emergency obstetric care (such as antibiotics to treat infections). For women who develop complications around the time of birth and need more advanced emergency obstetric care – like caesarean sections or blood transfusion – reaching these primary care facilities is therefore only the first hurdle.
Difficult onward travel to a hospital for women referred with complications is in part due to a shortage of ambulances. Only 62% of health posts are able to use a vehicle on-site or elsewhere (which would take additional time to arrive) – when these are unavailable, women’s families usually have to find informal means of transport (like the local Catholic mission’s car and private car which transported Madeleine). Additionally, travel to the hospital itself can take a long time due to distance, traffic, and poor road conditions.
Mapping the problem
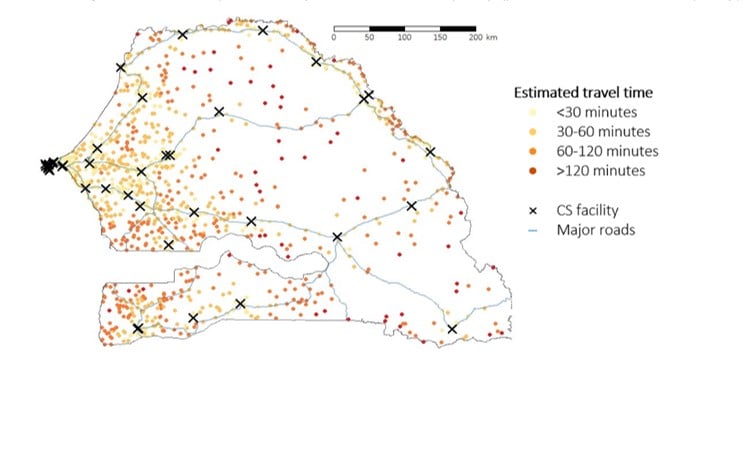
In our study, we wanted to know how long it would take for women who develop childbirth complications in primary care facilities to reach a hospital. We first identified the 40 health facilities in Senegal which were known to perform caesareans as of November 2018. The map below shows these are concentrated in the West of the country, in populated urban centres (represented by the crosses). For example the capital Dakar, the Westernmost peninsula home to 25% of Senegal’s population, had 12 of the 40 facilities with caesarean capacity. In rural regions containing almost half of the population, women face much longer distances to reach a facility with caesarean capacity.
We then used Open Street Map (a programme similar to Google Maps) to identify the minimum travel time from each primary care facility to the closest facility performing caesareans. We found that half of rural primary care facilities are located more than 47 minutes’ driving time away from the nearest caesarean facility, and 37% more than one hour away. The map below shows that primary care facilities in rural regions and those far from major highways have particularly longer travel.
Mapping health services like we have done here can help identify areas where women have poor access to lifesaving care. Addressing this issue is crucial to reducing the disproportionate number of deaths of women and babies during childbirth from these remote, rural areas.
A ticking clock for mothers and babies
Our travel time estimates are best-case scenarios: they do not take into account heavy traffic, slower speeds required at night, or seasonal flooding. They don’t include the time needed to call the ambulance and for the ambulance to arrive, for facilities with no on-site ambulance. No guidelines exist for how long – at most – obstetric referrals between facilities should take, but obstetricians’ associations in the UK and USA recommend a maximum of 30 minutes from diagnosing fetal distress (when the baby is not receiving enough oxygen) to delivering the baby via caesarean. This is an unattainable target for the vast majority of primary care facilities where women give birth in rural Senegal.
In other words - the transport times between health facilities in these areas can be life-threatening for women and their babies.
Rural women, who already travel longer to reach primary care facilities, later also face longer travel times to higher-level facilities if they need surgery or blood transfusions.
"I do not doubt the usefulness of these results, which bring a new perspective to our vision of maternal health in Senegal,” explains Dr Dioukhane, co-author of the study and expert who served as a District Medical Officer for 10 years in two rural regions. “Decentralisation policies put in place by the Ministry of Health have focused on making childbirth services available in rural areas, but without acknowledging differences in contexts between these regions. It is obvious that, to make services truly accessible to communities, infrastructure investments beyond the health system are also needed, in particular in road networks and availability of ambulances.”
People to services or services to people?
What can be done to overcome the challenge of distance in rural Senegal and elsewhere in rural sub-Saharan Africa? Governments can either bring services closer to people, or bring people to services more efficiently. So far, Senegal has chosen the former approach by encouraging women to give birth in primary care facilities such as health posts. However, if these facilities are unable to provide the full range of basic emergency obstetric care, this may not have a big impact on reducing maternal and perinatal mortality. When complications arise, many of these facilities are still too far or too “long” from hospitals for women who need a caesarean or transfusion to reach care on a timely basis.
Several innovative strategies have been tried in other countries to bring people to services (the second approach): maternity waiting homes allow women to stay near hospitals close to their due date to avoid needing to make the journey in an emergency, and ambulance sharing can help cover larger areas with limited resources. High-income countries with large rural areas, such as Canada and Australia, use costly means such as air ambulances, but other lessons might be applicable to African contexts. Whether bringing people to services and services to people, substantial improvements in road networks and ambulance availability are needed.
Addressing the challenge of providing high-quality childbirth care to women living in rural areas will need tailored, region-by-region strategies. Important progress in reducing maternal mortality has taken place in Senegal under the Ministry of Health’s leadership; we must now focus on areas left behind to prevent avoidable deaths like Madeleine’s, and accelerate reductions in maternal and newborn deaths.
Our postgraduate taught courses provide health practitioners, clinicians, policy-makers, scientists and recent graduates with a world-class qualification in public and global health.
If you are coming to LSHTM to study a distance learning programme (PG Cert, PG Dip, MSc or individual modules) starting in 2024, you may be eligible for a 5% discount on your tuition fees.
These fee reduction schemes are available for a limited time only.