Fuelled by its strength and depth in research, education and action, LSHTM’s response to the 2013-2016 Ebola virus outbreak in West Africa helped save lives and control the epidemic. It was ground-breaking in the way it mobilised the global health community to work together for a sustained, long-term and far-reaching impact on disease preparedness. Mathematical modelling experts confirmed the scale of the outbreak and provided crucial evidence about the resources needed to help contain, control and treat the disease, and to prepare for future outbreaks. In an innovative trial, LSHTM researchers showed that a new vaccine was safe and effective, directly informing the World Health Organization’s immunisation strategy recommendations in 2017.
Underpinning research
Ebola virus disease is a viral haemorrhagic fever, with high death rates and significant epidemic potential. The West African Ebola virus epidemic (2013-2016) was the biggest Ebola outbreak in history, and caused major loss of life and disruption in the affected countries (Guinea, Liberia and Sierra Leone). On 8 August 2014, the WHO declared a Public Health Emergency of International Concern (PHEIC). WHO reported a total of 28,646 suspected cases and 11,323 deaths for the epidemic.
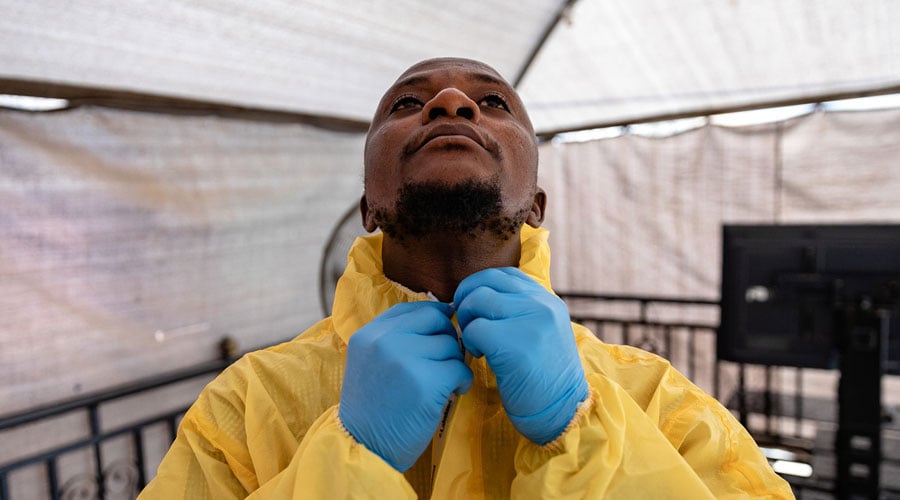
Peter Piot, LSHTM Director since 2010, was part of the original team who discovered the Ebola virus in 1976. In response to the public health emergency declaration, he issued an all-staff call to action, urging LSHTM researchers to offer their skills and knowledge to respond to the devastating epidemic, and stating that ‘an exceptional crisis requires an exceptional response’. As a result, more than 400 academic and professional services staff volunteered to help, and many volunteers were deployed in a wide range of activities via NGOs, WHO and Public Health England.
Modelling to support and inform response planning
During the outbreak, mathematical modellers at LSHTM led by Professor John Edmunds mapped the spread of Ebola to support and inform response planning. The team used a transmission model fitted to the number of weekly Ebola virus cases during August to November 2014 to evaluate the risks and benefits of introducing community care centres (CCCs) in Sierra Leone. These are small facilities (up to 10 beds) within the community run by community health workers, which provide isolation facilities for Ebola patients as an alternative to overburdened Ebola treatment centres. This research found that using CCCs could lead to a reduction in Ebola cases, even if virus transmission occurred between isolating patients and the community. Transmission models demonstrated that CCCs contributed to a 13-22% reduction in the Ebola virus reproduction number. Research in collaboration with UNICEF using focus groups and key informant interviews showed the centres were well accepted by the community.
Modelling to predict the impact of immunisation strategies and trial design
As the worldwide response progressed, modellers at LSHTM sought to predict the impact of different candidate Ebola vaccine immunisation strategies and trial designs. WHO led a trial in Guinea from April to July 2015, with LSHTM and other partners, using an innovative design co-developed by LSHTM, called a ‘ring vaccination’ approach. Based on the method used to eradicate smallpox, it involves vaccinating people in rings of contacts and contacts of contacts of confirmed cases.
This novel, adaptive trial design ensured that sufficient endpoints could be accumulated to test the vaccine despite very low levels of Ebola in Guinea. The Guinea vaccine trial was the only successful Phase 3 trial conducted in West Africa. Rings were initially randomised for adults to receive the vaccine either immediately, or after a 3-week delay. The trial found the experimental vaccine rVSV-ZEBOV developed by Merck was highly protective. Among the 5,837 people who received the vaccine, no Ebola cases were recorded 10 days or more after vaccination. In comparison, there were 23 cases in the same time period among those eligible who did not receive the vaccine. All rings were subsequently offered the vaccine immediately and the trial opened to children over the age of six. A total of around 12,000 people were vaccinated in rings.
Guinea was declared Ebola virus-free in 2016. However, during 2016 there was an additional flare-up of the virus identified in the rural Nzérékoré prefecture of the inland Guinée Forestière region, and the ring vaccination strategy was used again. Further analysis during this outbreak further demonstrated the efficacy and safe implementation of the ring vaccination strategy with rVSV-ZEBOV in rural, resource-limited settings.
Details of the impact
LSHTM’s response to the 2013-2016 West African Ebola epidemic translated expertise into immediate practical and life-saving action. Researchers not only went into the field to help patients, communities and organisations, but also helped contain the spread of Ebola through disease mapping and outbreak analysis. The research benefited international organisations such as WHO, in-country health ministries, UK Aid, and communities affected by Ebola including frontline health workers, by informing resource provision, vaccination strategy and preparation for future outbreaks. This huge mobilisation effort also contributed to sustainable action in the longer term through pioneering education and training programmes and the creation of a new rapid support team.
Shaping the resources needed for Sierra Leone
By demonstrating the effectiveness of Community Care Centres (CCCs) to take the pressure off Ebola treatment centres and reduce the virus transmission, LSHTM research directly underpinned the response in Sierra Leone from 2014 onwards. Modelling the country’s transmission rate of Ebola helped to predict what facilities the country needed and informed the UK Department for International Development (DFID, now FCDO) funding strategy for CCCs. At the request of the government of Sierra Leone and endorsed by the WHO, the UK government committed a £427 million package of direct support to help contain, control and treat Ebola. This strategy was informed by LSHTM research on how and where the outbreak was progressing. It included supporting more than 1,470 treatment and isolation beds in Sierra Leone, including the UK’s six purpose-built Ebola treatment centres.
Safe and effective vaccination strategy
The pioneering ring vaccine trial in Guinea demonstrated that the rVSV-ZEBOV vaccine was safe and effective, strengthening global capacity to fight future outbreaks of Ebola. Following the publication of the trial results in December 2016, Edmunds, Dr Anton Camacho and Professor Adam Kucharski presented evidence to the WHO Strategic Advisory Group of Experts on Immunisation (SAGE) in early 2017. This highlighted ring vaccination as the optimal vaccine delivery strategy for Ebola. The WHO then recommended use of rVSV-ZEBOV via ring vaccination under an expanded access/ compassionate use protocol:
‘Ring vaccination, as used in the Phase 3 study in Guinea, is the recommended delivery strategy. This should be adapted to the social and geographic conditions of the outbreak areas and include people at risk including but not limited to: (i) contacts and contacts of contacts; (ii) local and international health-care and front-line workers in the affected areas and (iii) health-care and front-line workers in areas at risk of expansion of the outbreak.’
Based on this recommendation, the ring vaccination strategy was used against Ebola virus in the 2018-2020 outbreak in the Democratic Republic of the Congo (DRC). Over 290,000 people in the DRC received the Merck-manufactured rVSV-ZEBOV vaccine under the ‘compassionate use’ protocol, as well as health and frontline workers in Uganda, South Sudan, Rwanda and Burundi. Preliminary WHO results indicated that the vaccine administered via the ring strategy was 97.5% effective and reduced the chances of death in those who developed Ebola. In November 2019, the Merck vaccine was licensed by the European Medicines Agency and prequalified by the WHO, making it possible for countries to start their own regulatory processes. It then became available for procurement by UN agencies and The Global Alliance for Vaccines (GAVI). The vaccine was also approved by the US Food & Drug Administration (FDA) in December 2019, citing the Guinea trial as key evidence and commending the study design. In February 2020, four African countries (the DRC, Burundi, Ghana, and Zambia) became the first to license rVSV-ZEBOV. This meant it could be administered without prior clinical trials or research protocols.
Preparing for future outbreaks: the UK Public Health Rapid Support Team (UK-PHRST)
The Ebola crisis highlighted the need for the international community to strengthen its response to and control of disease outbreaks before they develop into a global threat. In 2016, LSHTM was chosen because of its instrumental role in the Ebola response to jointly run the newly established £20 million initiative, the UK-PHRST, in partnership with Public Health England. The PHRST was headed by LSHTM Professor Dan Bausch and in academic partnership with the University of Oxford and King’s College London. UK-PHRST was developed as part of the UK contribution to global health security and to complement the WHO’s work on the Global Health Emergency Workforce. As well as coordinating and hosting the UK-PHRST as it responded to outbreaks, LSHTM members worked to expand the range of scientific expertise used for outbreak control. The UK-PHRST has since been deployed to 11 outbreaks, where the team supported the response by organisations on the ground via technical advice and expertise on outbreak control measures, tracking the progress of diseases, and delivering training. Outbreaks included: Sierra Leone (2017, disease risk reduction following Freetown landslides), Nigeria (2017, meningitis and 2018, Lassa fever), the DRC (2018-19, Ebola virus), Madagascar (2017, pneumonic plague), Bangladesh (2017-18, diphtheria in displaced Rohingya populations), and COVID-19 (2020).
Making an impact through open-access training
LSHTM staff pooled their expertise to create a unique three-week online course to provide a better understanding of the Ebola virus for health professionals, field workers and students. The course, ‘Ebola in Context’, was delivered via the FutureLearn online platform in 2015 and featured LSHTM and other frontline responders in West Africa. More than 24,000 participants from 185 countries joined the course. The course materials are available online for free, open to re-use by educators.
Recognition, awards and press coverage
LSHTM’s extensive Ebola response, including the work of the modelling team, was widely commended. LSHTM was awarded the prestigious Times Higher Education (THE) ‘University of the Year’ award for 2016. The judges were unanimous in their decision, recognising LSHTM’s wide-ranging and life-saving response to the 2014 epidemic. The Guinea vaccine trial was runner-up in Science’s ‘Breakthrough of the Year’ in 2015. Edmunds received an OBE in the 2016 Queen’s New Year Honours list for his services to infectious disease control, particularly the Ebola crisis response in West Africa.