The UK-PHRST, funded by UK aid from the Department of Health and Social Care, supports low- and middle-income countries in investigating and responding to disease outbreaks and conducts research to improve our response to future epidemics.
The UK-PHRST is funded by UK aid from the Department of Health and Social Care and is a partnership between the London School of Hygiene & Tropical Medicine (LSHTM) and the UK Health Security Agency (UKHSA) with contributing academic partners.
About the team
Through the UK Public Health Rapid Support Team (UK-PHRST), the UK has the capacity to respond rapidly to disease outbreaks in low- and middle-income countries around the world and conduct operational research into epidemic preparedness, playing an important role in global health security. The team also works to help countries to build their own capacity for an improved and rapid national response to outbreaks.
The UK-PHRST is funded by UK aid from the Department of Health and Social Care and is a partnership between the London School of Hygiene & Tropical Medicine (LSHTM) and the UK Health Security Agency (UKHSA) with contributing academic partners.
Tackling disease outbreaks at their source at the earliest possible stage helps prevent their spread, saves lives, and is the most effective way to protect the UK. As of March 2021, the team has taken part in just over 20 deployments across more than 10 countries.
Deployable team
The UK-PHRST comprises of a core team of experts ready to deploy overseas within 48 hours to support countries in responding to disease outbreaks.
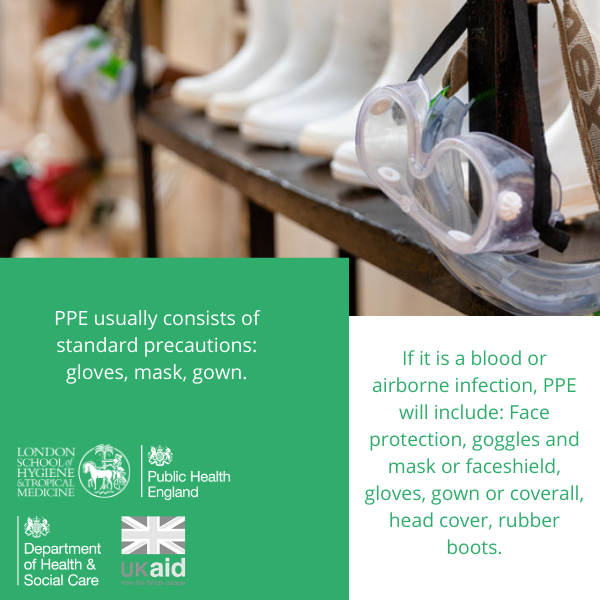
The deployable team includes experts in tracking the progress of an outbreak (epidemiologists); in diagnosing the cause of an outbreak (microbiologists); in advising on outbreak control measures (infection prevention and control) and community responses to outbreaks (social scientists); and in developing the best clinical response measures (clinical researchers). The full team comprises:
- Epidemiologists
- Clinical researcher
- Social scientist
- Microbiologists
- Data scientist
- Infection prevention and control expert
- Logistician
Deployment of the UK-PHRST is at the invitation of the host government or in response to requests made by the World Health Organization (WHO) or by the Global Outbreak Alert and Response Network (GOARN).
Reservist team
In addition to the deployable team, the UK-PHRST will train a group of public health reservists to ensure the UK is able to scale up its response to any disease outbreak or health emergency. Information on how to join the public health reserve cadre will be posted as soon as it is available.
- Case study: UK-PHRST action against Lassa fever
-
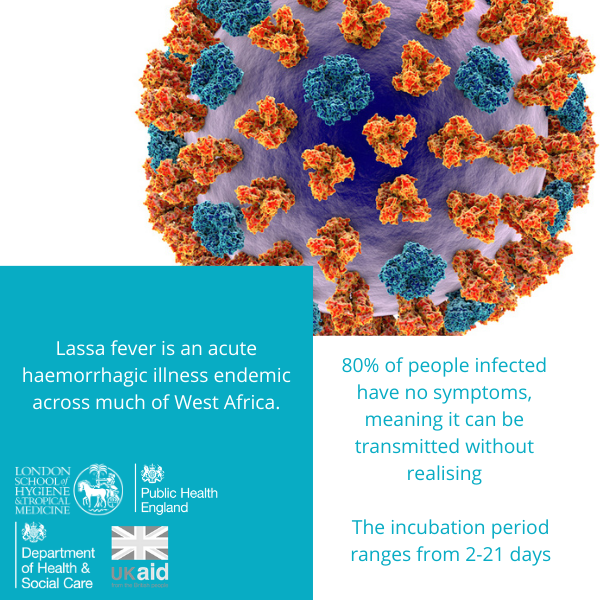
Lassa virus causes a potentially fatal haemorrhagic fever syndrome that, in its most severe form, is similar to Ebola virus disease. The virus is carried by a rodent called the “multimammate rat”, which is found across West Africa, infecting humans exposed to infected rodent excreta, with occasional secondary transmission between humans, including to healthcare workers. There are estimated to be hundreds of thousands of infections and tens of thousands of deaths due to Lassa fever every year, with transmission usually peaking during the dry season.
Outbreak response: Putting out the fire
Lassa fever reached epidemic proportions in Nigeria during the dry seasons of 2018 and 2019, prompting the Nigerian Centres for Disease Control to request support from the UK-PHRST. The UK-PHRST quickly deployed personnel to provide epidemiologic, laboratory, and logistical support to Nigeria to help bring the outbreak under control.
Research: Identify the causes of the fire
The UK-PHRST is collaborating with investigators in Nigeria and Sierra Leone – two countries where Lassa fever is hyperendemic and often leads to epidemic spread – to fill key knowledge gaps regarding this dangerous disease. These include studies exploring the clinical evolution and pathogenesis of Lassa fever and looking at the pharmacokinetics of ribavirin, a drug used to treat the disease but whose efficacy and mechanism of action remains to be determined.
In the laboratory, the UK-PHRST is working on the development of a less invasive diagnostic antibody test that can be performed on saliva (as opposed to on blood), which will facilitate field studies on risk factors for transmission. The UK-PHRST is also engaged in social science research to better understand healthcare seeking behaviour for febrile illness in an effort to encourage early recognition and presentation of care for people with Lassa fever, potentially allowing rapid implementation of life-saving care.
Capacity building: Preventing future fires
With an eye to the long-term, the UK-PHRST is helping to development clinical research capacity at the Kenema Lassa Ward in Kenema, Sierra Leone, one of the major care centres for the disease in West Africa. This will facilitate the study of novel therapeutic agents and vaccines for Lassa Fever, with the hope of ultimately being able to prevent the disease. In addition to enhancing the physical infrastructure in Kenema, the UK-PHRST has sponsored the training of local physicians in the use of various techniques, such as echocardiography to assess cardiac function, to better understand the pathophysiology of Lassa fever, and thus provide better clinical care.
Background to the UK-PHRST
The Ebola crisis in West Africa in 2014/15 highlighted the need for the international community to develop a system to help countries respond to and control disease outbreaks that pose a threat to public health, before they develop into a global emergency.
The UK Public Health Rapid Support Team was developed as part of the UK contribution to global health security and to complement the World Health Organization’s work on the Global Health Emergency Workforce. The team is funded over five years by £20 million made available from the UK official development assistance budget. Former Public Health Minister Nicola Blackwood officially announced the launch of the team in November 2016.
The London School of Hygiene & Tropical Medicine was chosen to lead the UK-PHRST in partnership with Public Health England. LSHTM is a world authority in public and global health research. During the Ebola crisis, LSHTM staff advised governments, analysed data to assist in response planning, conducted clinical trials of vaccines and treatments, provided a free online course for healthcare professionals, developed culturally sensitive interventions to change behaviour in local communities, volunteered on the frontline in Ebola treatment centres, and carried out research to strengthen the global response to future infectious disease epidemics. LSHTM was also involved in the response to the Zika virus outbreak and ongoing related research.
Further information:
The UK-PHRST is funded by UK aid from the Department of Health and Social Care and is a partnership between the London School of Hygiene & Tropical Medicine (LSHTM) and the UK Health Security Agency (UKHSA) with contributing academic partners.

Ed Newman
UK-PHRST Director (UKHSA)
UK-PHRST Director (UKHSA)/Honorary Professor in the Practice of Global Outbreak Response, LSHTM

Gwenda
Hughes
Deputy Director for Research UK PHRST
UK-PHRST Deputy Director of Research (LSHTM)/Professor of Epidemiology and Public Health, LSHTM
Susan Ismaeel
UK-PHRST Programme Manager (UKHSA)

Thom Banks
UK-PHRST Programme Manager (LSHTM)
Cristina Leggio
Lead Microbiologist (UKHSA)
Anthony Twyman
IPC Team Lead (UKHSA)/Senior IPC Specialist (UKHSA)
Infection Prevention and Control Team Lead (UKHSA)/Senior Infection Prevention and Control Specialist (UKHSA)
Claire Bayntun
UK-PHRST Head of Capacity Strengthening (UKHSA)
UK-PHRST Head of Capacity Strengthening (UKHSA)/Honorary Clinical Consultant, Global Leadership Programmes, LSHTM
Victor Del Rio Vilas
Epidemiology Co-lead (UKHSA)
UK-PHRST Epidemiology Co-lead (UKHSA)/Senior Epidemiologist (UKHSA)

Hilary
Bower
Associate Professor in Epidemiology
UK-PHRST Epidemiology Co-lead (LSHTM)/Associate Professor in Epidemiology, LSHTM

Farhana
Haque
Assistant Professor
UK-PHRST Implementation Science lead (LSHTM)/Assistant Professor, LSHTM

Shelley
Lees
Professor Anthropology of Public Health
UK-PHRST Social Sciences lead (LSHTM)/Professor of Anthropology of Public Health, LSHTM

Nadine
Beckmann
Associate Professor in Social Science

Julian
Eaton
Assistant Professor Global Mental Health
UK-PHRST Mental Health and Psychosocial Team lead (LSHTM)/Assistant Professor of Global Mental Health, LSHTM

Gwenda
Hughes
Deputy Director for Research UK PHRST
UK-PHRST Deputy Director of Research (LSHTM)/Professor of Epidemiology and Public Health, LSHTM

Ed Newman
UK-PHRST Director (UKHSA)
UK-PHRST Director (UKHSA)/Honorary Professor in the Practice of Global Outbreak Response, LSHTM
Richard Amlôt
Scientific Programme Leader, Behavioural Science (UKHSA)
Miles Carroll
University of Oxford
Jake Dunning
Senior Clinical Research Fellow in Emerging and High Consequence Infectious Diseases (University of Oxford)
Martin Hibberd
Professor of Emerging Infectious Disease (LSHTM)

Adam
Kucharski
Prof of Infectious Disease Epidemiology

Shelley
Lees
Professor Anthropology of Public Health
Chinwe Lucia Ochu
Director, Prevention, Programmes & Knowledge Management, Nigeria Centre for Disease Control

Bhargavi
Rao
Clinical Associate Professor Pub. Health
Mohammed Abdulaziz
Head of Disease Control and Prevention (Africa CDC)
Nigel Field
Director of the Centre of Molecular Epidemiology and Translational Research at the Institute for Global Health (UCL)

Thom Banks
UK-PHRST Programme Manager (LSHTM)
E. Wangeci Kagucia
Research Fellow, KEMRI Wellcome Trust
William Nicholas
UK-PHRST Project Manager (LSHTM)
TSC Facilitator
Stella Atim
Senior Veterinary Officer, Animal Disease Diagnostics and Epidemiology, Ministry of Agriculture Uganda
Abdul
Sesay
Assistant Professor
Jonas Brant
Professor of Public Health, University of Brasilia
The UK Public Health Rapid Support Team (UK-PHRST) receives requests for deployment through WHO-GOARN, direct requests from the government of the state affected by the epidemic, or through the UK Emergency Medical Team and DFID.
The first deployment of the UK-PHRST took place in April-May 2017, when two epidemiologists and one clinical researcher deployed through GOARN to the Somali Regional State of Ethiopia to support an escalating outbreak of acute watery diarrhoea.
This was followed in May-June 2017 by a deployment through GOARN to Nigeria when a team of two epidemiologists and one laboratory microbiologist assisted in the response to an outbreak of cerebral meningitis.
The UK-PHRST’s first bilateral deployment was to Sierra Leone (August-September 2017) when two epidemiologists, two microbiologists, one logistician, two Field Epidemiology Training Programme (FETP) fellows and the UK-PHRST Director were deployed. In this instance they assisted in the establishment of water-borne disease surveillance and assessment of diagnostic capacity at Connaught Hospital in Freetown in the wake of heavy rains, flooding and landslides in and around the capital.
In October – November 2017, two epidemiologists and one clinician were deployed to Madagascar though GOARN to support the response to an outbreak of pneumonic plague affecting primarily two large urban centres.
This was followed by a deployment to Bangladesh (December - January 2017/18) when a team consisting of an epidemiologist, a FETP fellow and an Infection Prevention Control (IPC) specialist worked alongside the UK Emergency Medical Team and DFID in support of the international response to the outbreak of diphtheria in the displaced Rohingya population in refugee camps in Cox’s Bazar.
The second bilateral deployment came in February-March 2018 in Nigeria, when an epidemiologist, FETP fellow, case management specialist and a logistician supported the government in controlling a large outbreak of Lassa fever through field-level interventions, logistics, capital-level data analysis and intervention strategy. This fostered a good partnership between UK-PHRST and Nigeria Centre of Disease Control (NCDC). In February-March 2019, UK-PHRST were invited to support the control of the a Lassa fever outbreak in Nigeria once more.
During February – March 2018, two epidemiologists and one infection prevention and control specialist were deployed to Bangladesh once again to support the WHO response to surveillance and monitoring of infectious disease outbreaks in the Rohingya refugee camps in Cox’s Bazar. In July 2018 an IPC specialist was redeployed to Cox’s Bazar.
In May-June 2018 during the Ebola outbreak in DRC, UK-PHRST deployed two epidemiologists and a data scientist to support with strengthening the alert system, including case investigation, protocol development, epidemiological analysis and data management.
The UK-PHRST is still actively engaged in the ongoing Ebola outbreak in DRC and has been instrumental in providing senior epidemiological support and in setting up the analytical cell, which is fully operational at the strategic coordination level (currently in Goma).
In 2019, deployments of UK-PHRST epidemiologists, data scientists and IPC specialist in response to the Ebola outbreak in DRC, have been continuous through GOARN.
At the end of March 2020, UK-PHRST in-person deployments to Africa CDC (Ethiopia), WHO Western Pacific Regional Office (the Philippines) and WHO Nepal to support the response to the emerging COVID-19 outbreak were cut short. This was due to the abrupt cessation of flights and rapid closure of borders globally. Despite the rapid change in location, the teams quickly adapted to remote working, continuing the support they had initiated with colleagues overseas.
This coordinated package of remote support has continued alongside in-person deployments when possible, subsequently benefiting from the team’s ability to draw on additional expertise from the pool of reservists and extended team when required.
Summary of Key COVID-19 Response Activities
Africa CDC
Initially an epidemiologist, infection prevention and control (IPC) specialist, social scientist and microbiologist were engaged directly at the Africa Centres for Disease Control and Prevention (Africa CDC) headquarters in Ethiopia. Since their return to the UK, a comprehensive programme of remote support has continued. Key areas include:
- Epidemiology
- Infection prevention and control
- Laboratory
- Social science
Bangladesh
We continue to build on previous UK-PHRST deployments as well as remote support to WHO’s Sub Office in Cox’s Bazar, with support from Field Epidemiology Training Programme (FETP) Fellows and UK-PHRST reservists. Key areas include:
- Epidemiology and data science
- Infection prevention and control
- Laboratory
- Research - Read about the COVID-19 seroprevalence study
Read more: UK Public Health Rapid Support Team COVID-19 Response – Bangladesh
WHO African Regional Office
One UK-PHRST field epidemiologist and two data scientists assisted WHO AFRO with analysis and interpretation of data gathered from across member states. The team supported WHO AFRO remotely and provided brief reports on the data that different countries had provided.
WHO Country Office (WCO) Tajikistan
In June, the UK-PHRST deployed one microbiologist and one epidemiologist on an assessment mission to determine the appropriateness, feasibility and likely impact of deployment of a Rapid Response Mobile Laboratory (RRML) to support the COVID-19 response. This was in response to a request for support through the Global Outbreak Alert and Response Network for the Tajikistan Ministry of Health and Social Protection in response to increasing case numbers of COVID-19.
The Gambia
Following a joint rapid assessment on COVID-19 response with colleagues from Africa CDC, UK-PHRST deployed a team of four to support the scaling up of testing and contact tracing services and the improvement of data systems. This was a bilateral deployment in collaboration with the Ministry of Health with support from two epidemiology specialists and two laboratory experts, all of whom have now returned to the UK and will continue to engage remotely.
Read more: COVID-19 Surveillance in The Gambia
Strengthening public mental health in Africa in response to COVID-19
Globally, mental health faces unprecedented challenges due to COVID-19. Bereavement, isolation, loss of income and fear are triggering mental health conditions or exacerbating existing ones. National leaders face significant challenges in protecting and scaling up mental health support as part of the COVID-19 response. A recent WHO global survey indicated that 37% countries reported that COVID-19 mental health response plans were only partially funded and a further 37% reported having no funds at all.
The UK-PHRST “Strengthening public mental health in Africa in response to COVID-19” project, due for completion in March 2021, aims to better understand enablers and barriers to integrating mental health and psychosocial support (MHPSS).
Read more: UK-PHRST Strengthening public mental health in Africa in response to COVID-19
When not responding to disease outbreaks, the UK Public Health Rapid Support Team (UK-PHRST) conducts rigorous operational research to improve epidemic preparedness and enhance our understanding of how best to tackle these threats in the future.
The team’s work will help generate an evidence base for best practice in disease outbreak interventions.
The London School of Hygiene & Tropical Medicine (LSHTM) leads an academic consortium which includes University of Oxford, King's College London and University of Glasgow, to carry out this research.
LSHTM
At LSHTM there are academics from a range of disciplines who are involved in research related to the UK-PHRST. Their areas of expertise include epidemiology, mathematical modelling, anthropology, community engagement and trust, virology, bacteriology, mental health and clinical research.
Projects include:
- Epidemic Response Anthropology Platform
-
The UK-PHRST funds the Epidemic Response Anthropology Platform, which is a partnership between LSHTM and the Institute of Development Studies. The platform is a resource to support a humane and effective response to epidemics. It aims to promote evidence on the social dimensions of epidemics in different contexts and to improve the way this evidence is used in response planning. The platform builds networks of anthropologists and other social scientists with regional or subject expertise and connects them to policy makers, scientists and humanitarian response workers involved in responding to outbreaks.
- The contribution of social science research to outbreak response
-
This work was led by Shelley Lees and Karl Blanchett (LSHTM). The project had two components:
- Component one consisted of exploring the views and experiences of anthropologists and other social scientists, and key information from organisations involved in infectious disease responses on the role of social scientists.
- Component two consisted of conducting secondary data analysis of research concerning community views and experiences of the Ebola response during the 2014 to 2016 Ebola epidemic.
An oral presentation was delivered at the Quebec Outbreak Intervention Symposium 2017, with Shelley Lees being invited as a main speaker. Manuscripts describing the work are being finalised.
This project has raised the profile of the UK-PHRST within the social science community. A social science working group has been formed at LSHTM to support the research team, which will be sustained. The findings of this work helped define the profile of the social researcher to be recruited into the UK-PHRST and have also guided the social science working group when developing the social science research strategy. On a wider scale, these findings will inform contemporary debates about the role of social scientists and anthropologists in outbreaks, and on how to engage with affected communities.
- Effect of acute illness on contact patterns, Malawi
-
This work was led by Judith Glynn (LSHTM). Understanding population mixing patterns are vital for predicting how infectious diseases move through communities. This project aimed to assess how acute illness affects contact patterns in a rural African setting in northern Malawi. We recorded contacts over 48-hours following a clinic consultation for acute illness and again 2-3 weeks later for the recovered person and for their mother/carer, if a child.
We documented changes in contact patterns when ill and these findings will help to refine models of infection transmission, which are essential for understanding how infections spread, and for planning appropriate interventions. We are preparing a paper for publication.
- Study of the aetiology of severe undifferentiated febrile illness outbreaks in Sudan
-
This work was led by Hilary Bower (LSHTM), Tom Fletcher (Liverpool School of Tropical Medicine), and Mubarak Mustafa El Karsany (Karary University/Federal Ministry of Health (FMoH)).
The research aims to assist the FMoH of Sudan to identify the causative agent(s) of outbreaks of febrile illness associated with haemorrhagic symptoms that occur regularly in the country and to inform public health intervention and diagnostic capacity for them.
The study involves testing legacy samples from an outbreak in Dafur in 2015/16 (~500 case; 18% case fatality) at PHE Porton Down, and developing a prospective study with a FMoH and Karary University team to encourage more rapid identification and better description of the disease in future outbreaks.
To date, a set of stored outbreak samples have been prepared and transferred, with the collaboration of colleagues from the National Public Health Laboratory (NPHL) and FMoH agreement, to PHE Porton Down and tested on a bespoke panel of molecular and serological assays covering a broad range of likely pathogens. Results have been shared with the Ministry and will be published shortly. A prospective study protocol has been developed with ethical approval from LSHTM, Karary University and the FMoH Technical Review Board, and a seven-person team has been trained in study implementation, with basic logistics also in place for a rapid start if/when an outbreak occurs. If no outbreak of the syndrome occurs within the current grant period, the protocol will remain in place ready to be triggered by Sudanese colleagues and we anticipate a request for UK-PHRST support may be made at that time.
Our project has created a new and strong collaboration with the FMoH and the NPHL, and provided a good example of UK research collaboration and support to improve outbreak investigation and control in Sudan. As health scientists in Sudan emerge from the period of sanctions, we hope these relationships with key outbreak-related departments of the FMoH will create further opportunities to assist outbreak response and International Health Regulation capacities in the country.
- Establishing real-time evaluations of WASH on disease outbreaks in emergency settings
-
This work was led by Oliver Cumming and Lauren D’Mello-Guyett (LSHTM). The project aimed to combine the academic experience of LSHTM and the operational experience of Médecins Sans Frontières (MSF) to strengthen the evidence base for Water, Sanitation and Hygiene (WASH) interventions used in disease outbreaks in emergency settings in low and middle-income countries (LMICs).
The role of WASH interventions as a means to both preventing and controlling infectious disease outbreaks is well established. However, at a practice and policy level, there have been calls to address the evidence gap as to how WASH interventions can be best mobilized to support during outbreak responses. We therefore developed approaches for evaluating the WASH component of MSF outbreak responses with a particular focus on study designs and methods that are appropriate for cholera outbreaks during complex emergencies.
Using these approaches to more rigorously evaluate WASH interventions will help strengthen the effectiveness of routinely delivered interventions for cholera control and improve access and outcome among vulnerable populations in low income settings.
Three summary reports are available from our field site visits to MSF projects in Nigeria and South Sudan, evaluating the ability, risks, and ethical considerations to be able to conduct operational research in such a setting. These are supplemented by a desk-based study including interviews with MSF staff in Central African Republic and Democratic Republic of Congo (DRC).
Three “sleeper protocols” that could be adapted for urban or rural contexts and/or closed or open settings within DRC have been developed. Ethical approval has been granted on the basis that an update will be submitted when an appropriate study site has been identified at the start of a conducive cholera outbreak. The collaboration has continued with MSF with plans to implement the protocols in DRC during the next cholera outbreak. Copies of the reports and protocols can be obtained on request from oliver.cumming@lshtm.ac.uk.
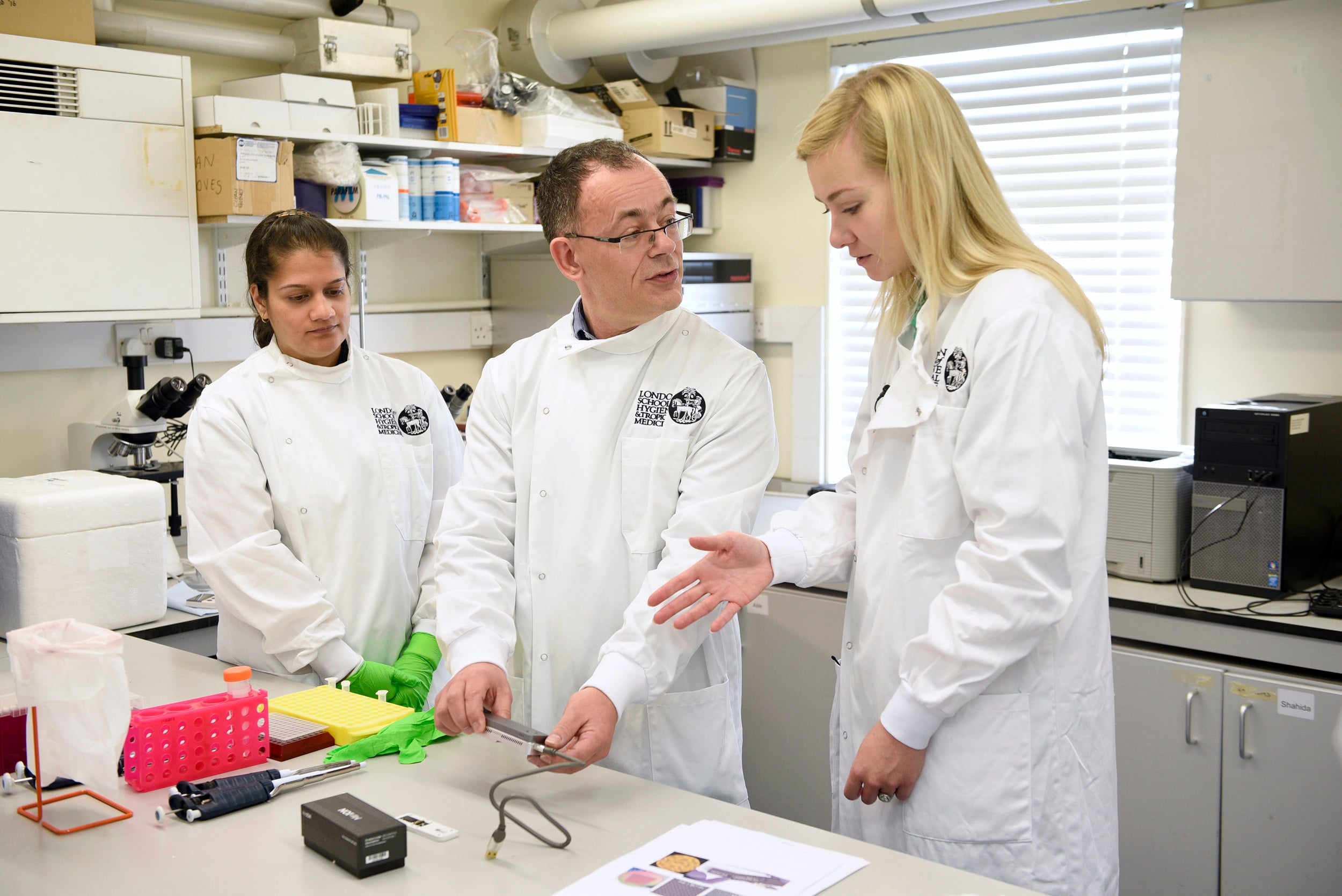
- Building readiness for real-time pathogen sequencing for surveillance and control of infectious disease outbreaks
-
This work was performed by teams from PHE and LSHTM. The aim of the study was to take advantage of new technologies for near-real time genome sequencing in the field. We aimed to develop specific genome sequencing primers for selected viruses capable of causing outbreaks, validate sequencing methods and primers using UK returning traveller clinical samples and evaluate MinION sequences in relation to MiSeq,
Equipment is now in place within UK PHRST for amplicon-based viral whole-genome-sequencing on the MinION, primer sets have been designed and provisioned for 4 dengue virus serotypes, 3 chikungunya lineages, and 5 Lassa virus lineages. The UK PHRST lead microbiologist has been trained in the use of the MinION and the primer sets, a bioinformatic pathway has been developed in-house at LSHTM. Testing shows DENV-1,2,3 and CHIKV Asia and ECSA schemes are fully effective at detecting viruses with good genome coverage.
However, the schemes were less effective for DENV-4, CHIKV West Africa and Lassa; most likely due to lack of a relevant reference genome and future work could be done to establish this. A strategy for amplicon-based Crimean Congo Haemorrhagic Fever (CCHF) virus genome sequencing has also been developed by PHE using a separate funding source. The primers and protocol are also available to the UK PHRST. All established protocols could now be field tested for further integration into the PHRST.
We aim to transfer technology to laboratories in West Africa and evaluate performance in an LMIC setting, and utilize sequence clustering and other bioinformatics tools to determine the performance of sequence results in identifying transmission.
University of Glasgow
The MRC-University of Glasgow Centre for Virus Research (CVR) is home to an internationally leading critical mass of virologists, entirely focused on the study of human viral diseases and viruses at the human-animal interface. Established in 2010 as a partnership between the University and the Medical Research Council (MRC), the CVR contributes to national virology capability and supports the global response to viruses and the diseases they cause.
- Collaborative supervision of a healthcare worker study in Uganda
-
Kasese District is nestled in the far western corner of Uganda, surrounded by mountainous national parks, and bordering the Democratic Republic of Congo (DRC). Building on existing collaborations with Kagando hospital, a team from the MRC-University of Glasgow Centre for Virus Research (CVR) is investigating the prevalence of exposure to viral hemorrhagic fever viruses (VHF viruses) and SARS-CoV-2 in health care workers and surrounding communities. VHF viruses are regularly seen in this part of Uganda and cause a variety of diseases: Rift Valley Fever (RVF), Ebola and Crimean congo haemorrhagic fever (CCHF). This study seeks to understand the epidemiological spread of disease in healthcare workers and abattoir workers in order to strengthen prevention strategies.
Pandemic roadblock
After successfully running several studies in Uganda, international travel was suspended and team members from the UK were unable to visit the research sites. However, with the leadership of Dr Mary Munyagwa, medical director at Kagando hospital and Stella Atim, a veterinarian and PhD fellow at Makerere University who is investigating CCHF in Uganda and remote assistance from members of the CVR team, the study went ahead. Laheri Kabugho was appointed as team leader with Mercy Musoki, Joshua Muhindo, Esther Atolere and Mercy Kabugho as study nurses, Bettress Happy and Robinah Aliganyira as HIV counselor, Robert Muhindo as community mobilizer and Edson Masereka as laboratory technologist. Alongside the need to train staff in sample collection and research, the UK team also ensured that equipment was delivered in a timely and safe manner – with items such as blood tubes and needles, a heat block, and the relevant trial documentation i.e. consent forms.
What did they do about it?
Zoom provided the platform to carry out remote training with powerpoint slides and videos shared online. WhatsApp daily communication was also an essential tool.
(L-R): Mercy, Bettress, Laheri and Joshua in Kagando, with Marina on Zoom. Marina Kugler, Project Coordinator, made sure that the equipment and necessary items for the study arrived, carefully boxed and labelled from Glasgow.
‘We organised kits and lab equipment, printed out consent forms and packed boxes with needles, phones, face masks and much more. Everything was labelled so the participants could be easily recruited and to reduce administrative errors in the very important documentation of the study’.
The minutiae required in planning a remote study was not underestimated and enabled the successful implementation of the research. Participants were recruited at a rate of ~30 per day, blood samples were heat inactivated and stored in the delivered freezer, before transported to Entebbe for testing at the UVRI.
Blood samples for transportation Study questionnaires were filled out via mobile phones and REDCap, rather than by paper, to allow quick collection and safe storage. Data is available in real time online, which allowed Marina to check for missing values and any queries were resolved on Whatsapp – the fastest and most reliable way to communicate with the study site. Laheri and the team also commented on the ease they felt in getting help and support from the remote team.
‘The care and the support you gave us was the best part of the study. It was not as we were alone, we were always with you during the whole study.’ - Laheri
One of the key elements of any study is the mobilisation of communities and this was carried out very effectively by the study team. Stella, Laheri and Robert would meet with a member of the village health team and the village leader to explain the study. Through these contacts, they would organise mobilisation in the villages to recruit participants.
What can we learn?
Clear expectation setting with stakeholders is important, especially in regard to the availability of data for analysis. Depth is paramount with many qualitative or mixed-methodological studies, and when timing is disrupted, staying open, positive, and accommodating goes a long way toward ensuring high-quality data. It’s advisable to build in padding for each and every stage of the research process, from recruitment through to analysis. Staying flexible will help ensure maximum number of participants are recruited and it will also reinforce a collaborative research ethos, which is important now more than ever.
What is next?
Right now, the team is working on the data analysis of all 300 health care workers with their sex/age/geographically matched 450 community members. The results will provide information about the epidemiological spread of viral infections in the expected special risk group of health care workers. Results will be communicated to the study groups and solutions for risk reduction will be developed together.
University of Oxford
The Epidemic Diseases Research Group Oxford (ERGO) delivers on the clinical operational research theme and contributes to the core deployable team and the training and capacity building in low and middle income countries. ERGO is led by Professor Peter Horby and the group aims to reduce the health and socioeconomic impact of emerging and epidemic infections by conducting and enabling clinical research in this area.
Since the launch of the UK-PHRST, members of the Oxford team have worked in Ethiopia, Nigeria, Madagascar, Sierra Leone, Nigeria and Cambodia, either as part of deployments or on research projects with local staff.
Selected research projects completed by ERGO:
- Rapid needs appraisal to inform clinical research priorities in response to (re-) emerging outbreaks
-
This work was led by Louise Sigfrid together with Alex Salam, Catrin Moore and Peter Horby.
The evidence base for the response to epidemics of (re-)emerging pathogens is limited. Research is rarely an early priority, there are many challenges at the outset of an epidemic, and there is a limited window of opportunity to implement research.
This means it is important that the priorities for research are rapidly, but rigorously defined during the earliest stages of an epidemic, while considering ethical aspects and ensuring the potential for a direct clinical and public health impact.
A methodology for rapidly (≤5 days), systematically and transparently identifying key knowledge gaps to inform research priorities during emergency outbreaks was developed in collaboration with Evidence-Aid and Cochrane response.
The intention is that the outcome from the rapid research needs appraisal will be used to inform clinical research prioritisations.
The methodology was piloted in July 2017 using a Lassa fever outbreak scenario and the results compared with expert opinions collected from Lassa fever experts to inform the final version of the protocol.
The methodology was presented at the Global Evidence Summit in South Africa in September 2017.
- Patient data quality improvement in epidemics: An audit of West African Ebola data
-
This work was led by Amanda Rojek, Alex Salam, Peter Horby and the Infectious Diseases Data Observator.
Good medical record keeping is a challenge, particularly in humanitarian public health emergencies, and this is likely to impact clinical care for patients.
The overall aim of this project was to evaluate the quality of clinical data from patient records from the West African Ebola outbreak (2014/15).
The project was divided into 3 sub-projects:
- A systematic review and metaanalysis of published clinical data from the West African Ebola outbreak
- A questionnaire for healthcare workers, investigating their perceptions of the quality of clinical record keeping whilst working in West African Ebola Treatment Centres
- An audit of clinical data from 5,000 Ebola virus disease clinical case records from West Africa
This project will help generate an evidence base for best practice for medical record keeping in disease outbreaks and humanitarian emergencies in developing countries.
- An evaluation of syndromic surveillance and clinical characterisation of EEID syndromes in refugee camps
-
This work was led by Amanda Rojek together with Karl Blanchet (LSHTM) and Peter Horby.
There is an unprecedented global forced migration, with the UN Refugee Agency (UNHCR) estimating that more than 65 million people are in need of protection. At least 12 million of these are living in refugee camps, which are a high risk environment for disease outbreaks.
This work aimed to improve the provision of accurate and comprehensive clinical information that verifies an outbreak, characterises the likely cause and severity of illness, and identifies populations at risk.
The team collected prospective data from thirteen refugee camps across Greece, where research nurses observed clinical consultations with recently arrived refugees presenting with syndromes consistent with outbreak prone infectious diseases.
The data were collected to find out the extent to which the risks for infection, severity of infection and clinical manifestations of infection were assessed and recorded.
The study findings were published in BMC Medicine.
ERGO have several research projects currently underway. These include: Rapid identification and characterisation of avian influenza viruses by direct Nanopore sequencing in collaboration with Institut Pasteur du Cambodge; an ongoing cohort study looking at clinical characterisation and microbiological diagnosis of patients with suspected pneumonic plague in collaboration with Institut Pasteur de Madagascar; and Lassa fever cohort study based in Sierra Leone and Nigeria in collaboration with Kenema Government Hospital and Owo Federal Medical centre respectively.
In collaboration with the WHO/Tropical Diseases Research (TDR) programme, ERGO developed and ran a training curriculum on generating clinical evidence during outbreaks in lower and middle income countries (the Clinical Research During Outbreaks Course - CREDO). The delivery of the curriculum will build capacity overseas for an improved and rapid national research response to disease outbreaks. CREDO received accreditation for the African Academy of Sciences in 2017. The work was presented in October 2017 as a poster at the 10th European Congress on Tropical Medicine and International Health, Antwerp, Belgium.
King’s College London
Research into the mental health aspects of infectious disease outbreaks is led by a joint team from the NIHR Health Protection Research Unit in Emergency Preparedness and Response at King’s College London and the South London and Maudsley NHS Foundation Trust.
Projects already completed by the team as part of their UK-PHRST work include studies to understand the feasibility and effectiveness of small group therapy for staff in Sierra Leone who worked in Ebola treatment centres, the preliminary results of which are available in the International Journal of Social Psychiatry.
Ongoing work involves assessing whether it is possible to ‘screen’ people who wish to work on future infectious disease outbreaks, to identify and support people at risk of experiencing distress as a result of this work. For further information, please contact Dr James Rubin at KCL.
UK-PHRST attends CPHIA Conference 2023: Repositioning Africa in the global health architecture
In November, UK-PHRST members attended the 3rd 2023 International Conference on Public Health in Africa (CPHIA) in Lusaka, Zambia alongside thousands of delegates from across Africa and further afield. They launched a Global Health Diplomacy course which was developed with Africa CDC, discussed how best to respond to infectious disease outbreaks and strengthened our partnership with Africa CDC to support mental health across the continent. This annual conference provides a unique African-led platform for public health leaders across the continent to reflect on lessons learned in health and science and align on a way forward for creating more resilient health systems.
Dr Ed Newman, UK-PHRST Director said:
“This year’s International Conference on Public Health in Africa was a great opportunity for the UK-PHRST to support our Africa-CDC colleagues with their events and partake in some critical side events ourselves – further building on the excellent relationships we have in the region. I was especially pleased to see the emphasis on African health leadership to build solutions for the continent’s public health challenges, particularly exemplified by the close alliance demonstrated by Africa CDC and WHO Senior leadership. We support their clear call for nationally driven, local responses to public health threats - further emphasising the value that both organisations place on collaboration."
See the pictures from the event.
Interregional One Health cross-border simulation exercise
At the request of the World Health Organization (WHO) Ethiopia country office, UKHSA teams including the UK-PHRST, mobilised to help deliver a unique and complex One Health cross-border simulation exercise between Ethiopia, Somalia and Kenya, that was held in Addis Ababa in October 2023.
UK-PHRST colleagues alongside others from the UKHSA’s International Health Regulations Strengthening Project (IHR-SP) based in both the UK and Ethiopia, and UKHSA’s Global Health Consultants joined forces with stakeholders from across the three countries and other international partners to test preparedness, operational readiness, and cross-border and cross-sector coordination in the event of a One Health-related threat – in this case, anthrax.
Hibo Asad a Field Epidemiologist with the UK-PHRST, reflected on her experience:
“A key highlight for me was the inclusion of the community representatives across Ethiopia, Kenya and Somalia – facilitated by Risk Communication and Community Engagement (RCCE) Colleagues in the UK-PHRST. This is the first time we have held a workshop of this magnitude with community representatives involved and contributing to discussions on cross-border preparedness and coordination against One Health threats. Their shared perspectives significantly strengthened the One Health discussions, bringing to the table very insightful on the ground experience and wisdom.”
The simulation exercise was well received by all participants, with community experts applauding “the sharing of expertise and resources to collaborate in achieving a common goal”.
Dr Lilian Wambua, Regional One Health Coordinator at the World Organization for Animal Health, also praised the cross-organisational work in her closing remarks, saying:
“Thanks to colleagues from WHO, UKHSA, PANDORA and other organisers. The level of inclusivity has been phenomenal, from community to high-level policy makers, all allowing for smooth partnership working.”
The findings from the exercise are currently being evaluated and written up. These will be shared with key country stakeholders to start taking the next steps towards cross-border health security using a One Health approach.
UK-PHRST team and partners are currently delivering ten research projects, a selection of which are highlighted below.
UK-PHRST Panel Discussion and Q&A: Working with family caregivers to improve infection prevention and control in hospitals
This discussion and Q&A event, aimed at those working in health service delivery, policy development, health workers, Infection Prevention and Control teams and other academics, examined the role of caregivers in African healthcare systems, an often integral but largely unrecognised part of the health team.
The event began with presentations focusing on the healthcare situation in Cameroon and Malawi specifically delivered by researchers from a variety of organisations including the UK-Public Health Rapid Support Team, the Cameroon Baptist Convention Health Service/Infection Control Africa Network, WaterAid and London School of Hygiene & Tropical Medicine.
There followed a chaired panel Q&A session with leading experts in the field, chaired by Professor Wendy Graham, an LSHTM Professor of Obstetric Epidemiology. The event was an opportunity to find out about the next steps for the research and its real-world implementation.
Event Based Surveillance Study - Cape Verde and Brazil workshops
Throughout November and December 2023, the project team held workshops in both Cape Verde and Brazil. In Cape Verde, the team met with ten community leaders who helped test the project app Guardians of Health that will be used to record the event-based disease surveillance information collected directly from communities.
The team held two workshops in Brasilia working with local community leaders to introduce the study and map out potential local individuals who could participate in data collection. Both workshops were an opportunity to engage local leaders in the project, creating a bond with the local community to enable their full participation and ensure they lead the nomination of participants using their understanding of regional dynamics. The team now intend to invite the nominated leaders to a future project development workshop as well as visiting the local territories and building stronger community bonds within the study regions.
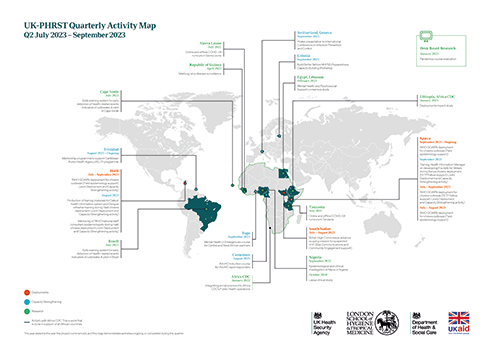
View our quarterly map to see our activities between October and December 2023.
The UK-PHRST team and partners are currently delivering 10 research projects, a selection of which are included below:
Nigeria mpox research collaboration launches
Researchers from the Nigeria Centre for Disease Control (NCDC) and the UK-Public Health Rapid Support Team (UK-PHRST) are teaming up with multiple partners for a new project to study mpox in Nigeria. Since it re-emerged in Nigeria in 2017, the mpox virus has caused numerous outbreaks globally. This research aims to increase understanding of how it spreads and affects communities in Nigeria.
NCDC, alongside partners including the UK-PHRST, the National Veterinary Research Institute (NVRI), the Niger Delta University Teaching Hospital (NDUTH), the Pandemic Sciences Institute at the University of Oxford and stakeholders in Lagos and Rivers States, launched the collaborative project at an event in Abuja on 16 October. Distinguished guests included senior national and state representatives from collaborating stakeholders and partners across Nigeria and from the UK.
The co-created research project – titled “Epidemiological and clinical investigation of mpox in Nigeria: A multi-disciplinary research project to inform case management and outbreak prevention and control” - will help address the current significant gaps in clinical and epidemiological knowledge of the virus in Nigeria. Its findings have the potential to not only strengthen detection, prevention, response, and control in Nigeria, but also inform practice in other countries across the world where mpox is endemic.
Following the launch of the research project, the UK-PHRST will continue to support Nigerian partners in the co-ordination and implementation of the study, lab capacity strengthening and data analysis.
Professor Gwenda Hughes, co-project lead, Deputy Director for Research for UK-PHRST, and Professor of Epidemiology and Public Health at LSHTM said:
“The UK Public Health Rapid Support Team is delighted to be part of this exciting collaboration between Nigeria Centre for Disease Control and other partners to better understand the clinical characteristics, pattern of infection and spread of mpox in Nigeria – a disease that has greatly affected Nigerian communities, especially in recent years.
“The UK-PHRST will support Nigerian colleagues to answer important scientific questions through this extensive research programme and will also help deliver training of local laboratory staff and field teams. Our microbiology specialists have already provided lab equipment and shared expertise to help build local diagnostic capabilities for mpox. Ultimately, through co-creation and by taking a partner-led approach with our Nigerian colleagues, our aim is to support improved case and contact management and inform the development of effective control measures for mpox both in Nigeria and globally.”
Read the full NCDC press release.
Online and offline COVID-19 rumours in Sierra Leone and Tanzania
In August 2023, the research team completed both data collection and analysis in Sierra Leone and Tanzania. The project team are currently developing an ethnographic toolkit and writing up results. Project dissemination will take place in the New Year.
Rapid Virus Genomics for Outbreak Investigation (RAViG) – Assessing the feasibility and added value in Coastal Kenya
A new study, in partnership with the KEMRI-Wellcome Trust Research Programme, Kilifi, Kenya began in October. The central aim of the project is to assess the implementation of real-time field genomics (“portable sequencing”) to support investigation and management of suspected viral outbreaks in coastal Kenya. The investigating team aim to add to the evidence base on the added value and sustainability of in-field rapid genomic sequencing relative to conventional surveillance in low resource settings. The team will explore how genomic data can help identify the cause of an outbreak or factors associated with it, and whether this information can influence policy or outbreak control measures. The project team will also work with the Kenyan Ministry of Health, Africa CDC, and the Regional WHO in delivering this research.
The UK-PHRST team has been busy delivering capacity strengthening activities advancing partnerships and contributing to the global discourse around outbreak response. A selection are highlighted below:
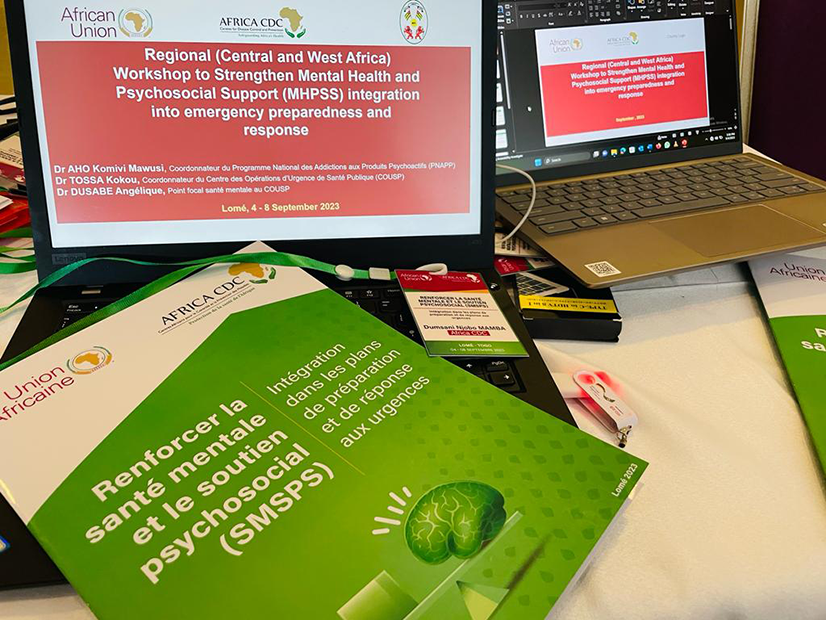
UK-PHRST supports Africa CDC’s Regional Francophone workshop on Mental Health and Psychosocial Support (MHPSS) Emergency Preparedness and Response
In September 2023, Africa CDC arranged a third regional workshop in Togo as it continues to build recognition for the importance of MHPSS in outbreaks across the African continent, focusing this time on Francophone countries in Central and West Africa. The event was part of a series of workshops, previously held in Liberia and Kenya, and was attended by 49 individuals spanning 20 countries including national leads in mental health and Emergency Preparedness and Response alongside input from the Inter-Agency Standing Committee, the UK-PHRST, UNICEF, and other regional bodies.
Julian Eaton, Co-Lead, UK-PHRST Mental Health Psychosocial Support Group attended the workshop on behalf of the UK-PHRST and said:
“National health and other sector leaders deserve coordinated and evidence-based information to drive effective response. Our international partnership with Africa CDC, WHO and regional public health institutes has proven an incredibly valuable way to support national emergency preparedness in mental health and psychosocial support.”
The workshop provided a unique opportunity to invest in learning and sharing specific evidence in French. Although around 300 million people in Africa live in Francophone countries, there is a relative lack of investment in mental health and psychosocial support in this community, something this workshop aimed to start addressing.
The series are based around a Theory of Change model, with learnings incorporated iteratively through each workshop as well as using evidence systematically gathered from other sources – ultimately aiming to support national mental health and Emergency Preparedness and Response (EPR) teams to better plan and build stronger systems for response in the event of future emergencies.
Build Better Before: Scaling up capacities for Mental Health and Psychosocial Support Preparedness and Risk Reduction
Biksegn Yirdaw, Assistant Professor in Mental Health and a member of our Mental Health and Psychosocial Support (MHPSS) team, attended a World Health Organisation international workshop held in collaboration with the Estonian government: “Build Better Before: Scaling up capacities for Mental Health and Psychosocial Support (MHPSS) Preparedness and Risk Reduction” on behalf of the UK-PHRST in September. The workshop lasted several days and included lecture session and a full-scale simulation exercise on MHPSS preparedness and response, disaster risk management (DRM) and emergency preparedness and response (EPR) in humanitarian/emergency situations.
Biksegn was involved in facilitating MHPSS need assessments, writing a standard operating procedure and developing a response plan during the simulation exercise. As a result, he deepened his expertise in conducting rapid need assessments, risk analysis, and planning during emergency situations. Using this knowledge, he will help the UK-PHRST further strengthen its MHPSS component of its outbreak response work in Overseas Development Assistance eligible countries around the world.
Bringing together more than 80 MHPSS and humanitarian experts from 35 countries, the workshop aimed to strengthen the capacities of responding organisations to integrate MHPSS into national emergency plans and to include MHPSS as part of real-world emergency response including to infectious disease outbreaks. In particular, the workshop’s approach could be used to inform the UK-PHRST’s work to design, implement and evaluate integrated MHPSS interventions in infectious disease outbreaks – ultimately progressing the team’s research portfolio and ensuring the UK-PHRST’s work can have a global impact.
Find out more about the UK-PHRST's MHPSS work.
International Conference on Infection Prevention and Control (IPC), Geneva
IPC colleagues Emilio Hornsey and Lipi Begum recently presented their poster on the review of IPC activities during outbreak response deployments by UKPHRST in 2022 at the biennial, International Conference on Infection Prevention and Control in Geneva, Switzerland. The event not only allowed international networking with academic and operational IPC colleagues but also highlighted how other governments, NGOs & civil societies manage health sector resilience and patient safety via IPC during normal and emergency outbreak responses.
View our quarterly map to see our activities between July and September 2023.
Researchers from the Nigeria Centre for Disease Control (NCDC) and the UK-Public Health Rapid Support Team (UK-PHRST) are teaming up with multiple partners for a new project to study mpox in Nigeria. The virus has caused a number of outbreaks since it re-emerged in Nigeria in 2017, and this research aims to increase understanding of how it spreads and affects people among Nigerian communities.
Nigeria Centre for Disease Control (NCDC), alongside partners including the UK-PHRST, the National Veterinary Research Institute (NVRI), the Niger Delta University Teaching Hospital (NDUTH), the Pandemic Sciences Institute at the University of Oxford and stakeholders in Lagos and Rivers States, launched the collaborative project at an event in Abuja on 16 October. Distinguished guests included senior national and state representatives from collaborating stakeholders and partners across Nigeria and from the UK.
The co-created research project – titled “Epidemiological and clinical investigation of mpox in Nigeria: A multi-disciplinary research project to inform case management and outbreak prevention and control” - will help address the current significant gaps in clinical and epidemiological knowledge that surround the virus. Its findings have the potential to not only strengthen detection, prevention, response, and control in Nigeria, but also inform practice in other countries across the world where mpox is endemic.
The research will be split into two linked studies: a clinical study and a One Health study. These will be implemented concurrently to understand the clinical characteristics, patterns and routes of infection and associated risk factors, and the experiences of people with confirmed mpox and those close to them.
Dr Ifedayo Adetifa, Director General of the NCDC, said: "Today, we begin the journey of knowledge, unity, and determination. In partnership with dedicated researchers and institutions, we set out to unravel the unknowns of the mpox virus through bridging clinical and One Health studies. This project symbolises our unwavering commitment to protecting the health of Nigerians, and in turn the world, embracing the power of research, and the strength of collaboration. As we work together, may we move closer to a world free from the threat of mpox that ensures the wellbeing of generations to come."
Using £1.6 million funding provided by the UK Department of Health and Social Care through UK Aid, the UK-PHRST – an innovative partnership between the UK Health Security Agency and the London School of Hygiene & Tropical Medicine (LSHTM) - has worked closely with the partners to co-create the research project. The collaborating organisations first met in early 2022, prior to the global mpox outbreak, to agree to co-develop a preparedness-and-response research programme on mpox in Nigeria. Following the launch of the research project, the UK-PHRST will continue to support Nigerian partners in various parts of the study from design, co-ordination and implementation, lab capacity strengthening to data analysis and publication. This will ultimately enable Nigerian partners to provide the necessary long-term laboratory support and promote sustainable mpox diagnostics in Nigeria.
Professor Gwenda Hughes, co-project lead, Deputy Director for Research for UK-PHRST, and Professor of Epidemiology and Public Health at LSHTM, said: “The UK Public Health Rapid Support Team is delighted to be part of this exciting collaboration between Nigeria Centre for Disease Control and other partners to better understand the clinical characteristics, pattern of infection and spread of mpox in Nigeria – a disease that has greatly affected Nigerian communities, especially in recent years.
“The UK-PHRST will support Nigerian colleagues to answer important scientific questions through this extensive research programme and will also help deliver training of local laboratory staff and field teams. Our microbiology specialists have already provided lab equipment and shared expertise to help build local diagnostic capabilities for mpox. Ultimately, through co-creation and by taking a partner-led approach with our Nigerian colleagues, our aim is to support improved case and contact management and inform the development of effective control measures for mpox both in Nigeria and globally.”
In his address at the launch event, Dr Edmund Newman, Director of the UK-PHRST, said: “It is great to see this project and collaboration between UK-PHRST and our Nigerian partners progressing to a point where we can launch our co-created mpox study. This has been possible thanks to significant work from all sides and builds upon the long history of the UK-PHRST’s successful work with Nigerian partners including Nigeria CDC which has evolved from bilateral support missions and more recent capacity strengthening work. We will continue to support our Nigerian colleagues as they lead the way on this flagship project to answer the important research questions about mpox in Nigeria.”
Mpox virus, formerly known as monkeypox, causes the most important global human orthopoxvirus disease since smallpox was eradicated in 1979. Since the virus re-emerged in Nigeria in 2017, reported cases have continued to increase annually. From 2017 until now, there have been 2668 suspected cases, 975 confirmed cases and 14 deaths, with Lagos and Rivers States accounting for the highest burden of the disease. As such, the research project will be implemented in Lagos and Rivers states in the first instance.
The 2022 global outbreak which affected over 100 countries coincided with Nigeria’s largest outbreak with 762 confirmed from more than 2000 suspected cases. While this sharp rise in cases is likely linked to improved surveillance and testing, for Nigeria and other endemic countries, the surge of mpox attention and information only further highlighted important gaps in clinical and epidemiological knowledge and the effect of this deficit on developing effective measures to prevent further cases. The research project aims to answer the co-identified research questions for Nigeria, while also informing practice in similar endemic settings.
Read the full NCDC press release about the event.
About NCDC
The Nigeria Centre for Disease Control and Prevention (NCDC) is the country’s national public health institute, with the mandate to lead the preparedness, detection, and response to public health emergencies. The Bill for an Act to establish NCDC was signed into law in November 2018 by President Muhammadu Buhari. The mission of the NCDC is to protect the health of Nigerians through evidence-based prevention, integrated disease surveillance and response, using a One Health approach, guided by research, and led by a skilled workforce.
Launch event attendees
The project launch event took place on 16 October 2023 in Abuja and included the following key guests amongst many others:
- Representatives of:
- Director General of Nigeria CDC
- British High Commissioner to Nigeria
- Federal Ministry of Agriculture and Food Security
- Federal Ministry of Environment
- Chief Veterinary Officer of Nigeria
- University of Port Harcourt Teaching Hospital
- Ministry of Defence Health Implementation Programme
- UK Health Security Agency (UKHSA) and UKHSA IHR Strengthening Programme
- Wild Aid
- Walter Reed Program - Nigeria/Henry Jackson Foundation Medical Research Institute
- Director of Public Health, Rivers State Ministry of Health
- The Honourable Coordinating Minister for Health and Social Welfare
- The Honourable Commissioner of Rivers State Ministry of Health
- The Chief Medical Directors of Rivers State University Teaching Hospital and Lagos University Teaching Hospital
- The President and the Acting Registrar of Veterinary Council of Nigeria
- The Director/Chief Executive of National Veterinary Research Institute,
- The Directors of Veterinary Services of Lagos State Ministry of Agriculture and Rivers State Ministry of Agriculture
- The Conservator General of National Park Service Abuja
- The Director, Public Health Laboratory Services
- The Director of Public Health, Rivers State Ministry of Health
- The State Epidemiologist, Rivers State Ministry of Health
- Disease Surveillance and Notification Officers and Clinical Health Workers from Lagos and Rivers States
- UK-PHRST speakers included:
- Co-principal Investigator
- UK-PHRST Director
Julian Eaton. Co-Lead, UK-PHRST Mental Health Psychosocial Support Group
In the face of a public health emergency such as a major disease outbreak, governments and responding organisations know they must implement public health measures to quickly control the situation and prevent loss of life. As we know all too well from COVID-19, cholera, Ebola and other disease outbreaks, infections which spread rapidly can have devastating physical impacts. There is, however, a less visible effect of these outbreaks on people’s mental health, something which is beginning to be addressed by specialists in Mental Health and Psychosocial Support (MHPSS) like the UK-Public Health Rapid Support Team’s dedicated MHPSS team.
Even outside of an emergency situation, mental health is often not part of public health measures and services are often not on par with the standard of care given to those with physical injuries. Emergencies of all kinds can increase the risk of physical and mental health problems, especially if people are displaced, so it is imperative that mental health is addressed in these circumstances.
World Mental Health Day is an opportunity to remember the importance of mental health as an essential component of global public health in both everyday and emergency situations. Although huge strides have been made to make sure mental health is not left out of outbreak response, there's still more to do before it's integrated into every health emergency response; from outbreak preparedness activities, climate change and other natural hazards and conflicts.
This year’s theme of ‘Mental health is a universal human right’, reaffirms the importance of understanding how central mental health is to achieving Universal Health Coverage - to ensure that everyone, especially the most vulnerable, has access to the care they need, even during a public health emergency.
The road to establishing best practice in MHPSS
Almost 20 years ago, the Inter-Agency Standing Committee Guidelines on MHPSS in Emergency Settings, laid the foundations for best practice in MHPSS, stimulated by the need to apply global best practice standards in times when people are most vulnerable. The principles it laid down have served the field well, and the MHPSS community has an increasing range of evidence-based tools, including the Minimum Service Package (hosted at the Mental Health Innovation Network at London School of Hygiene and Tropical Medicine). A new research agenda for 2021-2030 was recently outlined, which demonstrated how far we have come, particularly in understanding the extent of needs and the basic elements of what works to reduce suffering. A mechanism is in place to quickly provide effective coordination in emergencies under Inter-agency Standing Committee (IASC), a surge support capacity is run by the Dutch government on behalf of the MHPSS community, and other key public health agencies like Africa CDC are also putting this in place alongside their response to physical health needs.
Learning lessons from COVID-19 and beyond
The COVID-19 pandemic demonstrated both increased mental health needs, and the importance of a range of health responses; from the value of neighbours looking out for each other’s basic needs, to health organisations having to protect access to essential mental health care services that were at risk. Despite the development of good quality guidance during COVID-19, when the MHPSS community was very nimble in its response, there remain substantial gaps in evidence of what works, and in sufficient political buy-in to invest in and act on risks to mental wellbeing in emergencies. People with pre-existing mental health conditions are far more negatively impacted by outbreaks than others, and there is always a huge increase in distress and mental health needs during outbreaks among the general population, and importantly, health and other sector response organisations. There are a number of reasons behind this: anxiety about contracting infection or getting vaccinated; some direct physical, emotional and cognitive effects (for example as part of long COVID); stigma and social exclusion associated with infection; and probably most significantly, the impact of social changes like isolation, economic loss, or educational disruption, especially when these are over prolonged periods.
How the UK-PHRST is making MHPSS part of outbreak response
The UK-PHRST strives in all areas of its work to create lasting change in response to infectious disease outbreaks across the globe by putting emphasis on knowledge co-creation, global partnerships and real-world action. This is no different for the UK-PHRST’s MHPSS team. Through our innovative research, capacity strengthening efforts and advocacy for on-the-ground response work, the MHPSS team works to bring mental health interventions to the fore of outbreak response and empower countries across Africa, Official Development Assistance (ODA) eligible countries and the wider global community to create real and lasting positive change for those affected by mental health problems following an infectious disease outbreak.
The UK-Public Health Rapid Support team has a dedicated MHPSS group, focused on research, capacity building, and deployment in the intersection of mental health, wellbeing and infectious disease outbreaks. Our work includes:
- Strengthening MHPSS preparedness and response at national level through collaborating with public health institutions like Africa CDC, WHO, Inter Agency Standing Committee, West African Health Organization, East Central and Southern Africa Health Community and other agencies
- Research, with a specific focus on understanding what works in MHPSS preparedness and response at country level, through participatory implementation research. Our aim is to equip decision-makers with clear, evidence-based guidance for integration MHPSS into outbreak response. To date we have published assessments of strength of outbreak preparedness across Africa, reviews of literature, and are planning implementation research in Africa.
- Strengthening deployment mechanisms for rapid response, through collaboration with the African Volunteer Health Corps and IASC/Dutch Surge Support mechanisms
- Building networks of MHPSS and Emergency Preparedness and Response partners for ongoing peer support, learning and coordination
- Supporting responder wellbeing within the RST and across other outbreak response partners
All of these workstreams contribute to one overall aim; to understand better the factors that influence how people respond to crisis, and to equip government and non-governmental organisations to be prepared and able to respond effectively to the mental health needs of people that come about from future public health emergencies like infectious disease outbreaks.
With so much progress in recent years around the world on mental health, the UK-PHRST MHPSS team is working hard to keep up the momentum and integrate mental health measures into outbreak response so that no one is forgotten, especially during an emergency.
Work with the UK-PHRST MHPSS team
Find out more about the MHPSS team within the UK-PHRST.
If you or your organization would like to collaborate or request MHPSS help during an outbreak, please contact uk-phrst@lshtm.ac.uk.
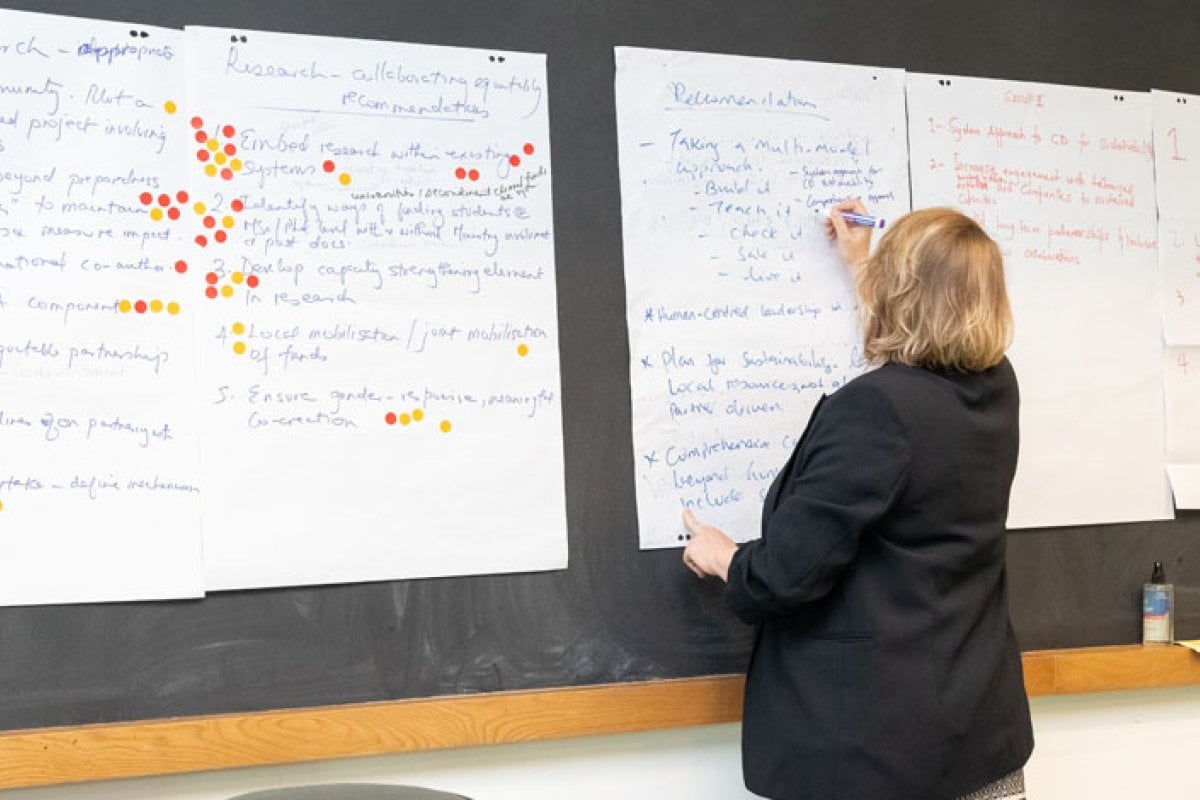
The UK-PHRST and its international partners came together to review their previous work, evaluating its strengths and weaknesses as part of a three-day Learning Review Session in Cape Town, South Africa. The discussions, in September 2022, acknowledged the ongoing success and enthusiasm for the UK-PHRST’s partnership working approach and also pointed to key issues that potentially affect the work of the UK-PHRST and international partners. These included strengthening public health leadership, narrowing the North-South technological gap, ensuring deployments create impact for host countries and embedding greater levels of equity across all working relationships.
The newly published UK-PHRST and Partners Learning Review Post Review Reflections & Actions Report highlights case studies from the discussions, and provides 35 recommendations for improved ways of working. The UK-PHRST senior leadership responded to 20 of the recommendations which the attendees felt were priority areas.
Learning and improvement are fundamental to the UK-PHRST’s international activities. The Learning Review and associated report will help the UK-PHRST to better understand our partners, their opportunities and challenges, and empower us to collectively address partner identified problems - a sentiment emphasised by UK-PHRST’s Director Ed Newman.
He said: “By giving a voice to our staff and partners to capture and share some of the lessons we identified, and by being candid about the difficulties we encountered - as well as highlighting our many successes - we can continue to work well with our partners, but also learn from those lessons and grow stronger in our collaboration and in the activities we jointly undertake.”
Not only was the Learning Review an opportunity for the UK-PHRST and partners to reflect on their previous work and achievements, but it also provided a vital space for mutual and multi-directional learning and capacity strengthening outside of an emergency infectious disease outbreak situation.
Dr Maryirene Ibeto and Dr Femi Nzegwu from the UK-PHRST emphasised that: “The review highlights how by having these continuous conversations, low- and middle- income countries and support agencies like the UK-PHRST can share best practice and learn from each other constantly. This will mean that they can more effectively deal with a crisis when it hits – ultimately creating a safer and more secure global health situation for everyone.”
Read the full UK-PHRST and Partners Learning Review Post Review Reflections & Actions Report
Ongoing research projects
The UK-PHRST are currently delivering eight ongoing research projects, a selection of which are included below:
Developing a mental health and psychosocial support (MHPSS) package for infectious disease outbreaks
A collaboration between UK-PHRST and Saint Joseph University of Beirut, this research project aims to identify, through expert consensus, a list of interventions to support people’s mental and psychosocial health as part of a complex package for an infectious disease outbreak context.
As part of this project, a consultation workshop was held in Cairo, Egypt from 8-10 May 2023 hosted by the Egyptian Red Crescent (ERC). Participants, including people with lived experience from the Global Mental Health Peer Network, shared their experiences of mental health and psychosocial support (MHPSS), and experts identified barriers and facilitators for MHPSS in outbreaks. The workshop provided valuable learning allowing the project team to focus on developing MHPSS priorities with country partners.
Epidemiological and clinical review of mpox in Nigeria: A multi-disciplinary research project to inform outbreak control measures (with Nigeria CDC)
The UK-PHRST team continue to collaborate with Nigeria CDC to develop two interlocking research studies. Using a OneHealth approach, the project aims to better understand the factors behind the spread of mpox across different Nigerian states.
A UK-PHRST research team travelled to Abuja in May to finalise project details prior to the study implementation later this year. Researchers from the UK-PHRST, including colleagues from the University of Oxford also assisted Nigeria CDC colleagues to further strengthen their laboratory systems ahead of the studies. For instance, one workshop provided attendees with hands-on experience of preparing, running and analysing blood sample analysis assays as well as the transfer of scientific methods to build local skills capacity for the upcoming studies.
Completed research projects
New briefing paper flags priority research questions to improve cleaning practices in resource-limited hospital settings
The CLEAN research group, first convened in mid-2022 within a UK-PHRST project, have produced a briefing report that outlines the need for additional research work in the field of environmental cleaning in resource-limited healthcare settings. The report details their 12 recommended key research questions and associated considerations to facilitate effective hospital cleaning in resource-limited healthcare settings and to help reduce the spread of infections and antimicrobial resistance.
They hope the research priorities will encourage the eventual implementation of low-resource tailored and cost-effective cleaning practices in resource-limited settings which will benefit the health of both patients and staff and ensure a respectful environment for patients. They are now calling on funders, policymakers and advocates to drive forward implementation research into cleaning practices in these healthcare settings.
Operational research framework workshop at Africa CDC
March - Members of the research team supported the facilitation of a consultative workshop held in Addis Ababa on developing an operational research framework in emergency preparedness and response at Africa CDC. The workshop built on remote support provided by the research team in developing the concept, format and agenda in previous months. The team will continue to support Africa CDC as the framework develops.
Field Deployment Training course
This year’s Field Deployment Training (FDT) course took 18 participants on the 'journey' of pre-deployment, deployment, needs assessment, intervention recommendations and exit planning thanks to the expertise of the co-ordinators in humanitarian scenarios, health, operations and capacity strengthening.
The training, jointly delivered by UK-MED (a humanitarian health organization), UK-PHRST and UK Health Security Agency across four days in Bedfordshire, is a mandatory component for all deployable members of the UK-PHRST team to ensure they can deploy safely and effectively.
To make sure the participants would be equipped for situations, the components typical of real deployments were condensed into a micro time scale (ie. experienced across four days rather than the usual deployment of six weeks), using forum theatre techniques such as being accosted by media, being challenged for breaches in security protocol and safe-guarding issues.
Workshop on mpox antibodies detection
There was an opportunity to learn more about tools for detecting mpox at a workshop during the UK-PHRST research team’s visit to Abuja, Nigeria in March focusing on the clinical characteristics and outcomes of mpox disease in Nigeria. The MVA (modified vaccinia Ankara) ELISA assay workshop and technology transfer session was held with colleagues from the Nigeria Centre for Disease Control (NCDC) and National Veterinary Research Institute (NVRI).
The workshop, hosted by The MRC Unit The Gambia at LSHTM, included training and advice from a University of Oxford expert on how to use the MVA ELISA to detect mpox antibodies for different aspects of the study. Colleagues from NCDC – Abuja, NCDC – Lagos, NVRI – Vom, the MRC Unit The Gambia at LSHTM and the National Public Health Laboratory Gambia who attended found the workshop informative, enjoyable and worthwhile.
Caribbean collaboration visit
In March, our Director Ed Newman, was invited to meet counterparts from the Caribbean Public Health Agency (CARPHA). Together, the two organisations hope to develop a strong collaborative relationship which could include the co-deployment of staff at CARPHA’s request - UK-PHRST deploying staff to CARPHA to enhance their public health emergency response and CARPHA deploying staff outside the Caribbean to gain response experience.
The meetings were well received by the CARPHA Senior Leadership who were very keen to work further with the UK-PHRST and develop future areas of collaboration. Additionally, Anita Shah, a UK-PHRST Field Epidemiologist who had seconded to CARPHA, shared the findings of her work with the organisation regarding its Field Epidemiology and Laboratory Training programme and future expansion plans.
View our quarterly map to see our activities between January and March 2023.
Cleaners must be viewed as a key part of the health system to reduce infections and antimicrobial resistance among staff and patients, according to a report by experts from the CLEAN research group.
The group produced the briefing paper as part of a UK-PHRST project. It sets out 12 priority research questions to improve hospital cleaning and highlights the challenges facing resource-limited settings, as well as factors that need to be considered to support the implementation of tailored and effective cleaning practices. These include, for example, ensuring capacity strengthening of cleaners and the need for financial support to cement cleaning in the healthcare system.
The Group is now calling on investors, policymakers and advocates to drive forward implementation research into cleaning practices in hospitals with limited resources.
The CLEAN Group was first convened in mid-2022 within a UK-PHRST project to identify the most urgent research questions to inform or enhance the implementation of best practices in surface and non-critical equipment cleaning in healthcare facilities in resource-limited settings. It includes experts from Africa, Europe, Asia, Australia, North and South America, with expertise in infection prevention and control, hospital cleaning and disinfection, water, sanitation and hygiene (WASH), health policy, implementation science and clinical research in resource-limited settings.
Read the full blog and the CLEAN Briefing Paper on the UK-PHRST Knowledge Hub.
The UK Public Health Rapid Support Team invites you to join our new drive to evaluate the definition, value and impact of our partnerships and capacity strengthening activities.
Fill out our Market Consultation Survey to indicate your interest in the competition to receive a contract. The contract will involve conducting the evaluation and generating significant learning and understanding of our partners' perspectives, identifying challenges and how these have and can be addressed in real time over the lifespan of UK-PHRST's project cycle.
Some key considerations for the evaluation include:
Partnerships
- Understanding of the "nuance of relationship" by different partners
- The degree to which they are perceived as beneficial and equitable by the people we work with
- What factors appear to enable or detract from "ideal partnerships" –what does the much-used phrase "power dynamics" mean in our context?
- Is it constraining in crafting equitable and useful partnerships?
- Does it play a facilitative role, or is it neutral in its perception by partners?
- What impacts have our partnerships had?
Capacity strengthening
- How can we gauge a deeper understanding of capacity strengthening in the context of UK-PHRST's work?
- What are the impacts realised by partners in their work with the UK-PHRST?
Information session
For more information, please join us online at our Market Engagement Session on 15 December 2022 at 10:00 am GMT. Join here
In order to be considered, please complete the Market Consultation Survey here.
This should be completed by the supplier or a partner or an authorised representative in his / her own name and on behalf of the company / organisation completing this questionnaire.
Registration is free and open to all. The deadline to complete the survey is 13 January 2023.
More information
Find out more
For further information, please refer to the documents attached, including:
download Attachment 2 - How to Bid including Evaluation Criteria v1.0.pdf
download Attachment 1 - About the Procurement Competition v1.0.pdf
download Market Consultation Survey - Evaluation of UK-PHRST Partnerships Capacity.docx
download Pre-sourcing event Zoom meeting invite link.docx
Please contact Zahra.Bhatti@ukhsa.gov.uk if you have any questions.
The UK Public Health Rapid Support Team and partners are currently working on seven research projects, and we have also developed our Research Plan for 2022-2025. Within the plan, we have described 17 new cross-discipline research projects that were co-identified and will be co-led with low-and-middle income partners, and three of these have recently started. Projects in the plan have been grouped into themes covering preparedness and prevention, detection, response, and impact and evaluation, however, the plan also enables flexibility to begin new projects that address urgent research questions arising during outbreaks or during deployments. Most of the 14 projects yet to be approved by Technical Steering Committee (TSC) are expected to be reviewed and begin over the next six months.
We are also delighted to announce a new research collaboration on Monkeypox with the Nigeria Centre for Disease Control, University of Oxford and partners. This new collaboration will cover key priorities in Monkeypox research in Nigeria and will have clinical, epidemiological, One Health, laboratory, and social science components. Priorities for the Monkeypox research programme were identified during a workshop in Abuja in August 2022, during which participants proposed several multi-disciplinary studies with Nigerian leads. The group also recommended strengthening laboratory operations at Nigeria CDC in preparation for the research, and this work is currently underway. The Monkeypox research programme is included in our research plan.
Among our currently running studies, one is developing an early warning system that can identify “hot spots” in remote regions of Guinea where Marburg virus outbreaks are likely, based on interactions between human and bat populations. In recent months, the study team have completed a community sensitisation (awareness raising) and a risk communication campaign across study villages in Macenta, led by the Guinean project lead in collaboration with a local NGO. They have also collected pilot data for surveillance tools from study villages and generated preliminary biodiversity indicators and machine learning algorithms. The next stage of the project will include in-depth investigations of zoonotic exposure and bushmeat hunting practises among the target population using qualitative methods.
Since the last research update, three research projects have been completed, including two Infection Prevention and Control (IPC) studies and a pilot study of a non-whole genome sequencing approach for monitoring SARS-CoV-2 variants in Burkina and Kenya. Find out more below.
Development and evaluation of resources to support IPC engagement with caregivers in hospitals
This study, which began in February 2021, aimed to develop and evaluate resources to support informal caregivers in Cameroon to engage with IPC . The project was co-led by the UK-PHRST and Cameroon Baptist Convention Health Services (CBCHS) in partnership with the Infection Control Africa Network (ICAN), the not-for-profit visual resource charity Medical Aid Films (MAF) and the Africa Task Force for Corona Virus Response (AFTCOR) IPC technical working group.
Thee study described the role and function of caregivers in a tertiary referral hospital in Cameroon, developed training resources to support their engagement with IPC, including context-appropriate audio-visual materials, piloted delivery of a multimodal intervention, and evaluated the effectiveness of the intervention.
The evaluation demonstrated the feasibility of delivering the intervention in the health system and that it was well-received by caregivers and health workers. Six local research assistants were also trained. The study findings have been and are being shared with all relevant stakeholders, including ICAN, MAF, Africa Centres for Disease Control and Prevention (Africa CDC), and the Cameroon Public Health Institute. The study team plans to present the findings at the bi-annual ICAN conference in 2023 via partner networks and in an open access, peer reviewed journal. The team will support further engagement of informal caregivers with a ‘toolkit’ of resources that will be transferable to other LMIC healthcare settings.
What is the current level of cleaning in LMIC health systems and what interventions are effective at improving it?
Formal training for cleaners in health settings may be inadequate in many LMICs and is of particular concern during outbreaks when there is additional urgency for rapid interventions.
In this study, the team led a systematic review of cleaning interventions in LMIC health settings and convened a workshop with diverse international stakeholders to develop recommendations and a roadmap of future research priorities. Stakeholders included leading IPC researchers in Africa, Asia and high-income countries, and representatives from public health institutes, relevant networks and the World Health Organization.
Unsurprisingly, most evidence from LMICs came from areas with greater resources, such as tertiary referral centres in large cities. Standard outcome definitions for cleanliness were found to be lacking, and results were reported inconsistently, hampering the synthesis and meta-analysis of aggregate data. Preliminary systematic review findings have been presented in a Webber teleclass and are being submitted for presentation to the ICAN conference and International Conference on Infection Prevention and Control in 2023. A blog and research prioritisation paper have been submitted to The Global Health Network, and the systematic review will be submitted for publication in a peer-reviewed journal.
A non-whole genome sequencing approach for monitoring SARS-CoV-2 variants in Burkina Faso and Kenya
This study, which started in November 2021 and was a collaboration between UK-PHRST/LSHTM and Groupe de Recherche-Action en Santé in Burkina Faso (GRAS), Kenya Medical Research Institute (KEMRI), MRC Unit Gambia (MRCG) and Liverpool School of Tropical Medicine (LSTM), aimed to understand the feasibility of running the HRM assay in LMIC settings through pilots in Burkina Faso and Kenya. These sites were selected because the research team had established partnerships through the Gates Foundation-funded Malaria as a Risk Factor for COVID-19 (MALCOV) SStudy. UK-PHRST Rapid Research funding enabled the team to leverage real-time access to MALCOV study specimens.
The study team developed and updated their high-resolution melt (HRM) assay in response to the emergence of new SARS-CoV-2 VOCs. Following training, researchers from Burkina Faso and Kenya analysed samples using the assay at laboratories in The Gambia and Kenya and validated assay performance against whole genome sequencing (WGS). This project demonstrated the utility of a non-WGS method in lower resource settings for tracking SARS-CoV-2 variants and may provide a lower-cost approach for understanding molecular epidemiology in settings where access to WGS is absent or limited. The project built new and developed existing collaborative working relationships between researchers from LSHTM, Groupe de Recherche Action Santé (GRAS), Kenya Medical Research Institute (KEMRI), MRC Unit The Gambia at LSHTM (MRCG) and Liverpool School of Tropical Medicine (LSTM). The findings have been presented at LSHTM and external meetings and conferences. One peer-reviewed article is nearing publication in the Scientific Reports journal, and a further article will be submitted in December 2022. Find out more about the field visit to The Gambia here.
In the coming months, the UK Public Health Rapid Support Team (UK-PHRST) will focus on establishing a refreshed and enhanced capacity strengthening pillar. Dr Claire Bayntun has been appointed to lead this work as the Head of Capacity Strengthening and will expand the team to take forward new strategic spheres of opportunities, reflecting the values of the UK-PHRST and aiming to secure trusted, sustainable partnerships for the future.
View UK-PHRST's capacity strengthening pillar
Over the last quarter, the UK Public Health Rapid Support Team (UK-PHRST) conducted eight capacity strengthening activities, including a learning review in Cape Town, South Africa, and R training* in Ethiopia and Nigeria, respectively.
*R is an open-source software environment for statistical computing and is used for data analysis and visualisation.
In September, we met with many of our partners in Cape Town, South Africa, to reflect on our working practices and exchange lessons on improving outbreak response, research and capacity strengthening. Experts at UK-PHRST co-led sessions on gender equity, capacity strengthening, policy and practice in research, outbreak response and equitable partnerships. These discussions will inform a summary of recommendations and actions we can implement to enhance our equitable partnerships and foster sustainable ways of working.
Watch the highlights of the learning review
R Training
UK-PHRST facilitated R-Training with Africa Centre for Disease Control and Prevention in Ethiopia in July, capturing lessons learned to strengthen future training, planning and delivery. The UK-PHRST epidemiology team co-facilitated two workshops with the African Volunteer Health Corps (AVoHC). This included prioritising key programme activities for 2022-23, reviewing and refining content for an induction course, and training new AVoHC roster members.
Equitable partnerships with infection prevention and control (IPC) stakeholders
The infection prevention and control (IPC) team shared preliminary results for developing and evaluating resources to support a study with Cameroonian partners in July. It delivered a workshop with key global stakeholders reviewing evidence and prioritising research needs for cleaning and disinfection interventions.
The team is contributing to reviewing a World Health Organization course for environmental cleaning and infection prevention control. The team is supporting the WHO Emergencies IPC team, offering technical support for Ebola and Monkeypox, and developing specific IPC implementation tools, including an IPC outbreak implementation package and updated IPC assessment tools will be provided in addition.
Mental health
As part of the Strengthening Public Mental Health in Africa in response to COVID-19 (SPACE) programme’s phase two delivery, the team involved representatives from Sierra Leone and Cameroon in a workshop in Liberia with partners Africa Centre for Disease Control, World Health Organization Regional Office for Africa (WHO AFRO), WHO Regional Office for the Eastern Mediterranean (WHO EMRO), West Africa Health Organisation (WAHO), and East Central and Southern Africa Health Community (ECSA-HC).
We have summarised the latest UK-PHRST deployment, research and capacity development activities from July – September 2022 in a quarterly map. Many of our activities across the triple remit overlap, and some will continue into the next quarter. The map demonstrates ongoing or completed activities during the quarter, and the year stated is when the project commenced.
The Strategic Framework 2022 to 2025 sets out UK-PHRST’s objectives to build on the commitment, impact and effectiveness of the past six years of our operations.
The UK-PHRST strategy is underpinned by three principles: learning, partnerships and impact. It outlines how the UK-PHRST will deliver on this commitment through activities across the triple remit in outbreak response, research and capacity strengthening.
On the week that the UK Public Health Rapid Support Team (UK-PHRST) celebrates its 6th sixth year anniversary, and with staff currently deployed to the Ebola outbreak in Uganda, UK-PHRST Director, Dr Ed Newman, shares the team’s ambitions for the next three years and our continued commitment to respond to disease outbreaks in the countries we work with.
Published by the UK Health Security Agency. Read more.
We are an innovative partnership between the UK Health Security Agency and the London School of Hygiene & Tropical Medicine, funded with UK aid by the UK Department of Health and Social Care.
In celebration of World Field Epidemiology Day on 7 September, the UK Public Health Rapid Support Team spoke to UK Field Epidemiology Training Program (UK-FETP) fellows Megan Bardsley and Mona Dave, who recently deployed with the UK Public Health Rapid Support Team (UK-PHRST). Field epidemiologists support the UK-PHRST to prevent and control infectious disease outbreaks, before they develop into global emergencies. The UK Field Epidemiology Training Programme recruits seven to eight UK-FETP fellows a year.
Megan Bardsley
Megan completed her undergraduate degree in biological sciences and studied an MSc in Control of Infectious Diseases at the London School of Hygiene & Tropical Medicine. She is in her second year of the Field Epidemiology Training Programme based in Field Service South West with the UK Health Security Agency (UKHSA). Before joining UK-FETP, she had prior experience in UKHSA’s human immunodeficiency virus / sexually transmitted infections (HIV/STI) department, worked as a research assistant at LSHTM and gained experience in Malaysia at a breastfeeding NGO. She recently deployed with UK-PHRST to Papua New Guinea via the Global Outbreak Alert and Response Network.
Mona Dave
Mona gained an undergraduate degree in biomedical sciences at Warwick University, and a Master's in Public Health with International Health at the University of Nottingham. She began her journey into global health after spending three months in the Philippines on a health education programme with the Voluntary Service Overseas (VSO) as part of the International Citizen Service (ICS) in 2013. Before joining the UK-FETP, she worked as a research assistant in non-communicable disease research at Newcastle University and as a scientist in the South West Field Service. Mona recently deployed with UK-PHRST and is currently based at a training site at UKHSA's Midlands Field Service.
What is epidemiology?
How do epidemiologists contribute to outbreak response?
Megan: Responding to an outbreak of disease in epidemiology involves providing and interpreting data to understand the severity of the situation, affected groups, what people are being infected by, and the impact and burden. You then highlight particular risk factors and groups that need targeting for intervention. One key role of the epidemiologist in an outbreak is getting everybody to agree on the case definition.
Mona: Contributing to regular disease surveillance allows us to understand 'normal' patterns and trends of disease spread. In other words, we can spot, investigate, and act when something looks out of the ordinary. Descriptive epidemiology (describing a disease in time, person and place) and analytical epidemiology (conducting statistical analysis to test a hypothesis) can explain how an infection might spread. However, you may not always know the true cause. As an epidemiologist, being able to interpret findings, make evidence-based recommendations and tailor these to your audience can help to ensure recommendations are actioned by the right stakeholders and, therefore, control further infections from spreading.
What does the role involve?
Megan: It involves working with many different people and using your technical expertise and scientific background to identify trends in surveillance data and present the strengths and limitations to various stakeholders. When investigating a public health outbreak, I am responsible for managing the data, writing code to analyse the data, and working with people to identify and describe cases and do detective work to investigate the source.
Mona: I support UKHSA's Midlands Field Service infectious disease surveillance and outbreak response work as part of a rota. This can involve producing or reviewing epidemiological summaries, attending outbreak control meetings and providing feedback and recommendations. I also work on specific projects that enable me to enhance existing and develop new skills while meeting my UK-FETP competencies.
What is a highlight of your job?
Megan: I worked on an investigation into an outbreak of Salmonella where I rang patients to complete questionnaires and conducted an analytical study, also known as a case-control study. Secondly, I enjoy being part of a global epidemiology network - it's a community of people who are interested in the spread of infectious diseases and you learn from people across the world.
What challenges do you experience in your role?
Megan: I think a lack of awareness of epidemiology can be challenging as some of the fantastic work we produce can go unacknowledged. I think increased awareness of epidemiology will attract more people who are interested in helping people through the use of science.
What led you to apply for UK-FETP?
Mona: As challenging as it was, contributing to the COVID-19 response, seeing the impact and working alongside dedicated individuals is incredibly rewarding. That was when I realised I wanted to continue working in and developing my skills in this field, and I applied for the UK Field Epidemiology Training Programme (UK-FETP).
About UK-FETP
The United Kingdom Field Epidemiology Training Program (UK-FETP) was founded in 2011 as a program associated with the European Program for Intervention Epidemiology Training (EPIET), and it was accredited by TEPHINET in the first accreditation round. Since EU-Exit the UKFETP has run as an independent programme for the UK.
About UK-PHRST
The UK-PHRST is an innovative partnership between the UK Health Security Agency and the London School of Hygiene & Tropical Medicine, funded with UK aid by the UK Department of Health and Social Care.
The UK Public Health Rapid Support Team (UK-PHRST) and partners are currently delivering nine research projects, including two new studies bolstering UK-PHRST's research in outbreak preparedness and response:
- 'A novel One Health approach to develop an early warning system to improve preparedness for and response to Marburg virus disease outbreaks'. This innovative study combines serological sampling of humans and Marburg virus detection from faecal bat samples to confirm target populations and uses remote audio-monitoring devices (AudioMoth) to assess humans and bat population interaction in target regions in Guinea. The team will use these findings to develop an early warning system to allow public health systems to recognise MARV outbreak threats with greater precision and prepare response measures tailored to affected areas. The study is being co-delivered with University of Oxford, the National Viral Haemorrhagic Fever Reference Laboratory, Guinea and MRC Unit The Gambia at the London School of Hygiene & Tropical Medicine (LSHTM).
- 'A novel early warning system involving local community leaders for early detection of health-related events indicative of outbreaks: A pilot in Cape Verde and Brazil'. This project, a collaboration between Brasília University, the Ministry of Health in Cape Verde and the UK-PHRST, investigates whether an event based surveillance (EBS) system - developed with and relying on the participation of community leaders - is more effective at detecting infectious disease outbreaks than indicator-based surveillance or centralised EBS systems. The study team will focus on two contrasting outbreak prone lower middle-income countries (LMICs), Cape Verde and Brazil, respectively.
In other active studies in the UK-PHRST portfolio, the project team delivering a pilot of a non-whole genome sequencing approach for monitoring SARS-CoV-2 variants in Burkina Faso conducted a successful research and laboratory visit to MRC Gambia Unit The Gambia at LSHTM in July 2022. See further details of the visit. The team had needed to move sequencing and assay development to two new sites, at MRC Gambia and Kenya, following a coup in Burkina Faso earlier in the year. The project team will submit a final report in October.
The study 'Rapid response molecular diagnostics for Crimean-Congo Haemorrhagic Fever (CCHF)', which aims to assist the economic development and welfare of CCHF endemic populations in LMICs, particularly those in marginalised areas with limited laboratory capacity, conducted its final visit to the Ministry of Health virology laboratory in Turkey in June 2022. A UK-PHRST-hosted CCHF workshop in September 2022 is in preparation to disseminate results to key stakeholders.
The UK-PHRST also convened a two day hybrid research workshop in June 2022 in partnership with Stellenbosch University as part of the UK-PRHST study investigating 'evidence on levels of, and interventions to improve, healthcare cleaning in low-and middle-income countries. Over 30 regional and international organisations attended, including experts in water, sanitation and hygiene (WASH), Infection prevention and control (IPC) and environmental hygiene. A report and roadmap are currently in preparation and will be published in due course as outputs.
A closing ceremony for the IPC Caregivers study in Cameroon, which focused on the development and evaluation of resources to support IPC engagement with caregivers in LMIC hospitals, was held at Banso Hospital on 24 June 2022 to mark the contribution of the research team and the conclusion of field research. As part of the study, a series of IPC instructional/orientation animated videos were developed in partnership with Medical Aid Films and designed for caregivers of patients. See the animations in English and in Pidgin. A short version of the film was also produced. The project team are writing the final project report currently, and will also present findings within the Infection Control Africa Network (ICAN) webinar series and at the upcoming Global Health Network Conference.
Three research projects have also been completed since the last research update. These include the study which examined excess mortalities associated with COVID-19 in The Gambia, as well as two rapid studies; one to improve the application of oral fluid filovirus surveillance methods in Africa, and one focused on the development of mental health and psychosocial support (MHPSS) in outbreak preparedness and response in Africa.
The study team investigating excess mortality in The Gambia associated with COVID-19 and other causes concluded there was an unexpected decline in recorded mortality during the COVID-19 pandemic, but that mortality rates increased in the second wave and reached excess mortality of 22.6 per 100,000 compared to 2016-2019. Foetal complications constituted the highest proportion of deaths, while sepsis, COVID-19 and stroke were also important. A report written by UK-PHRST, MRC Unit The Gambia at LSHTM and Ministry of Health Gambia has been shared with regional health centres and health facilities participating in the study. Results will also be disseminated through a policy briefing, Ministry of Health meetings, and presentations at national and regional meetings.
The second completed study, conducted in partnership with University of Oxford and the Fondation sante et développement durable (FOSAD) Guinea, set out to understand if the Lola population in Guinea exhibited signatures indicative of non-Ebola filovirus infections that impact upon individual and population-level seroepidemiological inference, and if so, if this information could be used to refine strategies for both oral fluid and serum-based seroepidemiological investigations in filovirus-endemic LMICs in Africa. The study demonstrated that oral fluid samples showed discordant responses with blood and concluded that at population scale, and despite prior validation of the assay in an Ebola virus survivor cohort, surveillance for Ebola virus and likely other filoviruses appeared unfeasible with oral fluid-based assays due to insufficient specificity. These limitations are important for public health professionals and researchers using oral fluid tools for the surveillance of filoviruses as they were widely used during and after the outbreak of Ebola in West Africa and have been suggested as more acceptable tools for surveillance in endemic settings. Results from the study were disseminated in Guinea through the national health security agency (ANSS), who lead operations and research strategy related to emerging infectious diseases including filoviruses. The study highlights the limitations of relying on oral fluid based surveillance for filoviruses and suggest dried blood spot (DBS) based sampling as a viable alternative.
The study ‘Evidence to practice: research and capacity development for mental health and psychosocial support (MHPSS) in outbreak preparedness and response in Africa: SPACE 2.0’, sought to support national actors in Liberia, Sierra Leone, Cameroon and Nigeria prone to outbreaks to integrate mental health interventions in emergency preparedness and response (EPR). An umbrella review on the effectiveness of mental health and psychosocial support (MHPSS) interventions during infectious disease outbreaks was conducted, and a hybrid workshop was held in Liberia which brought together mental health experts from African public health institutions. This included World Health Organization Regional Office for Africa (WHO Afro), Africa Centres for Disease Control and Prevention (Africa CDC), West African Health Organization (WAHO), East, Central and Southern Africa Health Community (ECSA-HC) and mental health leaders in Liberia, Sierra Leone, Cameroon, and Nigeria to share expertise and develop a theory of change (ToC) for integrating mental health into national EPR plans. Capacity building activities included introducing the newly developed Minimum Services Package for MHPSS in emergency response, and related MHPSS resources. The UK-PHRST mental health consortium convened a further webinar on 18 May 2022 at which results from the study were shared, and next steps discussed, including:
- How best to facilitate sharing expertise and lessons learned from different countries responses to the COVID-19 pandemic and other emergencies
- How to further improve and refine the ToC for MHPSS integration into emergency response
- Identification of research and capacity strengthening priorities for the next phase of the consortium’s work.
We have summarised the latest UK-PHRST deployment, research and capacity development activities from April – June 2022 in a quarterly map. Many of our activities across the triple remit overlap, and some will continue into the next quarter. The map demonstrates ongoing or completed activities during the quarter, and the year stated is when the project commenced.
View the UK-PHRST quarterly map
The UK-PHRST team and partners are currently delivering 11 research projects, including two new studies:
- ‘Integrating Social Science into Africa CDC’s Public Health Operations’, which examines the status and use of social science at Africa CDC and how it can be further integrated into public health preparedness and response.
- ‘What is the current level of cleaning in LMIC health systems and what interventions are effective at improving it?’ which strengthens UK-PHRST's research in Infection Prevention and Control (IPC) and environmental hygiene and aims to improve the evidence base for cleaning implementation and investment in cleaners, a vulnerable and neglected group in the health system in many Lower Middle-Income Countries (LMICs).
We are also delighted to welcome Nasser Fardousi to the UK-PHRST, who joined us as a Research Fellow in Environmental Hygiene in January. Nasser is working with the IPC team, investigating the current level of cleaning in LMIC health systems and what interventions are effective at improving it.
We have several research projects that are concluding. These include two rapid research studies, one of which aims to improve the application of oral fluid filovirus surveillance methods in Africa, and the other to develop mental health and psychosocial support (MHPSS) in outbreak preparedness and response in Africa. The team investigating the extent of excess mortality in health facilities in The Gambia associated with the COVID-19 pandemic is also in the final stages of writing up their results.
In February, as part of the MHPSS study, the team delivered a workshop in Liberia in partnership with Africa CDC hosted by the Liberian Ministry of Health. The workshop brought together a consortium of mental health experts from African public health institutions to share experiences and lessons learned from COVID-19 and other crises in the region. The workshop also mapped out processes for strengthening MHPSS in outbreak preparedness and response in Africa.
A military Coup in Burkina Faso in January 2022 threatened to affect the delivery of the rapid study piloting a non-whole genome sequencing approach for monitoring SARS-CoV-2 variants in Burkina Faso, however, the team were able to move sequencing and assay development to The MRC Unit The Gambia at the London School of Hygiene & Tropical Medicine and a new field site in Kenya.
Our study on COVID-19 vaccine strategies implementation in partnership with Gates Exemplars in Global Health has been published online and will soon be published in French. Read more here.
The research management team are also preparing the programme’s six-month report for National Institute for Health and Care Research (NIHR), including quarterly and annual finance reports.
Our newly developed research strategy for 2022-2025 is currently in review by our key stakeholders. The strategy has been informed by an evidence gap analysis complemented by stakeholder interviews and feedback from partners and formal reviews and aims to deliver a coherent, structured, partner-led research programme informed by public health need.
We have summarised the latest UK-PHRST deployment, research and capacity development activities from January – March 2022 in a quarterly map. Many of our activities across the triple remit overlap, and some will continue into the next quarter. The map demonstrates ongoing or completed activities during the quarter, and the year stated is when the project commenced.
View the UK-PHRST quarterly map
We are looking for an external consultant with ethnographic experience, public health, outbreaks training or experience, and experience working within or closely with Ministries of Health, National Public Health Agencies, or relevant multilateral bodies.
This consultant will support the UK-PHRST in conducting an institutional ethnography of Africa CDC, to support the development of a social science integration strategy and roadmap within the organisation; to conduct analysis of data collected; to write up operational and academic findings in partnership with Africa CDC.
Skills and experience:
- Relevant PhD or MA/MSc
- Social science training and substantial experience with primary data collection of qualitative data
- Project management skills
- Ability to work independently and as part of a team
- Excellent written and verbal English language communication skills
- Confident presentation skills
Preferred start date: 15 April 2022
Expected duration (days): 84 days
Expected hours per day: 7. Flexible working patterns can be considered during the project’s analysis phase.
Daily rate: £350-500/day, dependent on skills/experience
Interested candidates should submit their CVs and a cover letter outlining how they are suitable for the role, along with their expectations for a daily rate. Please send these to Hana.Rohan@lshtm.ac.uk and Thom.Banks@lshtm.ac.uk.
The UK-PHRST team and partners are currently working on ten research projects, two of which have newly started since our last quarterly newsletter:
- a rapid systematic review, building on the UK-PHRST infection prevention and control (IPC) caregivers study, of the evidence on the levels of, and interventions to improve, cleanliness in health facilities in LMICs and specifically relating to outbreak preparedness and response.
- a rapid study to validate and improve the application of oral fluid-based immunoassays for filovirus surveillance in West and Central Africa, building on previous UK-PHRST research on Ebola Virus immunoassays.
The team have also recently completed two research projects. One of these explored how serosurveillance of healthcare workers might be used to strengthen viral haemorrhagic fever preparedness in Uganda. The findings suggested that increased PPE training is needed to increase awareness and reduce potential exposure to Ebola Virus (EBOV) in healthcare workers and to Rift Valley Fever in abattoir workers. The other investigated the feasibility of using oral fluid-based anti-EBOV immunoassays to identify previously undetected EBOV infections in Guinea. It provided strong evidence that this approach can detect previously unidentified EBOV exposures many years after infection and demonstrated its feasibility in targeted surveillance and preparedness activities where EBOV is endemic.
In our last research update in July, we shared the collaborative research project with Gates Ventures that explored the barriers, enablers, and lessons from the previous implementation of vaccines during epidemics in LMICs that can be applied to COVID-19. The findings of this research were presented in our latest webinar on COVID-19 vaccination in low and middle-income countries: lessons from past and current campaigns.
We are also in the process of developing our new 3-year research strategy. This work is being informed by an evidence gap analysis to identify key areas where evidence from impact evaluations and systematic reviews in outbreak prevention, detection and response in LMICs is most limited. This resource is being complemented by stakeholder interviews and together these efforts will provide a strategic approach for identifying our research priorities in the coming years. We hope to provide more details on our new research strategy in the next research update.
We are seeking an outstanding Research Fellow or Assistant Professor to support the UK Public Health Rapid Support Team (UK-PHRST). The post-holder will contribute epidemiological and analytical expertise to support UK-PHRST’s strategic objectives in outbreak response, operational research, and capacity building, working in partnership with local and regional stakeholders. The role will also include representing the UK-PHRST at relevant external events, conferences and workshops.
The UK-PHRST is a collaborative partnership between the London School of Hygiene and Tropical Medicine (LSHTM) and Public Health England (PHE) that rapidly deploys a team of multidisciplinary public health professionals and researchers on behalf of the UK Government to areas of need in low and middle-income countries (LMICs). Application details here.
Deadline: Tuesday 28 September
Between September and November 2020, Itad conducted a number of Key Informant Interviews with stakeholders to gather evidence for the end-point evaluation of the UK Public Health Rapid Support Team (UK-PHRST) programme.
The purpose of the evaluation is to ensure independent monitoring and quality assurance of programme delivery, documentation of lessons learned, and robust tracking of results, providing assessment of the effectiveness of official development assistance (ODA) funds.
We are delighted to share these with you;
We are delighted to announce that Dr Ben Gannon has been appointed as the Interim Director of the UK Public Health Rapid Support Team (UK-PHRST). Ben has taken over the role from Professor Dan Bausch, who has accepted a post as Director of Global Health Security at the Foundation for Innovative New Diagnostics in Geneva. We would like to take this opportunity to thank Dan for his leadership of the UK-PHRST over the past four years.
Ben has worked in the UK-PHRST as the Microbiology Lead for the last five years, deploying on multiple occasions and building an extensive portfolio of overseas research and capacity development projects. He comes from an academic background, including specialising in zoonotic disease transmission and diagnostics at the University of Bristol. Later he joined the PHE Rare and Imported Pathogens Laboratory where he deployed to Sierra Leone on multiple occasions to support the Ebola diagnostic laboratory programme. Ben’s appointment is strongly supported by the Department of Health and Social care, as well as Public Health England and the London School of Hygiene & Tropical Medicine, the joint lead UK-PHRST partner organisations.
We are confident that the UK-PHRST is in excellent hands at this critical time.
Adapted by UK-PHRST staff, Dr Alice Walker, this course shows front-line responders how to recognise when people affected by the COVID-19 pandemic are in distress, and how to provide them with Psychological First Aid (PFA). It is specifically designed for first responders in Africa and reflects the different healthcare situations of African countries, drawing on guidance from the World Health Organisation and the United Nations, and has been adapted for the context by the UK-Public Health Rapid Support Team (PHE/LSHTM) with input by experts from WHO AFRO, WHO EMRO, Africa CDC, the West African Health Organization, and the East, Central and Southern Africa Health Community (ECSA-HC).
We are seeking an outstanding academic leader to serve as Deputy Director for Research for the UK Public Health Rapid Support Team (UK-PHRST). The post-holder will oversee and deliver the UK-PHRST research programme, building the evidence base for international disease outbreak response and interventions. The UK-PHRST is a high-profile collaboration between the London School of Hygiene and Tropical Medicine (LSHTM) and Public Health England (PHE), with a 5-year £20m grant from the UK government to support a triple mandate of outbreak response, outbreak-related research, and capacity building in low and middle-income countries (LMICs). Application details here.
Deadline: Sunday 03 January
Prof Bausch has served on ASTMH’s executive committee as scientific program chair for the last six years, and was recently voted President-elect by the society’s members. ASTMH is the largest international scientific organisation of experts dedicated to reducing the worldwide burden of tropical infectious diseases and improving global health. Prof Bausch will serve a three-year term comprised of one year each as President-Elect, President, and Immediate Past-President.
As president, he will be responsible for steering the important work of ASTMH, which includes generating and sharing scientific evidence, informing health policies and practices around the world and advocating for investment in tropical medicine and global health research.
Prof Bausch said “I feel so fortunate to be elected to lead such a great and talented group of people at ASTMH who are so dedicated to making the world a better place. Furthermore, being based in London and engaging with the Royal Society over the past few years, I’m excited about the potential for ASTMH-RSTMH collaborations.”
Read the full story here.
The UK Public Health Rapid Support Team (UK-PHRST) is conducting an online survey (until 25th October 2020) open to public health and healthcare professionals worldwide to understand their professional assessment of current and future COVID-19 interventions, specifically the practicality of, and barriers to, implementation in their context.
Your participation is important to share learning to inform the COVID-19 response in your country and in others. The survey is available in English, French and Portuguese and is anonymous.
For more information on how to complete the survey, please click here.
Please help to share this with relevant professionals - many thanks for your valued support!
The UK-PHRST are pleased to announce the launch of their new Knowledge Hub, where practitioners and researchers can find and share the most useful information for their work in outbreak response. Hosted on The Global Health Network, the Knowledge Hub aims to:
- Bridge the gap between the fast-paced world of online discussion forums and maintain long-term access to useful resources.
- Share up-to-date research and policy, as well as a dedicated education and training area with resources to support learning and inform effective outbreak response.
- Connect UK-based researchers with specialists in LMICs, creating a flow of information exchange and localised adaptations to outbreaks.
The new UK-PHRST Knowledge Hub provides a community function, allowing members to start group conversations around key topics, such as this timely post on contact tracing technology and comment on current issues, as shown in this blog on the importance of looking after Mental Health in COVID-19
We look forward to you joining, contributing and using our Knowledge Hub as a reliable and up-to-date source on outbreak response! Please do give us feedback on how you would like to see the UK-PHRST Knowledge Hub evolve in our discussion forum here.
Welcoming Ashley Sharp, a medical doctor before moving into public health and completing the UK Public Health Specialty Training Programme and the UK Field Epidemiology Training Programme (FETP).
He has worked in a variety of public health roles at local, regional, national and international levels in the UK, Eswatini, Sierra Leone, Haiti and Bangladesh, with a focus on health protection and health systems development. He is also a member of the UK Faculty of Public Health, the standard setting body for public health specialists within the United Kingdom.
Ashley joins the team as the Senior Epidemiologist and Deputy Director for Operations, replacing Olivier le Polain.
The UK-PHRST notes that April 28th 2020 marks 20 years since the inception of the Global Outbreak Alert and Response Network (GOARN). For 20 years GOARN has facilitated and promoted partners to work together in tackling disease outbreaks across the world and by doing so, ensuring that the response can be greater than the sum of its parts. We congratulate GOARN for two decades of dedicated service, making the world a safer place. The UK-PHRST is proud to support GOARN, both through deployments in the field and strategic support through membership on the GOARN Steering Committee.
The UK-PHRST deploys specialist experts to outbreaks of infectious diseases overseas, to help increase and improve the response and reduce their risk of becoming global threats. As COVID-19 has shown, diseases don’t respect borders. In February and March the UK-PHRST deployed, both through GOARN and bilateral agreements, to combat COVID-19, working alongside colleagues from the World Health Organisation (WHO), Ministries of Health and others in the WHO Western Pacific Regional Office in the Philippines, WHO Country Office in Nepal, Nigeria CDC, and Africa CDC in Ethiopia to deliver expertise in epidemiology, data analysis, infection prevention and control, clinical care, laboratory diagnostics, social science, logistics, and strategic guidance.
Although global travel restrictions have now necessitated recalling all personnel back to the UK, the UK-PHRST continues to provide support remotely to the aforementioned partners, as well as to the WHO African Regional Office in the Republic of the Congo and WHO Country Office and Ministry of Health in Bangladesh. In addition to their support to partners overseas, many UK-PHRST team members are also supporting the domestic response, providing clinical care and epidemiologic support. The UK-PHRST is also engaged in developing and implementing several research projects on COVID-19 and has organized a Massive Open Online Course (MOOC) on COVID-19 through LSHTM, which has nearly 200,000 registrants.
At any time, an emerging, lethal, and highly transmissible pathogen might pose a risk of being spread globally because of the interconnectedness of the global population.1, 2 Emerging epidemic threats are occurring with increasing scale, duration, and effect, often disrupting travel and trade, and damaging both national and regional economies.3, 4 Even geographically limited outbreaks such as the Ebola virus disease in Africa might have a global effect.
The UK-PHRST has been working closely with the Nigeria Centre for Disease Control (NCDC) to improve knowledge on Lassa fever by identifying other pathogens that may be causing similar illnesses. A recent Weekly Epidemiological Report from NCDC features an update on this work, which is taking place at the NCDC National Reference Laboratory.
It's hoped the work could lead to improved patient care, better surveillance data, and will inform public health policy. As well as broadening the scientific knowledge base on the topic, this collaboration is supporting the growth of in-country capacity for genetic sequencing in Nigeria and leadership by local experts.
Experts from the UK Public Health Rapid Support Team have contributed to a new Massive Online Open Course (MOOC) from the London School of Hygiene & Tropical Medicine.
This course is for those interested in, studying or working in global and public health. This includes government stakeholders; health practitioners and NGO employees - particularly those working in countries regularly affected by infectious disease outbreaks.
Recent outbreaks of emerging and re-emerging infectious diseases have shown we need to be able to coordinate responses to disease outbreaks at the regional, country and global level. On this free course, participants will explore disease outbreaks, discovering what outbreaks are and why they matter as well as the different responses to such outbreaks. They will also consider the future of outbreak preparedness.
Public health specialists from the UK Public Health Rapid Support Team are supporting the Democratic Republic of Congo to tackle the country’s Ebola outbreak as it reaches the one-year mark.
Those deploying to the country include a data scientist, an expert in tracking outbreaks (epidemiologist), and an infection and prevention control expert who will work with local scientists. The deployment is at the request of the World Health Organization’s Global Outbreak Alert and Response Network following the recent decision to declare the outbreak a Public Health Emergency of International Concern.
In her final annual report before leaving the role, Dame Sally Davies – Chief Medical Officer, England, and Chief Medical Advisor to the UK – chose to ‘address the UK’s engagement with health at a global level’. Her report showcases the work of the UK Public Health Rapid Support Team and includes a case study of the team’s work to support Nigeria in tackling Lassa Fever.
Q&A with UK-PHRST’s Dr Olivier le Polain.
Olivier le Polain is the senior epidemiologist and deputy director for operations of the UK Public Health Rapid Support Team.
He has been a member of the team for just under two years and in that time has deployed to Madagascar to respond to an outbreak of pneumonic plague, to Bangladesh amidst the Rohingya refugee crisis and most recently to the Democratic Republic of Congo. The latter was to support the response to two consecutive Ebola virus disease (EVD) epidemics, one in Equateur Province (May – July 2018) as well as the ongoing large outbreak which has affected the Eastern provinces of North Kivu and Ituri since August 2018.
Olivier talks about his experience on the ground in the DRC during the ongoing Ebola epidemic, the importance of working in partnership with other countries and organisations and his experience on the UK-PHRST so far.
A new online resource which aims to strengthen the control response to disease outbreaks has been developed by the London School of Hygiene & Tropical Medicine (LSHTM) and the Institute of Development Studies. The Epidemic Response Anthropology Platform is funded by the UK-PHRST and will work with, and build, networks of anthropologists and other social scientists with regional or subject expertise, and connect them to policymakers, scientists and humanitarian response workers involved in responding to epidemics.
On 8 May 2018, the Democratic Republic of Congo (DRC) Government declared a new outbreak of Ebola Virus Disease (EVD)—the country’s ninth outbreak. The UK-PHRST is deploying to the Democratic Republic of Congo to help control the outbreak. The three UK-PHRST team members deploying include two experts in tracking outbreaks, LSHTM’s Hilary Bower and Olivier le Polain from Public Health England, and data scientist Patrick Keating from LSHTM.
The team is expected to remain in the DRC for around six weeks, during which time they will help track the spread of the outbreak, and will also support in establishing robust data systems that will help align crucial information gathering. The UK-PHRST also has expertise in various other key areas for Ebola response, such as laboratory diagnostics, that can be deployed should they be needed.
Q&A with team Director, Prof Dan Bausch.
In April 2017, Professor Daniel Bausch was appointed Director of the UK-PHRST. Prof Bausch is a specialist in emerging infectious diseases trained in internal medicine, infectious diseases, tropical medicine, and public health. He has extensive experience in sub-Saharan Africa, Latin America, and Asia combatting deadly global health threats such as Ebola virus, hantavirus, and SARS coronavirus.
A year on from the team's first deployment, Prof Bausch tells us more about the team and how they work to assist in managing disease outbreaks.
The UK Public Health Rapid Support Team (UK-PHRST) is deploying to Sierra Leone to help reduce the risk of a disease outbreak following the deadly landslides in Freetown.
Following natural disasters, outbreaks of water-borne diseases such as cholera can occur, particularly where there is a lack of access to clean water and sanitation. Given the scale of the disaster in Freetown, the local capacity to detect and control a disease outbreak is limited and the Government of Sierra Leone has requested international support.
The UK-PHRST team deployed to Sierra Leone includes experts in tracking the progress of an outbreak and diagnosing its cause, as well as a logistician. It will be working alongside Sierra Leone health system professionals and other experts in disaster relief to support the Sierra Leone Government’s response. As the UK-PHRST’s deployment progresses, it will continue to provide support and share expertise with our partners in Sierra Leone to strengthen the health system beyond the immediate response.
Professor Daniel Bausch has been appointed Director of the new UK Public Health Rapid Support Team (UK-PHRST).
Prof Daniel Bausch, a specialist in emerging infectious diseases trained in internal medicine, infectious diseases, tropical medicine, and public health, will take up the position of Director of the UK-PHRST in April. He has extensive experience in sub-Saharan Africa, Latin America, and Asia combatting deadly global health threats such as Ebola virus, hantavirus, and SARS coronavirus.
His most recent role was as the Technical Lead for the Epidemic Clinical Management Unit in the World Health Organization's (WHO) Pandemic and Epidemic Diseases Department. He is a tenured Professor at the Tulane University Health Sciences Center in the United States and has served as a regular consultant for the WHO, the United Nations and the US National Institutes of Health. In addition to his expertise in the sciences, Prof Bausch places a strong emphasis on capacity building in all his projects and also has a keen interest in the role of the scientist in promoting health and human rights.
The UK Public Health Rapid Support Team (UK-PHRST) has deployed to Nigeria to help control an unusually large outbreak of Lassa fever, a viral haemorrhagic illness that can cause severe symptoms and sometimes death.
Lassa fever outbreaks occur in most years in Nigeria but on a lower scale. Given the size of the current outbreak and the risk of further spread locally, the Government of Nigeria has requested support from the UK-PHRST.
The London School of Hygiene & Tropical Medicine has been chosen to jointly run the newly established UK Public Health Rapid Support Team in partnership with Public Health England. Public Health Minister Nicola Blackwood announced the £20m initiative, to help prevent global health emergencies on behalf of the UK Government. It means the UK has a fully operational specialist team that is ready to be deployed anywhere in the world within 48 hours to tackle disease outbreaks which have the potential to develop into major health emergencies.
It will continually monitor infectious disease outbreaks around the world, identifying situations where the deployment of specialist expertise could help mitigate threats. When not responding to a disease outbreak, the team will research how best to deal with different types of outbreak scenario as well as training a group of public health reservists so the UK maintains the capability to rapidly scale up responses to outbreaks.
Responding effectively to outbreaks of infectious diseases saves lives. Sharing knowledge, learning, and experience of outbreak response across geographies, diseases, and between researchers and policy makers is essential. Without collaboration, outbreaks risk spreading in size and scale.
The UK Health Security Agency and the London School of Hygiene & Tropical Medicine came together in 2016 to form the UK Public Health Rapid Support Team (UK-PHRST), with an academic consortium including the University of Oxford. The UK-PHRST’s integrated tripartite remit includes outbreak response, research, and capacity building.
Funded by UK aid from the Department of Health and Social Care, UK-PHRST supports low- and middle-income countries (LMICs) in investigating and responding to disease outbreaks and conducts research to improve our response to future epidemics.
The UK-PHRST are pleased to announce the launch of their new Knowledge Hub, where practitioners and researchers can find and share the most useful information for their work in outbreak response.
Hosted on The Global Health Network, the Knowledge Hub aims to:
- Bridge the gap between the fast-paced world of online discussion forums and maintain long-term access to useful resources.
- Share up-to-date research and policy, as well as a dedicated education and training area with resources to support learning and inform effective outbreak response.
- Connect UK-based researchers with specialists in LMICs, creating a flow of information exchange and localised adaptations to outbreaks.
Many of these resources have been developed by UK-PHRST and its partners, including a number of virtual learning resources on COVID-19.
The new UK-PHRST Knowledge Hub provides a community function, allowing members to start group conversations around key topics, such as this timely post on contact tracing technology and comment on current issues, as shown in this blog on the importance of Looking after Mental Health in COVID-19.
We look forward to you joining, contributing and using our Knowledge Hub as a reliable and up-to-date source on outbreak response! Please do give us feedback on how you would like to see the UK-PHRST Knowledge Hub evolve in our discussion forum here.
About The Global Health Network
Faster and better research is critical to solving the world’s biggest health challenges. The Global Health Network enables researchers and institutions to share best practice and know-how with each other to drive progress, while empowering local health professionals undertaking research in the world’s most vulnerable settings. The Global Health Network facilitates sustainable health improvements through sharing of research methods, knowledge and experience through an open-access online platform and face-to-face within varied healthcare settings. It delivers training, skills and career development to frontline health workers, no matter where they are or how resource-constrained their environment may be. The result is easier, faster, better research to help address the world's biggest health challenges.
Visit: www.theglobalhealthnetwork.org.
The UK-PHRST are deployed to outbreaks all over the world from Bangladesh to Nigeria to Sudan. Working alongside in-country staff from Minstries of Health, NGOs and other government organisations, UK-PHRST successfully help combat the outbreak and protect against future threats to health. Read some of our stories below:
- Using PPE in outbreak response
The UK Public Health Rapid Support Team (UK-PHRST), funded by UK aid from the Department of Health and Social Care, supports low- and middle-income countries in investigating and responding to disease outbreaks and conducts research to improve our response to future epidemics.
Our expertise in infection and prevention and control, which includes the use of Personal Protective Equipment (PPE), is used to protect people from infection in disease outbreaks. PPE can diminish transmission when used as part of an integrated package of measures, and crucially helps protect medical staff from disease, but there is variation in the need for, and use of PPE for different diseases, across countries, and differing views on its necessity.
This project investigated the use of PPE to protect people from Lassa Fever, in specific Lassa Fever Treatment Centres (LTCs) across Nigeria.
Lassa fever is often confused with Ebola or other viral haemorrhagic fevers, but it differs - it is less fatal, and its transmission is very different. Ebola is transmitted between people, whereas Lassa fever is spread to most people (~80%) through exposure to food or household items contaminated by rats. Less commonly, transmission can occur in laboratories, or between people, particularly in health care settings with inadequate infection prevention and control measures.
Why are the UK-PHRST involved?
Lassa Fever is an important cause of outbreaks of infectious disease. It is one of the pathogens in the World Health Organizations’ list of epidemic threats needing urgent research. The disease is endemic in rodent populations in parts of West Africa including Benin, Ghana, Guinea, Liberia, Mali, Sierra Leone, Togo, and Nigeria, and most likely exists in other West African countries as well. Cases are increasing in Nigeria.The nuances between viruses causing haemorrhagic fevers, such as Ebola and Lassa Fever, are not translated into official guidance, and policies end up addressing them in the same manner. In addition, much of the research and guidance for PPE are developed in high-income settings, where there are few cases of disease, therefore the guidance is built on data, rather than lived experience.
Recognising limitations in existing guidance, The Nigerian Centre for Disease Control (NCDC) invited the UK-PHRST work with them to investigate whether their infection, prevention and control (IPC) policies devised in 2017 were effectively disseminated and how, in the case of Lassa Fever, they were operationalised.
A woman suspected of contracting Lassa Fever awaits her lab results in quarantine. Suspect cases of Lassa Fever typically wait 12-24 hours for their samples to be tested locally at the virology laboratory. If positive they are moved by ambulance to the confirmed case ward a short distance away. What did they discover?
The team found that health care workers in Lassa treatment centres (LTCs) were frequently not using PPE in line with government guidelines. Limited availability of PPE in some centres led to health care workers using personal risk assessments to drive decision-making about its use, and there is a gap in understanding of staff perceptions, and how they protect themselves, in the absence of adequate PPE.
During interviews, researchers noticed that much importance was placed on the language, behaviour and understanding of PPE by the health workers. For example, some staff were basing their decision-making on what they perceived as ‘careful’ best practice, but this is not reflected in guidance. Staff also consistently expressed challenges with using PPE, for example in the environment they were using it in (high temperatures), with poor quality materials (gloves breaking or tearing), and limited function (reduced visibility when using eye protection).
Inside the grounds of the Federal Training Hospital (FETHA) in Abakaliki, a makeshift Lassa Fever holding centre is prepared for quarantining of suspected cases. To mitigate some of these issues, some health workers adapted PPE to suit their local context; for example, choosing to wear a surgical gown in replacement of gowns provided, saying they were cooler to wear and simpler to remove.
The study team observed that judgements made by health workers were based on their experience and understanding of the situation, and this was very different to PPE guidance from international and national bodies.
Demonstrating a correctly prepared personal protective equipment suit In low- and middle-income countries (LMICs), funds assigned for PPE procurement and supplies can be limited. Where there are competing demands, funds are often redirected to more immediate requirements, such as emergency operations, or treatments.
Alongside this, there were worries that the PPE provided was substandard. Much of the PPE in use had been donated, for example from non-governmental organisations, and there was no formal process in place to ensure it was fit for purpose.
Capacity building: Preventing future fires
As a result of the collaborative work carried out in the LTCs, The Nigeria Centre for Disease Control (NCDC) has revised national guidance on infection prevention control for viral haemorrhagic fevers.
Together with this success, emphasis on the quality of PPE facilitated prompted dialogue at a national level about developing assurance systems so that donation of equipment is fit for purpose in the future. These results have informed national advocacy work for improvements to supplies to Lassa Treatment Centres – with the ultimate aim of reducing countrywide infection.
Dr Abdulmajid Suleiman Musa shows a group of NCDC staff how a correctly prepared PPE suit should look when working in a virus hit region, Keffi, Nasarawa state. Nurse Mary Obasi measures the temperature of woman with Lassa Fever in the confirmed ward at the FETHA 02 facility, Abakaliki, Ebonyi state How can this work be translated into other contexts?
There has also been ongoing professional collaboration between the NCDC as part of the COVID-19 response with Africa Centre for Disease Control and as part of the African Union Taskforce for COVID-19.
Thinking through novel and more nuanced approaches to PPE is useful when considering PPE for COVID-19. It is also helpful in the face of supply chain issues, with many countries unable to source PPE during the pandemic. Rational use of PPE has been suggested to mitigate insufficient PPE supplies.
While COVID-19 has brought worldwide disruptions to PPE supplies, and its availability, the experience of clinicians in LMICs has much to teach us all about the realities of working with limited resources; developing adaptations and creating innovative local solutions. However, it is important that guidelines are rooted in evidence-based best practise, as well as reflecting the reality of those who are required to implement them.
Read the updated guidelines and vital role the NCDC plays in keeping hospitals, clinics, and health facilities safe and free from disease.
- Mystery pathogens and the role of the modular flight case mobile laboratory
Funded by UK aid from the Department of Health and Social Care, the multidisciplinary nature of the UK Public Health Rapid Support Team (UK-PHRST) allows its outbreak response support to take many forms, depending on the situation, and includes a mobile laboratory that can be deployed worldwide. This enables instant diagnostic capacity to process samples, identify causal agents, and tackle disease outbreaks.
The Philippines, like many tropical countries, has a wide variety of infectious agents circulating that cause febrile illness and severe disease. Patients presenting with febrile symptoms could be infected with dengue, yellow fever, zika, or malaria, for example. When there is a spike in fever cases in any country, it is vital that the diagnostic tests can accurately describe the pathogen or ‘causal agent’ – to facilitate appropriate treatment and prevent further spread.
Why are the UK-PHRST involved?
Dengue is a mosquito-borne viral disease that has rapidly spread in all regions of WHO in recent years. The Americas, South-East Asia and Western Pacific regions are the most seriously affected, with Asia representing ~70% of the global burden of disease. As part of its public health system to identify cases, and outbreaks, it is compulsory to record dengue cases in The Philippines. This enables trends to be analysed which provides potential notice for future outbreaks.
Dengue is a disease that not only has a high impact on health of the population, but also a large impact economically, therefore it is essential to identify outbreaks with the end goal of using targeted control measures to help combat the spread and repercussions.
So how are they tracking cases?
A national surveillance programme tracks cases countrywide, with 21 disease reporting units across 17 regions – 4 in the national capital region. The units are housed in hospitals and clinics. Many of the reported cases are ‘suspected dengue’ where the patient has presented clinical symptoms, but this has not necessarily been followed up with a laboratory test due to limited diagnostics.
From the national surveillance programme, the UK-PHRST identified >4,000 patients, including more than 1,000 with severe disease, that had been tested and actually found to be dengue negative. From these, UK-PHRST prioritised samples from severe cases and identified ~400 to analyse (2015-2016). Then they sought to identify the unknown cause(s), the so called ‘mystery pathogen(s)’ of this febrile illness.
The role of the modular flight case mobile laboratory
To test and diagnose disease, UK-PHRST deployed research expertise and various components of the modular flight case laboratory via airline courier to The Philippines. Inside this mobile laboratory are two very sophisticated pieces of kit, previously not used in-country, a MinION and a Film Array. Both accurately diagnose disease by analysing the genetic code and comparing it with an existing database of genetic material. This process is called metagenomics.
Metagenomics identifies the closest strains or sequences of disease, which can also give the transmission patterns and geographical origin.
How does this differ from current diagnostics?
Through use of metagenomics, all genes from the sample are sequenced, rather than specifically testing for an individual pathogen. Film Array is useful because it has the capacity to detect a range of pathogens, then the MinION enables precise confirmation of the causal agent. Because all the DNA is sequenced using these techniques, it gives scientists the ability to spot any disease, as well as find new strains of diseases.
Interestingly, within the samples there was lots of dengue present, despite testing negative. This suggests a new strain is not being picked up by the existing diagnostic tests.
Prior to the arrival of the mobile laboratory in The Philippines, diagnostics were only available for diseases the test is designed to recognise – allowing new strains to go under the radar.
How were the samples previously tested?
Samples can be tested in the Philippines, but the majority of sequencing would be carried out in labs overseas. For various reasons, this makes the process longer and creates a gap between sample collection and identification of the unknown pathogen, and all the time the outbreak can increase.
Firstly, there is difficulty shipping samples overseas because you need national and institutional approvals. Testing for Dengue is a lab bench process in The Philippines since it is as common as ‘flu. Elsewhere, such as the UK, dengue is very rare, therefore, to work on the virus itself research is contained within a category 3 laboratory and requires certain standards of biohazard safety. DNA needs to be transferred into RNA to be categorised as ‘uninfectious’ before shipping, and again, this increases the length of the process.
Having the in-country capacity to process samples makes a huge difference to the diagnosis and prevention of outbreaks.
Will this work continue?
The UK-PHRST tested three batches using these techniques, with 31/107 samples processed. As a result of the deployment, the team at Research Institute for Tropical Medicine in Manila are trained and equipped to test the next few batches.
To train a laboratory scientist on a Film Array, it requires one or two sessions of a couple hours each. A MinION takes slightly longer and training can be up to a week, as you are required to initially prepare and clean the sample. The time-consuming component is the analysis, with plenty of training and biological theory involved. As this is work with datasets, this part of the process can be supported remotely.
UK-PHRST can train and equip a team with the necessary techniques to diagnose unknown disease outbreaks within three weeks of the mobile laboratory arriving in the country.
The in-country team are then better prepared to manage further outbreaks without direct support.
Can this be used in other outbreak settings?
Any additions to the global database of genetic material from pathogens can assist with the diagnosis of future disease outbreaks worldwide. Scientists use these data to compare the genetic code to this database and further develop diagnostics for fever cases in many different settings.
In Sudan, the UK-PHRST used minimal components of the modular flight case laboratory to determine the requirements for metagenomic sequencing and analysis. 32 samples were sequenced in-country and Chikungunya virus was identified
In all 139 samples sequenced, Chikungunya virus was identified in 84%, with the metagenomic approach also identifying co-infections in six patients including ‘Dengue 4’ - not previously known to be circulating in Sudan.
"This case study shows the UK-PHRST are able to deploy a mobile laboratory providing cutting-edge diagnostic capabilities matching even the best ‘static’ laboratories. However, the value of this lab reaches beyond just doing the science and diagnostics; it provides a mobile training facility allowing local scientists, in countries such as the Philippines and Sudan, to learn and experience new techniques and develop their own scientific skills."
Dr Ben Gannon
The use of this method in Khartoum, Sudan, demonstrated capability to identify previously unknown pathogens. This shows that during an outbreak, the UK-PHRST can effectively deploy laboratory equipment to provide high level diagnostic capability, which is often unavailable even in most high-income health facilities.
The work of the mobile laboratory makes outbreak response more efficient, better equipped, and ready to tackle mystery pathogens all over the world.
Join the UK-PHRST Knowledge Hub here to find out more.
- What does it take to deploy in 48 hours?
No two outbreaks are the same. Having completed 19 deployments between April 2017 and November 2020, the operations team can safely testify that there is a need to remain alert, agile, and consistently open to change. Regardless of the mode of deployment, destination or disease, there are always new challenges to navigate.
For example, the suspension of air travel, resulting from border controls during the COVID-19 pandemic, led the team to explore new and innovative ways to offer technical support. Technical expertise was delivered remotely alongside a wide range of partners (including WHO Bangladesh and Africa CDC). This offered opportunities for reservist staff who may not be released for a six-week deployment to volunteer their support.
A full summary of deployments up to November 2020 below:
We will summarise the operational requirements to deploy UK-PHRST staff and reflect on what it takes to be operationally ready.
Onboarding staff:
Feedback from a wide range of governmental and non-governmental organisations supported the creation of processes to support the onboarding and advanced preparation of deployable staff.
- Medical
It is critical that individuals are medically fit for deployment and have all the necessary routine vaccinations to support their health and wellbeing whilst overseas. A routine schedule of vaccinations alongside a comprehensive medical assessment is required on appointment to the team. Individuals are then issued with an emergency medications kit, first aid kit and trauma kit (and of course, the training on what to do them). - Training
In addition to the necessary technical training, UK-PHRST individuals undertake mandatory UK-PHRST training which aims to prepare them for operating effectively overseas. This includes residential safety and security training, safeguarding training and an immersive 5-day deployment course alongside a package of online learning. - Logistics
Deployed staff are given a comprehensive kit to support their deployment, which includes resources for a wide range of environments (e.g. IT equipment, tents, mosquito nets, water chlorination tablets and ration packs). This kit is systematically reviewed, managed, and maintained by the operations team. external audits of the kit have taken place to ensure rigor and continual improvements are made. - Deployment handbook
This is a guidance document containing all the processes and procedures required of UK-PHRST staff. It incorporates all feedback to date and serves to anticipate any questions relating to finance, medical support, incidents, travel, logistics and more.
Accepting a request to deploy:
When the UK-PHRST Director receives a request to deploy, the following steps are taken;
- Criteria – Considerations to deploy include the country, infectious disease agent, location, partners already engaged and threat to further spread (particularly cross border).
- Approval – A Cross-Government protocol (developed in advance with key partners) ensures rapid consideration of any request received by HMG departments. This protocol has been revised several times and represents the key approval mechanism for the team to deploy.
To prepare for deployment:
Once a deployment has been accepted, the team are sent additional information;
- Risk assessment – a travel risk assessment is prepared in advance and includes any known hazards and mitigating actions in relation to the specific deployment, pathogen and country.
- Information pack– includes country and disease specific documentation to aid preparations.
- Pre-deployment briefing – A meeting is set up with the Director, deploying team and key UK-PHRST members to discuss a range of aspects relating to the deployment. This is an opportunity for the individuals to ask any questions and includes, but is not limited to, input from subject matter experts, medical advice, logistics and admin support.
In the field:
Whilst in the field team members have access to a wide range of 24/7 support from the UK based team. They also benefit from access to a dedicated nurse within the PHE Occupational Health team.
Reporting of any health and safety incidents or other concerns is done through a systematic process which links in with PHE reporting policies.
- Medical
- Making mental health and psychosocial support part of outbreak response
Although mental health affects everyone, whether it’s people trying to maintain their mental wellbeing or those living with a mental health condition, it is often forgotten about in the response to a public health emergency. This is particularly a problem in countries where services are already limited. Before the COVID-19 pandemic, resources allocated to mental health were scarce, with a median of 2% of government expenditure allocated to mental health across the world. During the pandemic, more resources were shifted towards managing COVID-19 infections, making the existing care gap even wider - in a global survey by the World Health Organization (WHO), 93% of 130 countries surveyed reported substantial disruption to their mental health services during the pandemic.
The UK-PHRST has a dedicated Mental Health and Psychosocial Support (MHPSS) team that works particularly across the African and the Eastern Mediterranean regions, on projects ranging from research and capacity strengthening activities to deployments.
The team works to integrate mental health into outbreak response plans and procedures, to improve the mental health and psycho-social wellbeing of people affected, including staff from organisations assisting on the ground – a direct response to the serious impact that these events can have on individuals and communities. During the COVID-19 pandemic in 2020 for instance, global prevalence of depression and anxiety disorders increased by a quarter, with the WHO stating the pandemic “had a severe impact on the mental health and wellbeing of people around the world”.
Strengthening existing MHPSS guidance in outbreaks through research
The team has a diverse research portfolio split into four main phases:
- Phase 1: Identify the needs, resources and current interventions for MHPSS across the African continent
- Phase 2: Work with stakeholders to explore how to better support existing MHPSS frameworks to adapt them into location and outbreak specific response tools
- Phase 3: Test the proposed MHPSS interventions in an outbreak scenario
- Phase 4: Produce a package of MHPSS interventions as a best practice guide which can be applied to specific outbreak situations
The team has already started to see real progress thanks to its research. For instance, members of the UK-PHRST team worked with a consortium of public health institutions in Africa including the Africa Centre for Disease Control (Africa CDC), World Health Organization African Region (WHO AFRO), WHO Regional Office for the Eastern Mediterranean (WHO EMRO) on the Strengthening Public Mental Health in Africa in Response to Covid-19 (SPACE) programme. The programme aimed to help integrate MHPSS into African countries’ emergency responses by exploring the extent to which MHPSS was already included in the national response to the COVID-19 pandemic in African countries. The consortium also examined the barriers and enablers to MHPSS integration in the COVID-19 response. Based on their findings, they recommend five key areas to target for improving mental health integration into the response to public health emergencies. The SPACE programme also acted as a catalyst to the development of working partnerships with regional health bodies and the establishment of an informal network of MHPSS experts across Africa. The research project, alongside other evidence sources, helped inform Africa CDC’s decision to integrate MHPSS into its strategic plan for emergencies.
Building recognition for MHPSS in outbreak response through capacity strengthening
In many countries, current outbreak response infrastructure and national outbreak response plans do not incorporate MHPSS measures. Through its capacity strengthening work, the UK-PHRST MHPSS team actively advocates for MHPSS to be included as part of national outbreak response plans with key health leaders, the strengthening of local co-ordination capabilities and dedication of resources to the area. For example, the team collaborate with Africa CDC to organise workshops throughout African regions to build recognition for the importance of MHPSS in outbreaks, while also taking the opportunity to learn from national MHPSS and emergency response leads to better understand how MHPSS can fit into a local context. In February 2022, the Liberian Ministry of Health, Africa CDC and the UK-PHRST MHPSS team hosted a three day regional workshop bringing together mental health experts from institutions in Africa and worldwide with national mental health leads from Liberia, Sierra Leone, Cameroon and Nigeria. The workshop aimed to build a knowledge and expertise sharing regional network whilst also developing a Theory of Change model for integrating mental health into national emergency preparedness and response plans.
Group attendees of UK-PHRST, Liberian Ministry of Health and Africa CDC Regional MHPSS Workshop. Image credit: Mental Health Innovation Network/Liberian Ministry of Health Finally, the team have also worked directly with organisations like Africa CDC’s African Volunteers Health Corps (AvoHC) to add MHPSS to the list of expertise they provide in public health emergencies in the continent and contributed to WHO Eastern Mediterranean Region’s MHPSS action plan.
Making MHPSS expertise part of outbreak deployments
A lack of global prioritisation for MHPSS during outbreaks, coupled with limited funding and understanding of its benefits, means that MHPSS experts are often not requested during an outbreak response call.
To address this, the UK-PHRST team is actively working to strengthen deployment mechanisms for rapid response, through collaboration AvoHC and IASC/Dutch Surge Support mechanisms. As a part of this collaboration, a group of MHPSS professionals will be trained and prepared to be deployed to ensure that MHPSS is an integral part of the outbreak response.
MHPSS deployments would allow a country to bring in experts to increase its preparedness and response capacity for mental health during an outbreak, allowing other in-country response teams to prioritise the other public health measures that are also required.
Work with the UK-PHRST MHPSS team
If you would like to find out more about the MHPSS team within the UK-PHRST, including how to collaborate or request their help during an outbreak please contact uk-phrst@lshtm.ac.uk.