Covid-19 reports, webinars and updates
We are a member of C19economics.org that collates health economic research on COVID-19 globally. Below is a sample of our work on COVID-19, for more, please visit the Centre for Mathematical Modelling of Infectious Diseases and the Centre for Economic Policy Research.
- Safeguarding evidence-based decision making in the FDA for COVID-19 vaccines
-
Authors: Dr Aris Angelis, Dr Jonathan Darrow
Public polls in the summer and fall of 2020 indicated two-thirds of Americans would be reluctant to get a COVID-19 vaccine once available,[1] worrying that political pressure could cause the US Food and Drug Administration (FDA) to rush its review. Such a lack of public confidence suggests a weakening of the FDA’s organizational reputation and credibility,[2] which could adversely affect COVID-19 vaccine uptake and thereby undermine public health efforts to achieve herd immunity. In light of the ongoing importance of vaccination to COVID-19 and a growing array of diseases, we consider the causes of such public skepticism and propose means to overcome it.
For full text review click here.
- Joining up health and economic policy to address COVID-19
-
Prof Peter Piot (LSHTM), Prof Edwine Barasa (KEMRI-Wellcome Trust), Prof John Edmunds (LSHTM), Dr Gesine Meyer Rath (Boston University), Mr Paul Johnson (Institute for Fiscal Studies), and Prof Anna Vassall (LSHTM) discuss joining up health and economic policy to address Covid-19 during the HESG Winter 2021 Meeting.
The meeting was hosted online by the Global Health Economics Centre, LSHTM, from 6th-8th January 2021
Click this link to watch the video recording.
- The Need for Novel Approaches in Assessing the Value of COVID-19 Vaccines
-
Authors: Dr Aris Angelis, Prof Rob Baltussen, and Dr Tommi Tervonen
Numerous coronavirus disease 2019 (COVID-19) vaccine development programs are under way, and several vaccines with potentially differing clinical and manufacturing profiles are expected to reach the market. We argue for the need to adopt new approaches for assessing the value of COVID-19 vaccines, calling for clinical, manufacturing and cost aspects to be complemented by societal value considerations to inform the vaccines' further development, reimbursement and pricing decisions.
For full text review click here.
-
Launch: a platform to support the researchers and decision-makers generating and using health economics research to tackle COVID-19
-
Since the beginning of the outbreak, the scientific community has worked around the clock to produce evidence to support decision-makers in all aspects of COVID management. As of November 2020, we have over 52,000 articles published in peer reviewed journals and pre-prints (as indexed by collabovid.org). Those unprecedented global collective research efforts already boasts many successes: earlier this week, Pfizer announced that a vaccine showed a 90% effectiveness. The RECOVERY trial in the UK found that Dexamethasone, if administered to patients on ventilation or oxygen support, could lead to a significant reduction in 28-day mortality rates. Despite costly early failures, different manufacturers are now also producing rapid test kits to be widely rolled out, especially in low-resource settings.
The response to COVID-19 requires governments to develop and evaluate a vast number of policies and guidance to tackle the outbreak and protect the health of its populations. Health economics can support decision-makers in appraising different investments and policy options, consider trade-offs, as well as adopt a ‘whole of health’ approach to the response. However, health economics research has been largely missing from this growing literature. This is problematic, especially in low and middle income countries, where budget constraint are significant (current health expenditure – from all sources- was less than $30 per person per year in 10 countries according to the WHO GHED database).
Health economics can support with (i) managing the health sector response (e.g. planning for medical supplies and resources to treat covid patients), (ii) considering trade-offs between COVID and other health priorities in the health sector, (iii) considering trade-offs with the wider economy (through the application of cost-benefit analysis, which can be relevant when considering lockdowns and other non-pharmaceutical interventions), and estimating the health impacts of the COVID response using a whole of health approach.
The C19economics.org platform
It has become obvious that many of us will live with COVID for the months ahead. For our work, this means continuation in restrictions of travel, limited face-to-face interactions, and on-going research or policy work to support planning of the COVID response, under substantial time and political pressure. The C19economics.org platform has been launched to support policy-makers (and their advisers) and researchers working on health economics for COVID, with a focus on LMICs.
C19Economics.org was created to curate experiences, data, tools and analyses, facilitate the meeting of researchers and decision-makers and support health economists generate evidence for policy across LMIC settings in a demand driven and scientifically robust fashion. The goal is to facilitate the sharing of experiences and provide analysts with access to a focussed set of resources, a space to informally receive peer support and review each other’s work. In addition, the platform aims to provide decision makers and those who advise them with a space to link up with analysts, ask questions about research directly linking to their policy needs, and access summaries of relevant evidence.
To this aim, C19economics.org contains a repository of evidence, an insights page (including summaries, blogposts and other contributions from our members), a discussion forum (open to all, sign up required) and will be running regular webinars and events on request from C19economics platform users on research or decision-making. For instance, two webinars have already been lined up on “Webinar: Macroeconomic and health impact of COVID: the meeting of two communities” and “Estimating Clinical Management Costs of Covid-19 in LMICs”.
The beginnings of a community on health economics
Please go to C19economics.org to visit our platform and be connected to other researchers and decision-makers.
C19economics.org has been put together by a group of health economics practitioners, coordinated by iDSI (International Decision Support Initiative) and London School of Hygiene and Tropical Medicine (LSHTM). C19economics.org is funded by the Bill and Melinda Gates Foundation, UK Aid and the Wellcome Trust. Partners of the website include UK Foreign Commonwealth and Development Office and the Health Intervention and Technology Assessment Program.
- Integrating economic and health evidence to inform Covid-19 policy in low- and middle- income countries
-
Authors: Anna Vassall, Sedona Sweeney, Edwine Barasa, Shankar Prinja, Marcus R Keogh-Brown, Henning Tarp Jensen, Richard Smith, Rob Baltussen, Rosalind M Eggo, Mark Jit
Covid-19 requires policy makers to consider evidence on both population health and economic welfare. Over the last two decades, the field of health economics has developed a range of analytical approaches and contributed to the institutionalisation of processes to employ economic evidence in health policy. We present a narrative review outlining how these approaches and processes need to be applied more widely to inform Covid-19 policy; highlighting where they may need to be adapted conceptually and methodologically, and providing examples of work to date. We focus on the evidential and policy needs of low- and middle- income countries; where there is an urgent need for evidence to navigate the policy trade-offs between health and economic well-being posed by the Covid-19 pandemic.
For full text review click here.
- The impact of Covid-19, associated behaviours and policies on the UK economy: A computable general equilibrium model
-
Authors: Marcus R.Keogh-Brown, Henning Tarp Jensen, W. John Edmunds, Richard D.Smith
We estimate the potential impact of COVID-19 on the United Kingdom economy, including direct disease effects, preventive public actions and associated policies. A sectoral, whole-economy macroeconomic model was linked to a population-wide epidemiological demographic model to assess the potential macroeconomic impact of COVID-19, together with policies to mitigate or suppress the pandemic by means of home quarantine, school closures, social distancing and accompanying business closures.
Our simulations indicate that, assuming a clinical attack rate of 48% and a case fatality ratio of 1.5%, COVID-19 alone would impose a direct health-related economic burden of £39.6bn (1.73% of GDP) on the UK economy. Mitigation strategies imposed for 12 weeks reduce case fatalities by 29%, but the total cost to the economy is £308bn (13.5% of GDP); £66bn (2.9% of GDP) of which is attributable to labour lost from working parents during school closures, and £201bn (8.8% of GDP) of which is attributable to business closures. Suppressing the pandemic over a longer period of time may reduce deaths by 95%, but the total cost to the UK economy also increases to £668bn (29.2% of GDP), where £166bn (7.3% of GDP) is attributable to school closures and 502bn (21.9% of GDP) to business closures.
Our analyses suggest Covid-19 has the potential to impose unprecedented economic costs on the UK economy, and whilst public actions are necessary to minimise mortality, the duration of school and business closures are key to determining the economic cost. The initial economic support package promised by the UK government may be proportionate to the costs of mitigating Covid-19, but without alternative measures to reduce the scale and duration of school and business closures, the economic support may be insufficient to compensate for longer term suppression of the pandemic which could generate an even greater health impact through major recession.
For full text review click here.
- The health sector cost of different policy responses to COVID-19 in low- and middle- income countries
-
Authors: Sergio Torres Rueda, Sedona Sweeney, Fiammetta Bozzani, Anna Vassall
Much attention has focussed in recent months on the impact that COVID-19 has on health sector capacity, including critical care bed capacity and resources such as personal protective equipment. However, much less attention has focussed on the overall cost to health sectors, including the full human resource costs and the health system costs to address the pandemic. Here we present estimates of the total costs of COVID-19 response in low- and middle-income countries for different scenarios of COVID-19 mitigation over a one year period. We find costs vary substantially by setting, but in some settings even mitigation scenarios place a substantial fiscal impact on the health system. We conclude that the choices facing many low- and middle- income countries, without further rapid emergency financial support, are stark, between fully funding an effective COVID-19 reponse or other core essential health services.
For full text review click here.
- The impact of Coronavirus disease 2019 (COVID-19) on health systems and household resources in Africa and South Asia
-
Authors: Nicholas G Davies, Sedona Sweeney, Sergio Torres-Rueda, Fiammetta Bozzani, Nichola Kitson, Edwine Barasa, Simon Procter, Matthew Quaife, LSHTM Centre for Mathematical Modelling of Infectious Diseases COVID-19 Working Group, Rosalind M Eggo, Anna Vassall, Mark Jit
Background. Coronavirus disease 2019 (COVID-19) epidemics strain health systems and households. Health systems in Africa and South Asia may be particularly at risk due to potential high prevalence of risk factors for severe disease, large household sizes and limited healthcare capacity. Methods. We investigated the impact of an unmitigated COVID-19 epidemic on health system resources and costs, and household costs, in Karachi, Delhi, Nairobi, Addis Ababa and Johannesburg. We adapted a dynamic model of SARS-CoV-2 transmission and disease to capture country-specific demography and contact patterns. The epidemiological model was then integrated into an economic framework that captured city-specific health systems and household resource use. Findings. The cities severely lack intensive care beds, healthcare workers and financial resources to meet demand during an unmitigated COVID-19 epidemic. A highly mitigated COVID-19 epidemic, under optimistic assumptions, may avoid overwhelming hospital bed capacity in some cities, but not critical care capacity. Interpretation. Viable mitigation strategies encompassing a mix of responses need to be established to expand healthcare capacity, reduce peak demand for healthcare resources, minimise progression to critical care and shield those at greatest risk of severe disease.
For full text review click here.
- The potential health and economic value of SARS-CoV-2 vaccination alongside physical distancing in the UK: transmission model-based future scenario analysis and economic evaluation
-
Authors: Frank Sandmann, Nicholas Davies, Centre for the Mathematical Modelling of Infectious Diseases COVID-19 working group, Anna Vassall, W John Edmunds, Mark Jit
Background: In response to the coronavirus disease 2019 (COVID-19), the UK adopted mandatory physical distancing measures in March 2020. Vaccines against the newly emerged severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) may become available as early as late 2020. We explored the health and economic value of introducing SARS-CoV-2 immunisation alongside physical distancing scenarios in the UK. Methods We used an age-structured dynamic-transmission and economic model to explore different scenarios of immunisation programmes over ten years. Assuming vaccines are effective in 5-64 year olds, we compared vaccinating 90% of individuals in this age group to no vaccination. We assumed either vaccine effectiveness of 25% and 1-year protection and 90% re-vaccinated annually, or 75% vaccine effectiveness and 10-year protection and 10% re-vaccinated annually. Natural immunity was assumed to last 45 weeks in the base case. We also explored the additional impact of physical distancing. We considered benefits from disease prevented in terms of quality-adjusted life-years (QALYs), and costs to the healthcare payer versus the national economy. We discounted at 3.5% annually and monetised health impact at 20,000 per QALY to obtain the net monetary value, which we explored in sensitivity analyses. Findings Without vaccination and physical distancing, we estimated 147.9 million COVID-19 cases (95% uncertainty interval: 48.5 million, 198.7 million) and 2.8 million (770,000, 4.2 million) deaths in the UK over ten years. Vaccination with 75% vaccine effectiveness and 10-year protection may stop community transmission entirely for several years, whereas SARS-CoV-2 becomes endemic without highly effective vaccines. Introducing vaccination compared to no vaccination leads to economic gains (positive net monetary value) of 0.37 billion to +1.33 billion across all physical distancing and vaccine effectiveness scenarios from the healthcare perspective, but net monetary values of physical distancing scenarios may be negative from societal perspective if the daily national economy losses are persistent and large. Interpretation Our model findings highlight the substantial health and economic value of introducing SARS-CoV-2 vaccination. Given uncertainty around both characteristics of the eventually licensed vaccines and long-term COVID-19 epidemiology, our study provides early insights about possible future scenarios in a post-vaccination era from an economic and epidemiological perspective.
For full text review click here.
- Routine immunisation is essential, even during the COVID-19 pandemic
-
Authors: Kaja Abbas, Simon R Procter, Kevin van Zandvoort, Andrew Clark, Sebastian Funk, Tewodaj Mengistu, Dan Hogan, Emily Dansereau, Mark Jit, Stefan Flasche, LSHTM CMMID COVID-19 Working Group.
The COVID-19 pandemic has brought human activity to a standstill and now threatens to undermine routine immunisation programmes. On March 26, 2020, the World Health Organization recommended that while routine immunisation programmes should continue, mass vaccination campaigns should be temporarily suspended because they could increase the spread of the virus in communities. A benefit-risk analysis was conducted to weigh up the health benefits of continued routine infant immunisation delivery against the excess risk of COVID-19 infections in Africa.
The results are striking – if routine immunisation was continued, for each excess COVID-19 death (predominantly among elderly household members) due to an infection acquired during the vaccination visit and spread to household members of vaccinated children, around 14 to 267 future child deaths could be prevented. Without vaccination, these deaths could result from a range of diseases including measles, yellow fever, pertussis, meningitis, pneumonia, and diarrhoea.
If countries do decide to continue with routine immunisation during the COVID-19 pandemic, they will need to work out ways to reduce human contact. For example, between other families waiting or health care workers, or on public transport when travelling to the site. Vaccinators will be at high risk of infection because of the sheer numbers of people they will be coming into contact with and will need to maintain stringent standards of infection prevention such as wearing suitable personal protective equipment and frequent hand washing.
In addition, whether or not a country suspends immunisation services, it will be critical for it to provide catch-up immunisations for any children who missed their vaccines due to the disruption caused by the COVID-19 pandemic.
Please find the links below for the publication and related dissemination.
- Routine childhood immunisation during the COVID-19 pandemic in Africa: a benefit–risk analysis of health benefits versus excess risk of SARS-CoV-2 infection
- Benefits of routine childhood vaccines far outweigh risks of additional COVID-19 transmission in Africa, modelling study suggests
- Should countries stop vaccinations to halt the spread of COVID-19?
- Routine vaccinations during a pandemic – benefit or risk?
- Models of COVID-19 vaccine prioritisation: a systematic literature search and narrative review
-
How best to prioritise COVID-19 vaccination within and between countries has been a public health and an ethical challenge for decision-makers globally. We reviewed epidemiological and economic modelling evidence on population priority groups to minimise COVID-19 mortality, transmission, and morbidity outcomes.
We searched the National Institute of Health iSearch COVID-19 Portfolio (a database of peer-reviewed and pre-print articles), Econlit, the Centre for Economic Policy Research, and the National Bureau of Economic Research for mathematical modelling studies evaluating the impact of prioritising COVID-19 vaccination to population target groups. The first search was conducted on March 3, 2021, and an updated search on the LMIC literature was conducted from March 3, 2021, to September 24, 2021. We narratively synthesised the main study conclusions on prioritisation and the conditions under which the conclusions changed.
For full text review click here.
- Exploring equity in health and poverty impacts of control measures for SARS-CoV-2 in six countries
-
Policy makers need to be rapidly informed about the potential equity consequences of different COVID-19 strategies, alongside their broader health and economic impacts. While there are complex models to inform both potential health and macro-economic impact, there are few tools available to rapidly assess potential equity impacts of interventions.
We created an economic model to simulate the impact of lockdown measures in Pakistan, Georgia, Chile, UK, the Philippines and South Africa. We consider impact of lockdown in terms of ability to socially distance, and income loss during lockdown, and tested the impact of assumptions on social protection coverage in a scenario analysis.
For full text review click here.
- COVID-19 vaccination in Sindh Province, Pakistan: A modelling study of health impact and cost-effectiveness
-
Multiple Coronavirus Disease 2019 (COVID-19) vaccines appear to be safe and efficacious, but only high-income countries have the resources to procure sufficient vaccine doses for most of their eligible populations. The World Health Organization has published guidelines for vaccine prioritisation, but most vaccine impact projections have focused on high-income countries, and few incorporate economic considerations. To address this evidence gap, we projected the health and economic impact of different vaccination scenarios in Sindh Province, Pakistan (population: 48 million).
For full text review click here.
- Moving beyond ‘lives-saved’ from COVID-19
-
Andrew Briggs
Professor of Health Economics
May 15, 2020Epidemiological models of the COVID-19 pandemic have largely focused their efforts on exploring the effectiveness of different policies to prevent deaths and to avoid overloading the ability of health care systems to handle the onslaught of cases. As we move from an extended period of lockdown to easing restrictions, it is a good time to think about moving beyond the simple metric of ‘lives-saved’. In other less challenging times, years of life lost (YLL) and Disability-Adjusted Life Years lost (DALYs) or Quality-Adjusted Years of Life lost (QALYs) are the more usual policy tool.
Yet even conditional life-expectancy is poorly understood. Examples abound where supposed life expectancy is ‘estimated’ by subtracting current age from life expectancy at birth (not to pick on anyone in particular – but see this tweet about an article by Vince Cable which raises useful issues but falls into this exact trap). This is surprising, as conditional life expectancy (by age and sex) are routinely compiled by almost all countries in the world using standard life table methods.
In this short blog we outline a policy tool that can be easily employed to generate YLL and (discounted) QALYs lost due to deaths from COVID-19 in a way that facilitates adjustment for comorbidities, while putting pay to the conventional wisdom that suggests that victims who are old and with long term conditions ‘would have died anyway’ (see for this article for example).
The approach itself involves a three-step process to adapt a standard life table:
- Add a Standardised Mortality Ratio (SMR) parameter to allow for increased mortality due to existing long-term conditions (LE).
- Adjust survival for background quality of life and the additional quality of life decrement associated with the long-term conditions (QALE).
- Discount to a net-present value (dQALY).
Full details of the method can be found in this accompanying technical note and the method is implemented for (currently) five countries in this spreadsheet tool.
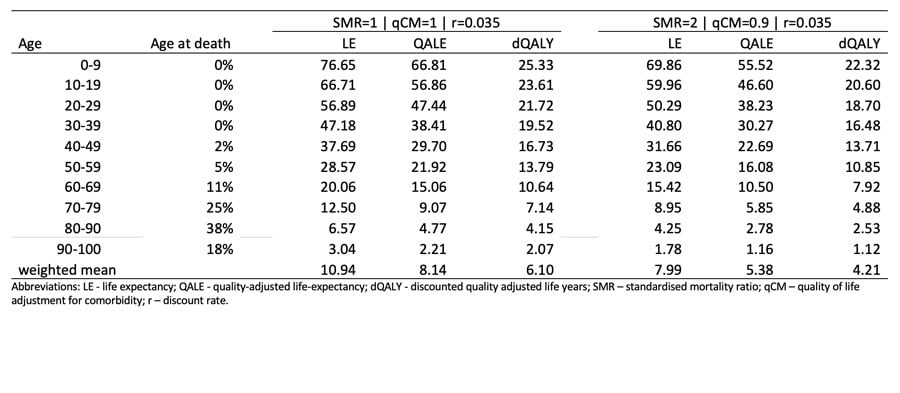
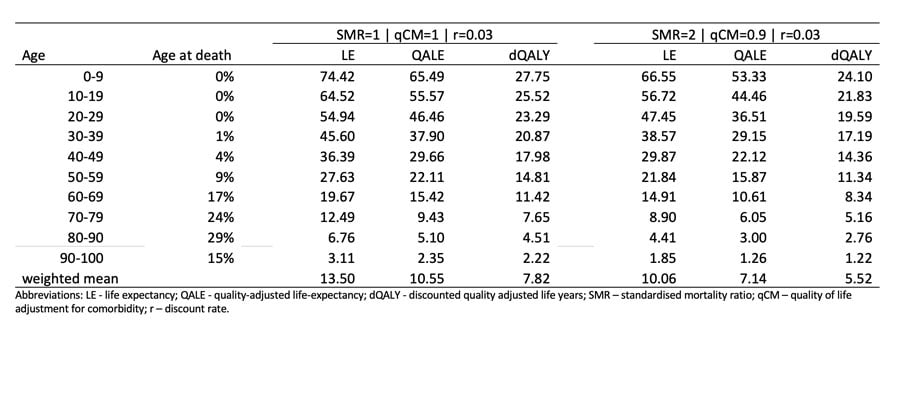
Some results from the approach are below. Table 1 shows the estimates based on UK data and Table 2 shows the equivalent estimates for US data. The underlying life tables come from ONS and CDC. The age distributions at death for COVID-19 victims also comes from ONS and CDC (these are being updated on a weekly basis and so the results below may not be the most contemporary estimates). Finally, the background norm quality of life data comes from chapter 3 of the book published by members of the EuroQol Group.
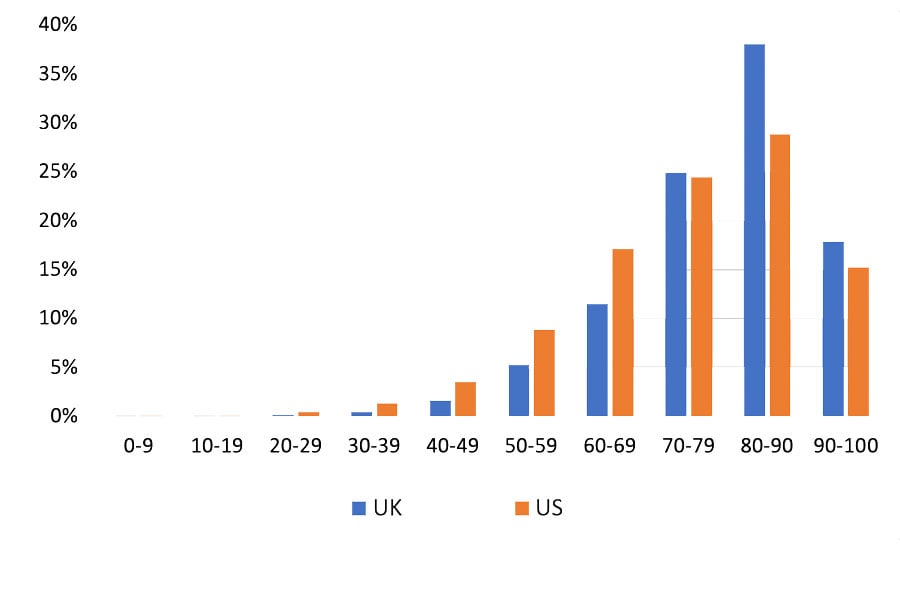
What we see from the comparison of the UK and US results is that the conditional life expectancies are broadly comparable and it is clear that even with a SMR of 2 and a 10% reduction on quality of life for the remainder of life to adjust for comorbidities, the life expectancy and (discounted) QALY losses remain substantial for all age groups. Small differences between the UK and the US relate to the data sources, but by far the most important difference is the pattern of age at death from COVID-19 between the two countries. These are illustrated in Figure 1 showing that the UK has a relatively higher proportion of older victims of COVID-19.
How might this approach be utilised? Apart from showing that it is unlikely, at least for most victims, that they would have succumbed to their long-term conditions in any case, the approach outlined can be used to explore the wider implications of the COVID-19 pandemic. For example, excess deaths have been widely reported and this approach could be used to explore whether the burden of excess deaths is greater than those from COVID itself.
An earlier version of this blog was highlighted in the linked article from the WSJ, although the focus of the article was on years of life lost without quality adjustment. More recently, a presentation based on this material was given as part of the ISPOR pre-conference plenary session on HEOR in the era of COVID-19 which was held on 14 May 2020. The video for the full session, including the panel of which this presentation was a part, can be found on the ISPOR website and you can also download a copy of the slides presented.
Table 1: Estimating the health burden associated with deaths from COVID-19 in the UK Table 2: Estimating the health burden associated with deaths from COVID-19 in the US Figure 1: Age distribution at death from COVID-19 in UK and US
- Count the cost of disability caused by COVID-19
-
The COVID-19 pandemic is well into its second year, but countries are only beginning to grapple with the lasting health crisis. In March, a UK consortium reported that 1 in 5 people who were hospitalized with the disease had a new disability after discharge1. A large US study found similar effects for both hospitalized and non-hospitalized people2. Among adults who were not hospitalized, 1 in 10 have ongoing symptoms 12 weeks after a positive test3. Treatment services for the long-term consequences of COVID-19 are already having to be absorbed into health and care systems urgently. Tackling this requires a much clearer picture of the burden of the disease than currently exists.
- Is there a role for RDTs as we live with COVID? An assessment of different strategies
-
We provide an overview of the potential impact of several RDT use cases (surveillance; testing, tracing and isolation without and with surveillance; hospital-based screening to reduce nosocomial COVID; and testing to enable earlier/expanded treatment) for a range of country settings. We use conceptual models and literature review to identify which use cases are likely to bring benefits and how these may change with outbreak characteristics. Impacts are measured through multiple outcomes related to gaining time, reducing the burden on the health system, and reducing deaths.