On April 15th, 2023, a violent clash started between the Sudanese Armed Forces (SAF) and the Rapid Support Forces (RSF) in Khartoum, marking a critical juncture in Sudan’s already turbulent socio-political landscape. Soon, the power struggle erupted into a large-scale armed conflict that overwhelmed the country. The proceeding violence has resulted in the world’s largest displacement crisis, extensive loss of life, and a humanitarian and hunger catastrophe.
A year into the conflict, prospects of a meaningful truce are profoundly grim, and the humanitarian emergency is growing ever more complex. Despite the scale of the crisis, international diplomatic and humanitarian responses remain wholly inadequate. As a result, the crisis in Sudan has been described as “neglected” and “forgotten” by UN officials and humanitarian agencies and professionals. The burden of the humanitarian response at the frontline rests on the shoulders of volunteers, medics and affected communities, with little attention or support from the humanitarian system. These groups need to be recognised for the critical role they play and better supported by the humanitarian system.
A humanitarian and health catastrophe
A year on, more than 5,506 incidents of political violence and 15,400 fatalities have been recorded in Sudan. An estimated 10.7 million people have been forcibly displaced inside and outside Sudan since the start of the conflict. The current conflict exacerbated an already dire humanitarian situation in Sudan, with the number of people needing humanitarian assistance skyrocketing. Humanitarian access is severely limited due to insecurity, bureaucratic impediments, and fuel shortages.
The health system, already strained by decades of instability and underfunding, faces severe challenges in responding to people’s health needs, with extensive destruction of health infrastructure, disrupted supply chains and staff shortages. The financial losses to the health system are estimated at $700 million, diminishing prospects for recovery. Concurrent cholera, measles, malaria, polio and dengue fever outbreaks were reported in 2023. About 65% of the population lacks access to healthcare, with only 2% of displaced populations having uninterrupted access. In conflict hotspots like Khartoum, less than a third of healthcare facilities are functional.
Minimal aid, maximum courage: local responders step up
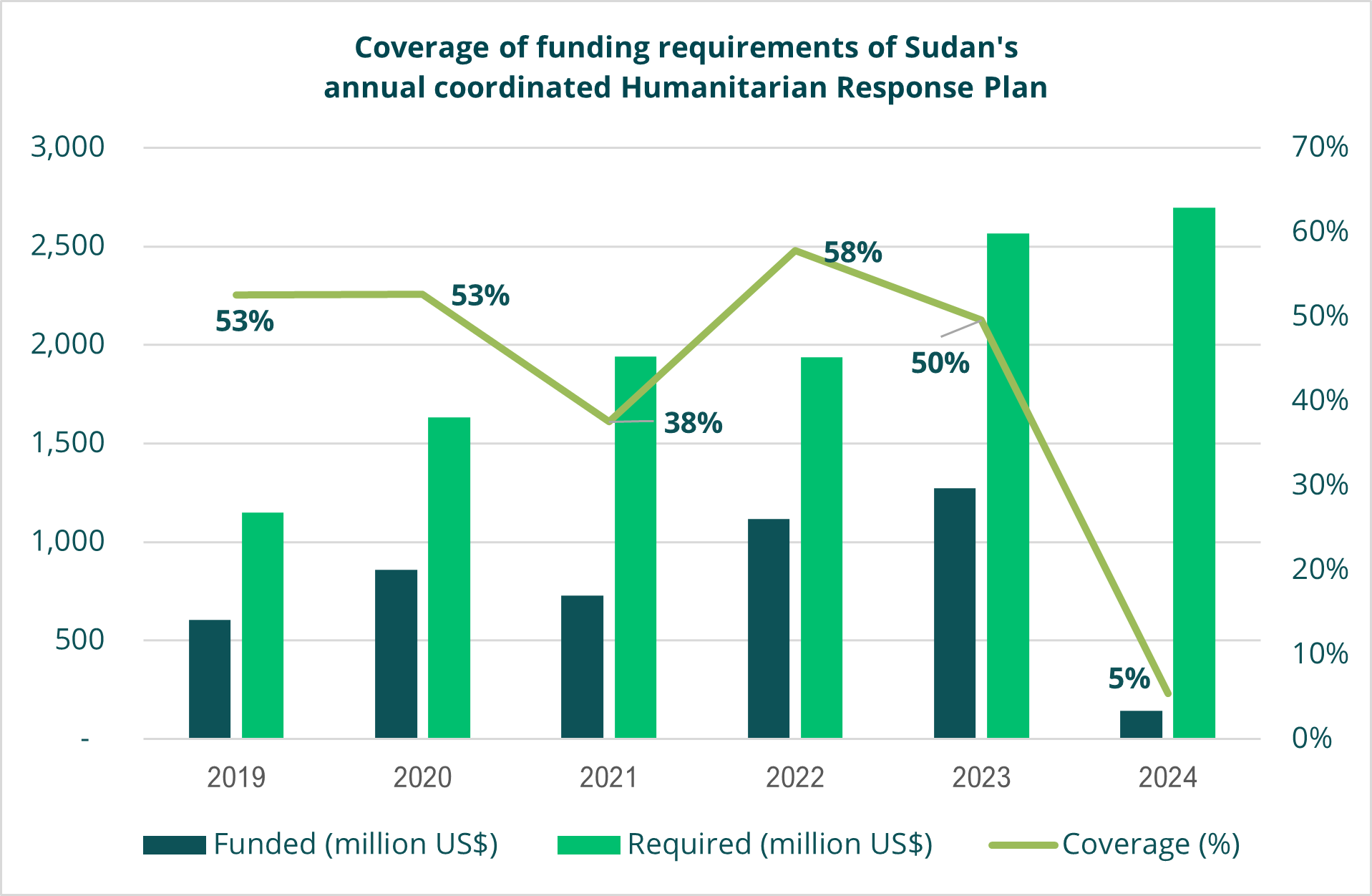
The international diplomatic response to resolve the conflict, hold the warring factions accountable for international humanitarian law violations and ensure civilian protection and access to humanitarian assistance has been underwhelming. Similarly, the humanitarian response has been severely underfunded (see Figure 1), and the operational presence of international and national NGOs has drastically shrunk due to safety, logistical and funding constraints.
Figure 1: Coverage of funding requirements of Sudan’s annual coordinated Humanitarian Response Plan (data source: UNOCHA Financial Tracking Service - https://fts.unocha.org/)
Local health responders play a pivotal role in meeting urgent health needs, embodying the long-standing Sudanese tradition of "Nafeer", community-led mutual aid. These local groups and Emergency Response Rooms (ERRs) include medics, volunteers and activists, who swiftly responded to the violence by setting up clinics and makeshift ambulances, securing medical supplies and supporting health workers. Many were pre-existing resistance committees fighting authoritarianism and state violence, reminiscent of the "humanitarian resistance" seen in Myanmar, Syria, and Ukraine. The Sudanese diaspora is a crucial source of financial and technical support to local health responders, similar to recent Ethiopian, Zimbabwean, and Syrian diaspora efforts. Sudanese medical professional organisations, both domestically and abroad, have also played a crucial role in advocating for political transition and documenting violence.
However, frontline health responders face daunting challenges. They confront security threats from the warring parties, experiencing assassinations, arrests, harassment, and asset confiscations. Financial support, primarily reliant on local and diaspora donations, falls short of meeting the extensive health needs and is aggravated by the collapse of the banking system and recurrent telecommunication blackouts. Coordination gaps, high turnover rates, and lack of technical expertise further strain their efforts.
Currently, funding and other support from institutional humanitarian health actors to local health responders is limited and inconsistent. Historically, foreign aid actors in the health sector have predominantly worked directly with the Sudanese authorities and resorted to direct funding and cooperation with Sudanese civil society during high-profile diplomatic tensions between donor governments and Sudanese authorities. In this conflict, challenges to forming stronger partnerships with local responders include fears of funding diversion by warring parties and concerns about financial accountability.
The need for a bold and innovative humanitarian response
In this past year, traditional health assistance models that flow primarily from international funding governments to international NGOs have failed to make a meaningful impact on excess morbidity and mortality in Sudan. There is increasing recognition of the contributions of local health responders; indeed, their courageous actions should be celebrated and acknowledged, and further funding and other forms of support should be channelled to them to meet the urgent health needs of crisis-affected civilians. However, this increased support should ensure:
- that assistance from institutional humanitarian actors to local groups and volunteers safeguards the autonomy and spontaneous nature of the local response and adopts a risk-sharing approach; and,
- strong and streamlined coordination between the Sudanese diaspora and institutional humanitarian health actors.
There is a common understanding in the humanitarian community that not enough is being done by international humanitarian donors, NGOs and the UN. There is an urgent need to drastically increase international funding and other humanitarian resources and improve international and national NGOs' operational presence in areas with easier access to crisis-affected populations. This must be matched by pressure from global and regional actors to ensure unfettered access to humanitarian assistance and civilian protection, as well as meaningful diplomatic efforts to resolve the conflict.
Our postgraduate taught courses provide health practitioners, clinicians, policy-makers, scientists and recent graduates with a world-class qualification in public and global health.
If you are coming to LSHTM to study a distance learning programme (PG Cert, PG Dip, MSc or individual modules) starting in 2024, you may be eligible for a 5% discount on your tuition fees.
These fee reduction schemes are available for a limited time only.