People who use opioids, including heroin, may delay seeking health services due to experiences of inequitable treatment in care. Delays in accessing care can lead to worse health outcomes for the individual as well as added strain on healthcare services. Qualitative research with people who use opioids suggests that a primary reason for delayed care-seeking is the lack of timely access to opioid substitution therapy to prevent withdrawal upon hospital admission. The iHOST study seeks to address this gap by implementing a five-pronged intervention to improve OST provision in acute hospital settings. The intervention has been co-developed with people who use opioids and other key stakeholders.
This project is funded by NIHR [HSDR NIHR133022]. The views expressed are those of the author(s) and not necessarily those of the NIHR or the DHSC.
We are a multi-disciplinary team with expertise in social science, pharmacy practice, implementation science and health economics who have a considerable track record of work in these areas.
We have been humbled by people sharing their personal and professional experiences in response to hearing or reading about iHOST. We would like to collect this feedback formally to learn from and help raise awareness. Please share experiences or feedback relevant to the iHOST project. Here you can indicate whether you are happy for anonymised quotes to be shared from your experiences on the iHOST site. We will not publish or share anything you send through to us without your permission.
Personal testimonials from people who use drugs and care providers are particularly welcome – by sharing your experiences (both good and bad) we can learn how to do things better, understand the challenges in providing and accessing care from a variety of perspectives, and highlight where change is needed.
If you have questions about this form or the project more generally, please email us ihost@lshtm.ac.uk.
What is iHOST?
iHOST is an intervention that aims to improve hospital care for people who use opioids by removing barriers to opioid withdrawal management.
The Intervention
The iHOST intervention involves five key components co-produced by people who use opioids. Each of these five components aims to improve access to OST for all people who use opioids. The five components are:
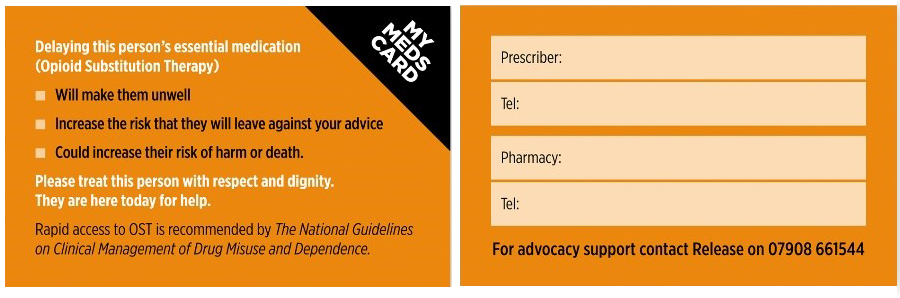
- ‘My Meds’ patient advocacy card;
- An OST advocacy and information helpline for people who use opioids and for hospital staff;
- An e-learning training module for hospital staff;
- A ‘best practice’ hospital OST policy template; and
- A local iHOST ‘champion. Each of these intervention components has been coproduced with relevant stakeholders, including people who use opioids.
- My Meds advocacy card
-
The card was developed through workshops with people who inject drugs in Camden, Finsbury Park and Brixton.
“like a helping hand. Something that speeds up the time you get your Methadone in hospital.”
“We need something like that [card] to take to the hospital to say I’ve got a right to be treated with dignity”
The advocacy card is credit card sized, double sided, and generic rather than personalised. It aims to:
- Empower people on OST to feel safe to access hospital care and to disclose their medication requirements.
- Enable timely medicines reconciliation: prescriber and pharmacist contacts to be entered by the drug service
- Support patients and staff with specialised OST advocacy and information (Release helpline).
No hospital will prescribe OST on the basis of the card alone. PWUD can choose to take or refuse a card (not mandatory).
- Advocacy helpline
-
The advocacy helpline, run by Release, aims to ensure that patients are supported in securing their community OST, in line with the hospital policy where the caller has been admitted. The advocacy helpline will also offer advice to hospital staff.
- Training module
-
The e-learning training module will offer hospital staff an introduction to providing equitable care in acute care settings. The training is designed to reduce stigma against people who use opioids, and to equip hospital staff in communication and de-escalation strategies. The training aims to improve understanding of the basic therapeutics and key safety around prescribing and administering OST. The training also includes an additional component to support local iHOST champion in taking up their role.
- ‘Best practice’ policy template
-
The ‘best practice’ guideline will be iteratively developed over the course of the iHOST project timeline. The aim of the 'best practice' guideline is to collate available evidence with insights from stakeholder consultation to promote the timely and effective management of opioid withdrawal symptoms in hospital. Our development of the 'best practice' guideline draws from the team's review of 101 existing hospital policies across England. In addition to this review, we also conducted a review of current national guidance from governing bodies such as NICE and the Department of Health and Social Care. The final 'best practice' guideline will be approved by key professional bodies and developed through robust engagement with people who use opioids as well as hospital staff.
UCLH guideline
As the first step in the 'best practice' guideline development process, we sought to revise existing guidelines at the pilot site, UCLH. The revised guideline was authored with support from the iHOST Policy Template Working Group, assembled of partners of the iHOST study, which met regularly to workshop the guideline's key provisions. The guideline's full development was guided by an Oversight Group, convened by the iHOST team with representation from key professional bodies, to refine and vet the guideline's final recommendations through facilitated workshops and written feedback. The final ‘best practice' guideline has also been revised and signed off by three committees of UCLH (the Opioid Stewardship Committee, the Use of Medicines Committee, and the Clinical Guidelines Committee). At its core, the guideline establishes four key changes to practice: 1) removing the urine screen requirement for OST prescription; 2) increasing the starting dose for initiating OST; 3) enabling takeaway OST for people who are already on a community OST prescription; and 4) providing takeaway naloxone to all patients prescribed OST in hospital.
- iHOST champion role
-
The iHOST champion(s) will support implementation of the iHOST intervention package in their local hospital setting, especially with respect to the training module and policy template. The iHOST champion(s) will promote uptake of the training module and, where relevant, alert colleagues to any changes made to local hospital policy and practice around OST provision. The iHOST champion role description has been co-produced with hospital staff including nurses.
What prompted the iHOST study?
iHOST responds to findings from the Care & Prevent study which aimed to understand risk and care practices for skin and soft tissue infections (SSTI) among people who inject drugs. This study generated survey data during 2017-2020 with 455 people who inject drugs in London, and in-depth interviews with 37 of these participants.
The Care and Prevent study found that a high proportion of participants (68%) reported experiencing an SSTI in their lifetime and nearly half (44%) of all participants with an SSTI had been hospitalised for this infection. Hospitalisation was associated with medical care delay: 28% reported taking 10 days or more to seek care after noting a SSTI symptom.
- Why were people taking so long to seek care?
-
Our qualitative interview data found that fear or experience of opioid withdrawal in the hospital system was a primary barrier to accessing and completing medical treatment. Even for people receiving a community OST prescription, delays in accessing their medication in hospital were lengthy, often leading to people self-discharging from hospital due to the distress of withdrawal.
“They give you a dose of Methadone in the hospital but you have to wait for the doctor to consent, so I'm waiting days, by the time I wait for the doctor I'm sick as a dog so I end up checking myself out to go and get drugs because I needed drugs because I'm kicking like Bruce Lee … I felt like I was going into convulsions, so I leave … sick as a dog, arm bandaged up, I have to go out and find some money to get high, thank God that I found something.”
(A quote from a participant of qualitative research that informed the iHOST study. This study has been published and is freely accessible)
“because if they didn’t give me Methadone … it was that that really scared me more than anything, was being sick in a hospital... I’ve been on it [using opioids] 11 years now, and being sick [in withdrawal] is one of the scariest things in the world to be.”
(A quote from a participant of qualitative research that informed the iHOST study. This study has been published and is freely accessible)
- What happened next?
-
We wanted to understand how hospital policy impacted OST provision, so we worked with stakeholders such as the Specialist Pharmacy Service to review the categorisation of OST as a ‘critical medicine’ and with project partner Release, we requested substance dependence management polices from all NHS hospital trusts. Read our analysis of these polices. We found that policies across the NHS differed widely, contained barriers to timely OST provision and could include punitive and stigmatising language. This work informed the policy template component of the iHOST intervention.
We then conducted three workshops with people who inject drugs in different parts of London to understand what would help them feel safer to access and complete hospital care. Participants in these workshops came up with the idea of the advocacy card and helpline which we further developed in conversation with a variety of stakeholders, including community members. More information about the My Meds Card and the Release advocacy helpline can be found above. Our research and conversations with hospital staff indicated the need for a dedicated training package to help inform better communication and provision of equitable care for people who use drugs in the hospital environment. With Exchange Supplies we developed an e-learning module with separate sections for clinical, non-clinical hospital staff and iHOST champions.
- What is a champion and why is this important?
-
An iHOST Champion is a clinical staff member who volunteers to become an advocate for people who use opioids (PWUO) and facilitates improved access to OST in their clinical area. iHOST champions take on an essential role of encouraging the adoption of the intervention, supporting new and existing colleagues to incorporate the intervention into their practice and be a practical source of local information e.g. signpost to community drug teams and local pharmacies.
If you are a clinical staff member at a participating site (University College London Hospital, St James's University Hospital and Royal Stoke University Hospital) and you would like to be an iHOST champion, please email ihost@lshtm.ac.uk.
iHOST study design
This research will test and evaluate the iHOST toolkit to scale nationally. The programme will be trialled at University College London Hospital from November 2022, before expanding to St James's University Hospital in Leeds and Royal Stoke University Hospital in Staffordshire.
This study has a quasi-experimental design and employs mixed methods to understand if iHOST works. There will be a few ways of understanding if this intervention has made a difference. The outcomes, which are the markers expected to change as a result of the intervention, are measured quantitatively (through hospital data sets at local hospital site and nationally across England) and qualitatively (through interviews, focus groups and observations with participants across the intervention).
There are two primary outcomes: Discharge Against Medical Advice (DAMA) and Emergency hospital readmission within 28 days of discharge.
There are four secondary outcomes: Reported inpatient illicit drug use; Time between admission; prescription of Opioid Substitution Therapy (OST) and receipt of OST; time taken to reach maximum OST dose; Provider knowledge and attitudinal change
We will then be able to see if there has been a difference in a patient outcomes. We will also seek to understand what parts of the intervention were key to these changes, what aspects were less important and how this differs according to the context of the intervention site. We will do this by through interviews, focus groups and observations. This will help us refine and develop the intervention further.
- Participatory research
-
The iHOST intervention was developed to address patient need, with intervention components, study methods and design workshopped in collaboration with people who use drugs, hospital nurses, consultants, community and hospital pharmacists and drug treatment providers. We continue to work with these stakeholders throughout the project, including through representation on the iHOST advisory committee.
We hold regular meetings with our ‘experts by experience’ group to provide updates and receive feedback on project progress. Together we have co-produced iHOST promotion materials aimed at people who use drugs and also hospital staff (UCLH leaflet) and (UCLH poster).
One of the central roles of this group of women and men with experience of opioid use and OST is to co-produce a ‘cultural safety’ framework based on their lived experience and project findings. This framework aims to inform providers of the changes necessary to develop a welcoming and safe hospital environment for people who use drugs living in the UK.
Peers are also involved in qualitative interview data collection and analysis, with support from the academic team. Towards the end of the project, we will hold output development workshops with people who use drugs in each study site to discuss study findings and co-produce outputs. Our experts by experience group will inform dissemination strategy, with a focus on delivering accessible resources, relevant to the needs of the communities we are working with, and for.
"The conscious or unconscious behaviours of people whose culture has the power to define service polices and practice may cause those from other cultural groups to feel powerlessness, anger and humiliation often resulting in avoidance of the service."
Cultural Safety in Nursing Education in Aotearoa by Irihapeti Ramsden
This research is guided by a framework called Cultural Safety. Cultural safety principles aim to reduce health care practices that cause marginalised patients to feel unsafe and powerless. Developed by nurse academics working with Maori patients in New Zealand , the concept of cultural safety has informed transformative care provision for indigenous populations globally, with recent work in North America extending this approach to reduce stigma and enhance equity of care for people who use drugs in hospital and primary care settings. We are inspired by this work, and aim – with our group of experts by experience – to develop a cultural safety framework informed by and relevant to the needs of people who use drugs in the United Kingdom.
-
Organisations participating in this study
-
The iHOST intervention has been co-developed with, and will be tested at the University College London Hospital from November 2022, before being evaluated at St James's University Hospital in Leeds and Royal Stoke University Hospital in Staffordshire. These large teaching hospitals provide different rural and urban contexts, each also have a high proportion of people who use drugs accessing their emergency and acute inpatient services.
The drug treatment services participating in London are situated in boroughs close to University College London Hospital. These are Better Lives Islington, Better Lives Seven Sisters, Westminster Turning Point and the Margarete Centre, Camden and Islington Foundation Trust.
The main drug treatment services participating in Leeds and Stoke are operated by Humankind: Staffordshire Treatment and Recovery Service (STARS), Forward Leeds.
The charity Release are providing the helpline.
The project is led by London School of Hygiene and Tropical Medicine with collaborating academic partners based at the University of Bristol, University College London, University College London Hospital, Liverpool John Moores University and the Bradford Institute of Health Research.
- Further information
-
The protocol is a document which outlines the plans for the study. This document describes the background, rationale, research methods, how the intervention will be delivered and the types of analysis that will be conducted to evaluate the study in full detail.

Magdalena
Harris
Prof of Inclusion Health (Sociology)
Magdalena is a sociologist in inclusion health based at LSHTM. She leads a mixed-method programme of research on health interventions for people who use heroin and crack cocaine in the UK, including through NIHR projects. She has 18 years’ experience in qualitative and participatory research with people who use drugs, holds the 2020 Society for the Study of Addiction Award for Impact on Policy and Practice and in 2022 was awarded a Membership through Distinction of the Faculty of Public Health.

Andrew Hayward
Director of the UCL Institute of Epidemiology & Health Care and NIHR Senior Investigator
Andrew is the Director of the UCL Institute of Epidemiology & Health Care and NIHR Senior Investigator, has over 20 years research experience on marginalised populations leading to policy change and service improvements.

Dan Lewer
Public health specialist and researcher
Dan is a public health specialist and researcher. He is an expert in analysis of data from hospitals, GPs, and other health services. Dan is leading the quantitative evaluation of iHOST.

Vivian Hope
Professor of Public Health, Public Health Institute, Liverpool John Moore University
Viv is currently Professor of Public Health at the Public Health Institute, Liverpool John Moore University. Prior to this he worked at Public Health England, and he has held academic posts at London School of Hygiene & Tropical Medicine, Imperial College London, and the University of Birmingham. He has over 25 years’ experience of research and public health practice focused on understanding the health issues associated with drug use and the responses to these. His research has focused on the harms associated with the injection of drugs, particularly infections, and preventing drug-related deaths. His research interests also include the use of human enhancement drugs, sexualised drug use, sexual health, and the well-being of LGBT+ communities.

Jenny Scott
Senior Lecturer in Primary Care
Jenny is a Senior Lecturer in Primary Care, and has expertise in intervention development in community pharmacies including online training development, previous clinical experience in hospital pharmacy and current clinical experience in a community drug treatment team.

Roz Gittins
Director of case standards and practice improvement
Roz primarily works for Westminster Drugs Project, a national treatment provider. She has clinical and research expertise in the management of substance use, psychiatry and pharmacy practice in primary and secondary care settings.

Alistair Story
Find and Treat lead for UCLH
Alistair is the Find and Treat lead for UCLH, co-ordinates a programme of outreach care for homeless, has published widely on inclusion health for marginalised populations and has extensive experience in operationalising public health interventions amongst vulnerable populations.

Adrian Noctor
Peer worker with UCLH Find and Treat
Adrian is a peer worker with UCLH Find and Treat. He has lived experience of OST, has received research training from MH, has experience in interviewing PWUO about hospital care access and will act as PPI lead.

Niamh Eastwood
Executive Director of Release
Niamh is Executive Director of Release, the UK’s centre of expertise on drugs and drugs law. Niamh has co-authored a number of Release’s policy papers including “A Quite Revolution: Drug Decriminalisation across the Globe" and "The Colour of Injustice: "Race’, drugs and law enforcement in England and Wales”. Niamh is an Associate Member of the Drug and Alcohol Research Centre, Middlesex University. She is also a committee member for DrugScience and has been a technical advisor to the Global Commission on Drug Policy. She is regularly asked to comment in the media on drug policy. Niamh started at Release as a legal advisor, supporting the legal rights of people who use drugs, especially those who have a history of drug dependency.

Mike Brown
Consultant physician/Clinical Director/Hon Associate Professor
Mike is a Consultant physician in Infectious Diseases and Acute Medicine, and Clinical Director, Division of Infection, UCLH, and Hon Associate Professor in the Clinical Research Dept at LSHTM, has led and published on improving diagnosis in vulnerable populations in acute hospital and primary care settings, and leads the Inclusion Health Strategic Forum at UCLH.
Penny Lewthwaite
Consultant in Infectious Diseases
Penny is a Consultant in Infectious Diseases, with a special interest in emerging infections, HIV, blood borne viruses and working to improve medical care delivery for patients who use opioids.
Ann-Marie Morris
Emergency Medicine Consultant and Deputy Medical Director
Ann-Marie is Emergency Medicine Consultant and Deputy Medical Director (Quality) at University Hospitals of North Midlands NHS Trust.

Andrew Preston
Founder of Exchange Supplies
Andrew Preston has been working in harm reduction for over 30 years. Following a decade of clinical practice as a community drug worker delivering OST and needle exchange, in 2002 he founded Social Enterprise Exchange Supplies to develop equipment to improve harm reduction by better serving the needs of people who inject drugs, and provide employment and training to people who inject drugs. Exchange Supplies provide on-site peer delivered needle and syringe programme for their local community, and are the equipment suppliers to the SIPP study sites.

Adam Holland
Public Health Physician/Research Fellow
Adam is a Public Health Physician and a Research Fellow at the University of Bristol and the London School of Hygiene and Tropical Medicine. He has research interests in the ethical and empirical arguments for different drug policy and harm reduction approaches and improving healthcare services for underserved populations who use drugs.
Nerissa
Tilouche
Research Fellow-iHOST Project
Nerissa is a Research Assistant at the London School of Hygiene & Tropical Medicine. She is supporting the research activities on the iHOST project.

Marisha Wickremsinhe
Research Fellow
Marisha Wickremsinhe is a bioethicist and qualitative researcher. Marisha leads the guideline development process for the iHOST study in her role as Research Fellow. Alongside Magdalena and Bean, she also conducts qualitative research for the iHOST study as part of the project's process evaluation.

Erica Smith
Advanced Clinical Practitioner
Erica is an RCEM credentialed Advanced Clinical Practitioner who works full time at the Emergency Department of the Royal Stoke hospital University Hospitals of North Midlands NHS trust. Erica has been an independent non-medical prescriber since 2014 and also guest lectures at Keele University on the health assessment module. Erica will be leading on the iHOST project at UHNM.
Stephen Parkin
Research Fellow
Stephen has an academic background in anthropology and sociology and has worked throughout the UK as a qualitative health researcher. He has over twenty years’ experience of conducting qualitative research with marginalised populations, including ethnographic studies of drug-using environments. In recent years he has provided qualitative research support to international mixed method studies of naloxone use (Europe, North America, and UK) and has conducted longitudinal qualitative studies of assorted intervention in England and Wales (including patient perspectives of long-acting injectable buprenorphine, and experiences of the ‘Everyone In’ policy initiative during COVID-19).

Adam Burns
Consultant
Adam Burns is a Consultant in Acute Medicine at Leeds Teaching Hospitals. He specializes in the initial assessment of treatment of adult medical patients presenting to hospital. This work is based primarily in the inpatient acute medical units, medical high observations (HOBS) unit and same day emergency care (SDEC). He also provides in-reach services to the emergency department. Adam’s clinical interests include the management of poisoning, drug toxicity and substance misuse. He is the author of trust guidelines for paracetamol poisoning and opiate substitution. He is a member of the trust drug and alcohol steering committee. Adam is also the lead for Acute and Critical Care at the University of Leeds and an Associate Dean for Quality with NHS England.
The Advisory Board
- Professor Anne Whittaker (Chair)
- Professor Sir John Strang
- Professor Peter Vickerman
- Dr Monica Desai
- Dr Tom Yates
- Dr Thomas Brothers
- Dr Chris Ford
- Dr Caitlin MacLeod
- Mr Peter Simonson (PPI member)
- Dr Chris Hallam (PPI member)
- Ms Erin O'Mara (PPI member)
- Study materials
These posters were iHOST promotion materials co-produced by the expert by experience group.
This leaflet was published when the study was launched at UCLH to share the importance of the iHOST study.
- Publications
Harris, M., Brathwaite, R., McGowan, C. et al. ‘Care and Prevent’: rationale for investigating skin and soft tissue infections and AA amyloidosis among people who inject drugs in London. Harm Reduct J 15, 23 (2018). https://doi.org/10.1186/s12954-018-0233-y
Wright, T., Hope, V., Ciccarone, D., et al. Prevalence and severity of abscesses and cellulitis, and their associations with other health outcomes, in a community-based study of people who inject drugs in London, UK. PLoS One. 2020 Jul 14;15(7):e0235350. https://doi.org/10.1371/journal.pone.0235350
Harris, M. Normalised pain and severe health care delay among people who inject drugs in London: Adapting cultural safety principles to promote care. Social Science & Medicine Volume 260, September 2020. https://doi.org/10.1016/j.socscimed.2020.113183
Harris, M., Holland, A., Lewer, D. et al. Barriers to management of opioid withdrawal in hospitals in England: a document analysis of hospital policies on the management of substance dependence. BMC Med 20, 151 (2022). https://doi.org/10.1186/s12916-022-02351-y
Lewer, D., Brown, M., Burns, A. et al. Improving hospital-based opioid substitution therapy (iHOST): protocol for a mixed-methods evaluation. [version 1; peer review: awaiting peer review]. NIHR Open Res 2024, 4:10. https://doi.org/10.3310/nihropenres.13534.1
- Presentations
Harris, M. Delayed care among people who inject drugs. Invited presentation. RCGP & SMMGP Managing Drug and Alcohol Problems in Primary Care Conference. 25-26 March 2021.
Harris, M & Noctor, A. Revolutionising care for people who use drugs in hospital settings: from Care & Prevent to iHOST. Inclusion Health Seminar Series. UCLH. 12 October 2021.
Harris, M. et al. Fear of inpatient opiate withdrawal: a modifiable barrier to health-care access for people who use illicit opiates. International Network on Health and Hepatitis in Substance Users Conference. 13-15 October 2021.
Harris, M. et al. Introducing an intervention to reduce late presentations, discharge against medical advice and repeat admissions among people who use opioids: the iHOST project. National Intelligence Network Meeting. Office for Health Improvement and Disparities. 4 March 2022.
Harris, M. Safe inhalation pipe provision (SIPP) & Improving Hospital Opioid Substitution Therapy (iHOST): two new interventions to improve access to care for people who use drugs. RCGP & AP Managing Drug and Alcohol Problems in Primary Care Conference. 24-25 March 2022.
Harris, M. Why service user involvement matters: in service delivery, planning & research. Medicines Optimisation and Prescribing in Complex Patients Module. Masters of Pharmacy Guest Lecture. University of Bath. 25 March 2022.
Harris, M. et al. Introducing iHOST and SIPP: Innovative research interventions to influence policy and improve care for people who use heroin and crack cocaine. Drug Science Symposium. London. 16 June 2022.
Holland, A. et al. Barriers to Management of Opioid Withdrawal in Hospitals in England: A Document Analysis of Hospital Policies. International Network on Health and Hepatitis in Substance Users Conference. 19-21 October 2022.
Harris, M. Introducing iHOST and SIPP: Innovative research interventions to influence policy and improve care for people who use heroin and crack cocaine. Evidence-Based Interventions Seminar Series, Department of Social Policy and Intervention, Oxford University. 15 November 2022.
Harris, M et al. Fear of inpatient opiate withdrawal: a modifiable barrier to health-care access for people who use illicit opiates. Lisbon Addictions Conference. 23-25 November 2022.
Harris, M & Wickremsinhe, M. Findings from the iHOST (Improving Hospital Opiate Substitution Therapy) project. RCGP & AP Managing Drugs & Alcohol Problems in Primary Care. 16-17 March 2023.
Harris, M. Transforming hospital care for people who use opioids: Implementing NHS policy change. Harm Reduction International conference (HR 23). Melbourne. 16-19 April 2023.
Harris, M. Improving opioid substitution treatment in the acute hospital setting. Royal College of Psychiatrists. Faculty of Addictions Psychiatry Annual Conference. 28 April 2023.
Harris, M. Improving health outcomes for people who use drugs: From research to policy and practice (Keynote speaker). Irish Street Medicine Symposium. 19-20 May 2023.
Harris, M. & Wickremsinhe, M. Re-orientating institutional perceptions of risk to meet the needs of people who use drugs: from Care & Prevent to iHOST. London Network of Nurses and Midwives Homelessness Group. 7th Annual Conference. 9 June 2023.
- Press
NIHR Evidence Alert - November 2022
Many hospital policies create barriers to good management of opioid withdrawal
BMJ Practice Alert – November 2022
Hospital policies can create barriers to good management of opioid withdrawal
University College London Hospitals (UCLH) Hospital news item on the launch of iHOST – November 2022
Research to improve hospital treatment for people who use opioids
University Hospitals of North Midlands (UHNM) Hospital news item on the launch of iHOST – 4 June 2024
UHNM in national project to improve hospital care of reported opioid-dependence patients
The Leeds Teaching Hospitals (LTHT) on the launch of iHOST – 5 June 2024
- Feedback
Letters - Hospital policies and opiate withdrawal
Joss Bray, a substance misuse specialist responded to the review in hospital policies on the management of opioid withdrawal.
The NIHR review of hospital policies on the management of opioid withdrawal is probably overdue.1 People who need opioid substitution therapy often have a difficult time in hospitals. Addiction is a strong driver to behave in certain ways, but I have found that using a competent and compassionate approach gives most people a positive and helpful experience of healthcare.
The finding that guidelines were often missing or not comprehensive enough clearly adds to the problem. I feel sorry for junior staff, who are expected to suddenly be proficient in something that medical school does not teach comprehensively and that senior doctors might want to avoid. I hope that the Improving Hospital Opioid Substitution Therapy project can go some way to remedying it, while emphasising the need for more teaching and a culture shift in attitude.
An important practical issue to highlight is that point of care instant urine drug tests (or, if unavailable, oral swabs) should be readily available in inpatient settings. They are not expensive and will provide extremely useful information—if interpreted correctly—to inform good and safe clinical care.
Footnotes
JB is founder of Competent Compassion (www.competentcompassion.org.uk), supporting an ethos that describes how a practitioner should interact with a service user to ensure a safe and effective intervention. Competing interests: None declared.
BMC Medicine volume 20, Article number: 151 (2022)
Review of hospital policies:
Magdalena Harris, Adam Holland, Dan Lewer, Michael Brown, Niamh Eastwood, Gary Sutton, Ben Sansom, Gabby Cruickshank, Molly Bradbury, Isabelle Guest & Jenny Scott
Feedback from a drug treatment service in London, August 2023
DAWs [Drug and Alcohol Wellbeing Service] have been pleased to work alongside iHOST in promoting the My Meds’ patient advocacy card which is just one of the project initiatives.
We have been providing the cards to residents and service users that we have contact with. Over the years it had been evident that OST [Opioid Substitution Therapy] was a barrier to those who we support accessing treatment in hospital due to their experiences and ongoing fear that they would be left to experience withdrawal when they did not receive the OST treatment. Through discussion the issues that service users experience in day centres and hostel we are able to promote hope for the client when they are in need of medical assistance and need to visit the hospital.
We have received positive feedback from clients that when they next go to hospital that they will not have to “suffer” – “I’ll have several cards please” one of the services ask, “I want to give to some friends”. A small card can make a big different to those in need.
Here you will find some questions you might have about the iHOST intervention such as; what is iHOST, who funds this research, why it is important or more general questions about opioid substitution therapy and understanding what withdrawal means.
- What is iHOST?
-
Improving Hospital Opioid Substitution Therapy (iHOST) is an intervention that aims to improve hospital care for people who use opioids by removing barriers to opioid withdrawal management. The project will co-produce, test and evaluate an intervention to make access to opioid substitution therapy (OST) timelier, more effective, and patient centred.
The intervention:
The iHOST intervention involves five key components:
- 'My Meds' patient advocacy card;
- An OST advocacy and information helpline for people who use opioids and for hospital staff;
- An e-learning training module for hospital staff;
- A 'best practice' hospital opioid substitution therapy policy template; and
- A local iHOST 'champion.
Each of these intervention components has been co-produced with relevant stakeholders, including people who use opioids.
Find out descriptions of the components and more detailed information presented in a presentation.
- Why is this study important?
-
The UK has highest rate of drug-related deaths in the European region and people who use drugs are at high risk of morbidity and mortality (1). Our research and international evidence shows that fear of opioid withdrawal is a barrier to timely hospital presentation and treatment completion among people who use illicit opioids, such as heroin, and/or who receive opioid substitution therapy (OST). Opioid Substitution Therapy (OST) is a medication-assisted intervention where patients are prescribed opioids such as methadone to alleviate symptoms of withdrawal, reduce drug use and help provide stability (2). There are an estimated 260,000 illicit opioid users in England (3) and over 140,000 people in England are on treatment (4). This is an ageing population, vulnerable to premature death, illness and infectious disease (5). People who use opioids have complex health needs and the rate of hospital admission in this population is several times greater than people of the same age in the general population (5).
Poor opioid withdrawal management, including breaks in continuity of care between community and hospital OST provision, can lead to discharge against medical advice, which is associated with emergency readmission in the following month (6). 1 in 14 opioid-related deaths in England happens in the two weeks after the hospital discharge (7).
Hospital-based interventions for the highly marginalised population of people who use illicit opioids, are therefore crucial.
(3) Public Health England "Opiate and crack cocaine use: prevalence estimates by local area"
(4) Statistics from the National Drug Treatment Monitoring System: (NDTMS)
- Where can I find more detailed information on the study?
-
The protocol is a document which outlines the plans for the study. This document describes the background, rationale, research methods, how the intervention will be delivered and the types of analysis that will be conducted to evaluate the study.
- What ethical approvals does the study have and is it registered?
-
This research has been approval by the NHS Health Research Authority, with details available for improving hospital OST. The study has been granted ethical approval by London - Camden & Kings Cross Research Ethics Committee (Reference: 22/LO/0370) and the London School of Hygiene and Tropical Medicine Ethics Committee (Reference: 27895)
The NHS Health Research Authority is a regulatory body that approves health and social care research, mostly in England, but also works closely with the other countries in the UK to provide a UK-wide system. Any research project that involves recruitment of NHS patients, staff, premises, resources (pharmacy, radiology or laboratories) or data/tissue in England must go through the HRA approval process, including ethical approval where appropriate.
The research is registered on the ISRCTN registry.
The ISRCTN registry is a primary clinical trial registry recognised by WHO and ICMJE that accepts all clinical research studies (whether proposed, ongoing or completed), providing content validation and curation and the unique identification number necessary for publication.
A systematic review on "How can access to opioid agonist therapy be improved in acute hospital settings?" is being conducted as part of this research. The review is registered on PROSPERO.
PROSPERO is an international database of prospectively registered systematic reviews of health and social care related research. See more information about the database. A systematic review is a piece of research that aims to identify, select and synthesis all research published on a particular question or topic. Systematic reviews follow a strict design that is planned in advance and this plan could be reproduced by another team of researchers.
- I would like to raise a concern about this research, who do I contact?
-
If you have a concern please contact Magdalena Harris, the Principal Investigator of the study, via email at magdalena.harris@lshtm.ac.uk or Aubrey Ko, the project manager at aubrey.ko@lshtm.ac.uk.
If you would like to make a formal complaint, you can do this by contacting the LSHTM Research Governance and Integrity Office at RGIO@lshtm.ac.uk or call 020 7927 2626.
- How can I find out the progress of this research?
-
The progress of the project, preliminary findings and research results will be reported in a variety of places including at external and publicly available methods such as conference presentations, peer-reviewed publications and community presentations. These will be made available on the outputs section of this website.
The progress of this research will also be shared at hospital sites that this intervention is being conducted in.
Please check out our twitter account @iHOSTstudy for updates, or email us at iHOST@lshtm.ac.uk if you would like to find out more or have publications sent to you.
- Who is the funder, and how do they decide what to fund?
-
The National Institute for Health Care and Research (NIHR) is funding this research. NIHR is the nation's largest funder of health and care research, spending £1 billion from the Department of Health and Social Care on research every year.
NIHRs work focuses on early translational research, clinical research and applied health and social care research. NIHR work in partnership with the NHS, universities, local government, other research funders, patients and the public, to fund, enable and deliver world-leading health and social care research that improves people's health and wellbeing and promotes economic growth.
Find out more information on NIHR fund research. Patients, members of the public, users of social care services and carers can get involved at all stages of NIHR research funding. Find out more about how to be involved.
This research comes under the research call for "19/165 HS&DR Injuries, accidents and urgent and emergency care" and started on March 2022 and is expected to finish in February 2025. The project reference for this is HSDR NIHR133022. The views expressed are those of the research team and not necessarily those of the NIHR or the DHSC.
- Who is conducting this research?
-
The multidisciplinary team working on this project represents advocates from national charities, clinicians and academics. Find out who is in the team.
The lead researcher (Principal Investigator) is Magdalena Harris who is based at the London School of Hygiene and Tropical Medicine. Magdalena leads a mixed-method programme of research on health intervention for people who use opioids in the UK, including through NIHR projects. She has 20 years' experience in qualitative and participatory research with people who use opioids.
- How will you know if the intervention makes a difference?
-
There will be a few ways of understanding if this intervention has made a difference. The outcomes, which are the markers expected to change as a result of the intervention, are measured quantitatively (through hospital data sets at local hospital site and nationally across England) and qualitatively (through interviews, focus groups and observations with participants across the intervention).
There are two primary outcomes: Discharge Against Medical Advice (DAMA) and Emergency hospital readmission within 28 days of discharge.
There are four further secondary outcomes: Reported inpatient illicit drug use; Time between admission; prescription of Opioid Substitution Therapy (OST) and receipt of OST; OST dose; Provider knowledge and attitudinal change
We will also seek to understand what parts of the intervention were key to these changes, what aspects were less important and how this differs according to the context of the intervention site. This will help us refine and develop the intervention further.
- Where are you carrying the study out? (What sites are you working with to test and evaluate iHOST?)
-
The three participating hospitals are: University College London Hospital, St James's University Hospital in Leeds and Royal Stoke University Hospital in Staffordshire. These sites have been selected to represent different geographical contexts and all experience a high proportion of people who use drugs accessing accident and emergency and acute inpatient admissions.
The drug treatment services participating in London are situated in boroughs close to University College London Hospital. These are Better Lives Islington, Better Lives Seven Sisters, Westminster Turning Point and the Margarete Centre, Camden and Islington Foundation Trust.
The main drug treatment services participating in Leeds and Stoke are operated by Humankind: Staffordshire Treatment and Recovery Service (STARS), Forward Leeds.
The charity Release are providing the helpline.
- Where do people get the cards and how are they expected to work?
-
'My Meds' patient advocacy cards will be provided to clients on Opioid Substitution Therapy (OST) at partner drug treatment intervention sites in London, Leeds, and Stoke. These drug treatment centres serve the local community near each hospital setting and are working in collaboration with the iHOST study to deliver this component of the intervention.
The My Meds cards have a dual function:
- To empower people to access hospital and advocate for their OST medication needs.
- To enable hospital providers to conduct speedy medicine reconciliation without delay and alert hospital providers to their needs for OST.
The card includes the advocacy helpline number for further assistance or information. The three hospitals that are participating in this intervention (University College London Hospital, St James's University Hospital in Leeds and Royal Stoke University Hospital in Stoke-on-Trent) are not expected to provide OST based on being shown this card alone.
- Who can access the helpline and how is it expected to work?
-
Anyone can access the helpline. It has been designed to support patients and staff in hospitals with OST provision who engage with the three participating hospitals of this intervention: University College London Hospital, St James's University Hospital in Leeds and Royal Stoke University Hospital in Stoke-on-Trent.
The helpline will be staffed by patient advocates who have a significant understanding of Opioid Substitution Therapy OST and, as partners in the project, have an understanding of the hospital's guidelines for patients accessing these medications, which may assist clinical staff.
0800 644 2999 - The hospital helpline, advertised on the 'My Meds' card, is operates between 9am-5pm.
07908 661544 - The helpline number can be texted to organise a call back in operating hours.
Details will be taken and Release staff will contact the relevant medical team and hospital pharmacist involved in the patients care, as well as liaising with the community drug services responsible for the patient's prescription.
The advocacy helpline is run by Release and aims to ensure that patients are supported in securing their community Opioid Substitution Therapy (OST), in line with the hospital policy where the caller has been admitted. Release has been providing advocacy and legal support to people who use drugs for over 50 years.
- Will this intervention be available across the NHS?
-
The intervention is currently only being conducted in the three participating sites: University College London Hospital, St James's University Hospital in Leeds and Royal Stoke University Hospital. After the iHOST intervention has been evaluated the team will make any changes or tweaks required, and dependent on the findings, will recommend it is implemented at scale across NHS acute hospital Foundation Trusts.
- What is the role of the drug treatment services?
-
Drug treatment services provide health care and support for people who are concerned about their use of drugs. In terms of the iHOST intervention, drug treatment services will hold a stock of 'My Meds' patient advocacy cards for people who use their service and receive OST.
The 'My Meds' card prototype was co-produced with people who use drugs and refined in collaboration with a variety of stakeholders, including drug treatment service providers. We have consulted drug treatment providers CGL, Turning Point, Humankind and NHS addiction services regarding implementation feasibility.
London Making Every Contact Count provides a list of community drug treatment services across London. Drug treatment services can be found at a national level.
Opioid Substitution Therapy (OST)
- What is opioid substitution therapy (OST)?
-
Opioid Substitution Therapy (OST) is a medication-assisted intervention where patients are prescribed opioids such as methadone to alleviate symptoms of withdrawal, reduce drug use and help provide stability.
OST is approved by National Institute for Health and Care Excellence (NICE) for the treatment of opioid dependence. The National Institute for Health and Care Excellence (NICE) provides national guidance and advice to improve health and social care. (1)
OST reduces the risk of all-cause mortality, including from opioid overdose, and reduces the risk of blood-borne virus transmission, including HIV and hepatitis C (2).
How is it prescribed?
Methadone is usually prescribed once-daily, with the initial daily dose of 20–30 mg that is later increased. Most methadone patients receive 60–120 mg of methadone per 24 hours, but some need higher doses.
How does OST work in a hospital setting?
When people who use heroin and other opiates are admitted to hospital, they usually need prompt medication e.g. opioid substitution therapy (OST) to prevent drug withdrawal. This is regardless of whether they are on a prescription for OST or not.
In hospital, the purpose of OST provision is to:
Prevent opioid withdrawal symptoms, Enable treatment of presenting medical condition(s), Reduce risk of self-management of withdrawal using illicit opioids in hospital, and Reduce risk of discharge against medical advice.
People who use opioids need access to OST in hospital to not only prevent withdrawal symptoms and a loss of tolerance, but also to ensure their wellbeing and ability to stay in hospital. Failure to offer opioid substitution therapy can contribute to decreased tolerance, thereby putting the patient at risk of fatal overdose upon discharge.
(2) 20. Public Health England. Guidance: Part 1: introducing opioid substitution treatment (OST). 2021.
- Opioid withdrawal is just like the flu, isn't it?
-
A common misconception is that symptoms of opioid withdrawal are relatively mild. However, people who use drugs report that experiences of opioid withdrawal are intolerable and far more significant than 'flu-like' symptoms. The fear of opioid withdrawal can be highly distressing and precede the actual onset of physical withdrawals. Rising panic and distress can be alleviated by knowing that withdrawals will be treated in a timely manner before they become severe.
In this project, we promote trusting people who use drugs, and trusting their accounts of opioid withdrawal symptoms.
- Why aren’t urine screens required in the iHOST guideline?
-
Through consultations with hospital staff, we identified time spent waiting for laboratory urinalysis as a prerequisite to OST prescription as a key barrier to timely OST access. However, a comprehensive patient history to determine opioid dependence and a physical observation to identify presence of withdrawal symptoms should be sufficient to indicate OST provision. Drug screens are designed to confirm recent opioid use, not to prove opioid dependence, and overreliance on testing combined with the possibility of false negative results may compromise timely and appropriate OST provision. Moreover, patients may experience drug screens as stigmatizing.
Where a drug screen is requested, either to enable further targeted discussion with the patient about their drug use or in cases of considerable uncertainty regarding the patient’s current opioid use, care should be taken to explain to the patient why testing is needed. The clinician should make clear that an appropriate and timely OST dose will be provided and that treatment of withdrawal symptoms will not be delayed by waiting for the test results. Drug tests should only be pursued with patient consent.
*Please note it is up to hospitals locally if they take up all elements of the guideline, and not all hospitals may take up all elements of the guideline developed by iHOST.
Hospital experiences for people who use drugs
- Will more people go to hospital to access drugs?
-
We want people to attend the hospital. The United Kingdom (UK) has the largest reported population of people who use non-prescribed opioids in Europe. The rate of emergency hospital admission in this population is several times greater than people of the same age in the general population, with most admissions relating to long-term health conditions, injuries and bacterial infections. Delays to seeking treatment are common and many admissions result in discharge against medical advice. Patients who leave hospital prematurely are more likely to be readmitted and have higher risk of death. Hospital discharge is a particularly risky time for people who use heroin as they may leave hospital in an unfamiliar neighbourhood and use drugs in public places, often while unwell and with reduced opioid tolerance, which are all risk factors for overdose.
People who inject drugs are often living with serious and painful health conditions but avoid care. Our research has found that people often delay care because they are worried about a health intervention that might harm them, but are particularly concerned about being judged and experiencing opioid withdrawal while hospitalised.
Some people are concerned that people who use drugs will come to hospital just to access OST. However, people who use drugs have greater access to drugs outside of the hospital rather than within it. People do not attend hospital to access drugs. Opioid substitution therapy helps manage the symptoms of withdrawal and does not lead to a euphoric effect.
- I am interested in reading more on this topic, what do you recommend that is freely accessible?
-
The academic publications below, which are freely accessible, are a good place to start.
They present the experiences of people who use drugs and the policies hospitals have on opioid substitution therapy.
- Normalised pain and severe health care delay among people who inject drugs in London: Adapting cultural safety principles to promote care
- Barriers to management of opioid withdrawal in hospitals in England: a document analysis of hospital policies on the management of substance dependence
Please contact ihost@lshtm.ac.uk if you would like to find out more or have publications sent to you.
Call Release on 0800 644 2999 or text "ihost" to 07908 661544 if you need support with your OST medication and you are based at UCLH.
Release will still be able to assist you if you are receiving hospital treatment somewhere other than UCLH. Release’s general helpline is 020 7324 2989.
What you need to know if you are a patient who is accessing the helpline:
If you are in University College London Hospital:
Our helpline for iHOST runs 7 days a week from 9am to 5pm.
If we hear from you during those hours we will give you a phone-call back after getting your text.
If we hear from you outside of these times, we will get back to you with a phone-call once we are back.
We know this is urgent and we appreciate you will need action now: if you have texted, you should have received an automatic text reply with advice about OST provision. You can show this text to the staff who are looking after you in hospital. The advice is written in line with the Department of Health’s Orange Guidelines (2017) and University College London Hospital’s local OST policy. It can also be found here:
The information above is written in line with the relevant guidance issued by the Government’s Department of Health – ‘Drug misuse and dependence: U.K. guidelines on clinical management’:
“Hospitalisation: For those dependent on opioids and in need of opioid substitution treatment (OST), provide reassurance, rapid assessment and suitable prescribing as soon as possible after admission, to facilitate their medical treatment as well as to manage the dependence. Appropriate communication between key professionals in hospital and in the community, particularly around time of entry to hospital and around discharge, is vital to ensure safe, effective and seamless care, including making appropriate plans for seamlessly and safely continuing OST prescribing in the community.” (Chapter 7: 7.5.1)
If you are at a different hospital:
The iHOST helpline supports people getting medical care from University College London Hospital. If you are receiving medical care elsewhere, someone from Release’s general drugs helpline will give you a call back as soon as possible. Sadly, Release’s general helpline does not run 7 days a week. We run Monday – Friday.
Release’s general helpline is run by the same staff as the iHOST helpline! However, as iHOST is a research project, it is currently only in place at University College London Hospital. The hospital you are receiving treatment from may have a different policy and requirements for you to get OST.
However, the same principle should apply: OST should be provided to any patient who is presenting symptoms of opioid withdrawal.