Antimicrobial resistance (AMR) is a leading cause of death around the world, with the highest burdens in low-resource settings. The World Health Organisation (WHO) has declared that AMR is one of the top 10 global public health threats facing humanity.
Researchers at the Medical Research Council Unit The Gambia at the London School of Hygiene & Tropical Medicine (MRCG at LSHTM) contributed to the first comprehensive assessment of the global burden of AMR, as well as an evaluation of the availability of data using major methodological innovations to provide new insights into the AMR burden.
The results of the study published in The Lancet, show that antimicrobial resistance caused an estimated 1.27 million deaths in 2019, and antimicrobial-resistant infections contributed to an estimated 4.95 million deaths globally. The estimates are based on an analysis of data from systematic literature reviews, hospital systems, surveillance systems and other sources.
The study used predictive statistical modelling to produce estimates of AMR burden for all locations, including for locations with no data. The approach can be divided into five broad components: number of deaths where infection played a role; the proportion of infectious deaths attributable to a given infectious syndrome; the proportion of infectious syndrome deaths attributable to a given pathogen; the percentage of a given pathogen resistant to an antibiotic of interest; and the excess risk of death or duration of an infection associated with this resistance.
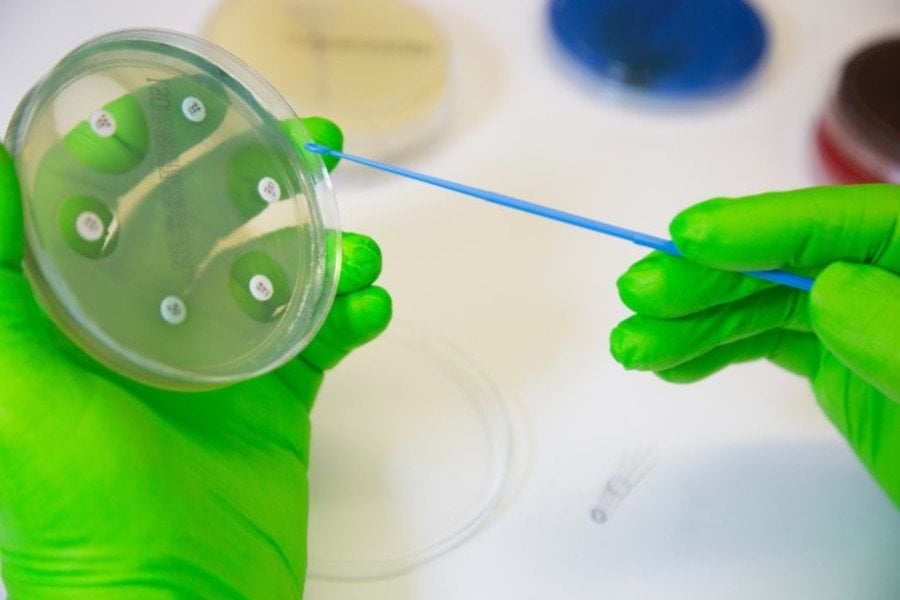
Saffiatou Darboe, Head of the Clinical Microbiology Laboratory at the MRCG at LSHTM said, “Antimicrobial resistance is an erupted volcano that should be taken seriously by all stakeholders before we run out of options. These figures from the analysis are quickly affirming the 10 million annual deaths previously predicted. The MRCG at LSHTM contributed both microbiology and clinical data to evaluate the impact of AMR. The Unit has recently invested heavily in its microbiological capabilities, and this will facilitate AMR surveillance.”
Dr Karen Forrest, Head of Clinical Services at the MRCG at LSHTM said, “We were able to contribute Gambian data to this study because of the excellent services provided by the microbiology diagnostic lab and the support of data management in developing our electronic medical record system. Antimicrobial resistance is a major concern, as it limits our ability to treat patients with infections that would otherwise be curable. The best way to reduce this risk is for each of us to think about how we use antibiotics. They should only be used when they are really needed.”
Dr Forrest added, “Antibiotics should not be taken by sick persons unless they have been prescribed by a doctor. We must accept and follow the advice from doctors and understand that not every infection is caused by a bacterium and not even every bacterial infection requires treatment. We also need to train our healthcare practitioners to know when they don’t need to prescribe these medications.”
Professor Anna Roca, Deputy Theme Leader for Disease Control & Elimination at the MRCG at LSHTM said, “As part of the Unit’s vision of leading research in our region to improve health across the world, we are committed to conducting research on the main health problems. As reflected in this publication, AMR is a major health thread. Generating surveillance data on the extent of the problem in each country and region is important to develop local policy decisions that will contribute to saving lives. Such data is lacking in many African countries. We have been able to contribute to this important milestone due to the decades of bacterial surveillance and thanks to the long-term investment in infrastructure and human capacity.”
Understanding the burden of AMR and the leading pathogen–drug combinations contributing to it is crucial to making informed and location-specific policy decisions, particularly about infection prevention and control programmes, access to essential antibiotics, and research and development of new vaccines and antibiotics.
However, there are serious data gaps in many low-income settings, emphasising the need to expand microbiology laboratory capacity and data collection systems to improve understanding of this important human health threat.
Publication
Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet (2022)
DOI: 10.1016/S0140-6736(21)02724-0
LSHTM's short courses provide opportunities to study specialised topics across a broad range of public and global health fields. From AMR to vaccines, travel medicine to clinical trials, and modelling to malaria, refresh your skills and join one of our short courses today.
