Many lower-level public facilities, the most common place of birth in Senegal, are unable to treat or refer women with obstetric complications, especially in rural areas, according to a new study published in BMJ Global Health.
A rising number of women in sub-Saharan Africa are giving birth in health facilities. This helps women to access emergency obstetric care rapidly, in case complications develop during birth. In Senegal, the percentage of facility births increased from 47% to 80% over the last 25 years. However, the study found that most of the increase in facility births (70%) was due to an increase in health posts and lower-level primary care facilities.
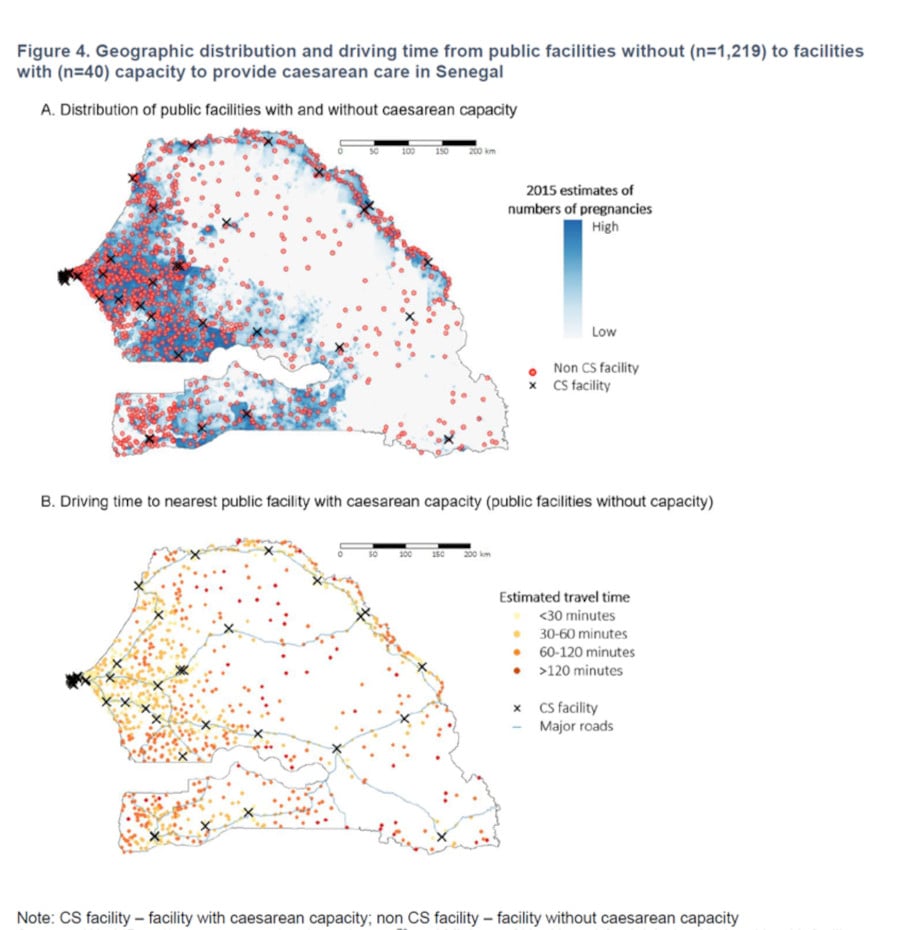
These health posts are only rarely able to provide emergency obstetric care; most cannot perform all basic emergency obstetric care elements (such as providing antibiotics for infections), and less than two thirds had access to a vehicle for referring patients to hospitals providing more advanced care, such as caesarean sections. In addition, health posts in rural areas are often remote: 37% of rural health posts were located more than one hour away from a hospital providing caesareans. Long referral times can be life-threatening for mothers and babies with obstetric emergencies.
These results highlight that encouraging births in primary care facilities may indeed help more women give birth in health facilities but may not always improve timely access to care if they develop complications. Improvements in emergency obstetric care and transport are needed in lower-level facilities, especially in rural areas, to accelerate reductions in maternal and perinatal deaths. Policymakers should also consider alternative health system configurations, where women give birth at higher level facilities.
The study was carried out in Senegal, using data from nine Demographic and Health Surveys between 1992 and 2017, to describe Emergency Obstetric Newborn Care (EmONC) and emergency referral readiness across facility levels in the public system, where 94% of facility births occur. A national global positioning system facility census was used to map access from lower-level facilities to the nearest facility performing caesareans.
Dr. Melisa Martinez-Alvarez, Senior Scientist at the MRC Unit The Gambia at the London School of Hygiene and Tropical Medicine said “Our study examined where women give birth in Senegal. We found that, despite substantial increases in facility-based deliveries, only 16% of births in the public health care system take place in facilities with either the full range of emergency obstetric care, or basic emergency obstetric care and referral capacity. We recommend countries and researchers go beyond encouraging facility-based deliveries to deliveries in facilities with the capacity to provide safe obstetric and newborn care.”
The study was carried out in collaboration with CEPED, Institut de Recherche pour le Développement in France ; Université Cheikh Anta Diop, Institut de Recherche en Santé, de Surveillance Epidémiologique et de Formations, among others
LSHTM's short courses provide opportunities to study specialised topics across a broad range of public and global health fields. From AMR to vaccines, travel medicine to clinical trials, and modelling to malaria, refresh your skills and join one of our short courses today.