Since the LSHTM Malaria Centre launched in 1998, those antimalarial drugs which were the mainstay of malaria treatment at that time have been largely abandoned because of resistance. Research during those 20 years has capitalised on rapid technological advances in genetics and genomics, investigating the molecular determinants of resistance and developing technologies to map the emergence and spread of drug resistance. Meanwhile, in the field, trials of malaria treatment efficacy and evaluations of treatment policy conducted at the Malaria Centre incorporated molecular genetic outcomes alongside the clinical, pharmacological, anthropological and economic ones. Among the many research approaches taken, we would like to emphasise the following themes of our work:
- The relationship between mutations and treatment outcome
-
Analysing the predictive association of molecular markers with disease severity, treatment outcome, transmission potential and their recurrence in breakthrough infections:
- Omar SA, Adagu IS, Gump DW, Ndaru NP, Warhurst DC. 2001. Plasmodium falciparum in Kenya: high prevalence of drug-resistance-associated polymorphisms in hospital admissions with severe malaria in an epidemic area. Ann Trop Med Parasitol 95: 661-9.
- Sutherland CJ, Alloueche A, Curtis J, Drakeley CJ, Ord R, Duraisingh M , Greenwood, BM, Pinder M, Warhurst, DC, Targett GAT. 2002. Gambian children successfully treated with chloroquine can harbour and transmit Plasmodium falciparum gametocytes carrying resistance genes. Am J Trop Med Hyg 67: 578-585.
- Hallett R, Sutherland CJ, Alexander N, Ord R, Jawara M, Drakeley C, Pinder M, Walraven G, Targett GAT, Alloueche A. 2004. Combination therapy counteracts the enhanced transmission of drug-resistant malaria parasites to mosquitoes Antimicrob. Agents Chemother 48: 3940-3943.
- Humphreys GA, Merinopoulos I, Ahmed J, Whitty CJM, Mutabingwa TK, Sutherland CJ, Hallett RL. 2007. Amodiaquine and artemether-lumefantrine select distinct alleles of the Plasmodium falciparum pfmdr1 gene in Tanzanian children treated for uncomplicated malaria Antimicr. Agents Chemother 51: 991-997.
- Beshir K, Sutherland CJ, Merinopoulos I, Durrani N, Leslie T, Rowland M, Hallett RL. 2010. Amodiaquine resistance in Plasmodium falciparum malaria is associated with the pfcrt 72-76 SVMNT allele in Afghanistan. Antimicrob. Agents Chemother 54: 3714-3716.
- Gadalla NB, Adam I, Elzaki SE, Bashir S, Mukhtar I, Oguike M, Gadalla A, Mansour F, Warhurst D, El-Sayed BB, Sutherland CJ. 2011. Increased pfmdr1 copy number and sequence polymorphisms in Plasmodium falciparum isolates from Sudanese malaria patients treated with artemether-lumefantrine. Antimicr Agents Chemother 55: 5408-5411.
- Henriques G, Hallett RL, Beshir KB, Gadalla NB, Johnson RE, Burrow R, van Schalkwyk DA, Sawa P, Omar SA, Clark TG, Bousema T, Sutherland CJ. 2014. Directional selection at the pfmdr1, pfcrt, pfubp1, and pfap2mu loci of Plasmodium falciparum in Kenyan children treated with ACT. J Infect Dis. 210: 2001-2008.
- Sutherland CJ, Lansdell P, Sanders M, Muwanguzi J, van Schalkwyk DA, Kaur H, Nolder D, Tucker J, Bennett HM, Otto TD, Berriman M, Patel TA, Lynn R, Gkrania-Klotsas E, Chiodini PL. 2017. pfk13-independent treatment failure in four imported cases of Plasmodium falciparum malaria treated with artemether-lumefantrine in the United Kingdom. Antimicrob Agents Chemother 61: e02382-16.
- The selection effect of specific antimalarial intervention policies
-
Including intermittent preventative therapy (IPT) and seasonal malaria chemoprevention (SMC), and combination therapy (CT) on the evolution of resistance:
- Cissé B, Sokhna C, Boulanger D, Milet J, Bâ EH, Richardson K, Hallett R, Sutherland C, Simondon K, Simondon F, Alexander N, Gaye O, Targett G, Lines J, Greenwood B, Trape J-F. 2005. Seasonal intermittent preventive treatment with artesunate and sulfadoxine-pyrimethamine prevents malaria in Senegalese children. Lancet 367: 659–67.
- Pearce RJ, Ord R, Kaur H, Lupala C, Schellenberg J, Shirima K, Manzi F, Alonso P, Tanner M, Mshinda H, Roper C, Schellenberg D. 2013. A community-randomized evaluation of the effect of intermittent preventive treatment in infants on antimalarial drug resistance in southern Tanzania. J Infect Dis 207: 848-59.
- Lo AC, Faye B, Ba el-H, Cisse B, Tine R, Abiola A, Ndiaye M, Ndiaye JL, Ndiaye D, Sokhna C, Gomis JF, Dieng Y, Faye O, Ndir O, Milligan P, Cairns M, Hallett R, Sutherland C, Gaye O. 2013. Prevalence of molecular markers of drug resistance in an area of seasonal malaria chemoprevention in children in Senegal. Malar J 12: 137.
- Oguike MC, Falade CO, Shu E, Enato IG, Watila I, Baba ES, Bruce J, Webster J, Hamade P, Meek S, Chandramohan D, Sutherland CJ, Warhurst D, Roper C. 2016. Molecular determinants of sulfadoxine-pyrimethamine resistance in Plasmodium falciparum in Nigeria and the regional emergence of dhps 431V. Int J Parasitol Drugs Drug Resist 6: 220-229.
- Allen L Malisa, Richard J Pearce, Ben M Mutayoba, Salim Abdulla, Hassan Mshinda, Patrick S Kachur, Peter Bloland and Cally Roper. The evolution of pyrimethamine resistant dhfr in Plasmodium falciparum of south-eastern Tanzania: comparing selection under SP alone vs SP+artesunate combination Malaria Journal (2011) 10:317 doi:10.1186/1475-2875-10-317.
- Allen Malisa, Richard Pearce, Salim Abdullah, Hassan Mshinda, Patrick Kachur, Peter Bloland and Cally Roper. Drug coverage in treatment of malaria and the consequences for resistance evolution-evidence from the use of sulphadoxine/pyrimethamine. Malaria Journal (2010) 9:190.
- Diallo, D.A., Sutherland C., Nebié, I., Konaté A.T., Ord R., Pota H., Roper C. Ilboudo-Sanogo E., Greenwood B.M., Cousens S.N. Sustained use of insecticide-treated curtains is not associated with greater circulation of drug resistant malaria parasites, or with higher risk of treatment failure among children with uncomplicated malaria in Burkina Faso. American Journal of Tropical Medicine and Hygiene (2007). 76(2) 237-244.
- Ravenhall, M. ; Benavente, E.D. ; Mipando, M. ; Jensen, A.T. ; Sutherland, C.J. ; Roper, C. ; Sepúlveda, N. ; Kwiatkowski, D.P. ; Montgomery, J. ; Phiri, K.S. ; Terlouw, A. ; Craig, A. ; Campino, S. ; Ocholla, H. ; Clark, T.G. ; Characterizing the impact of sustained sulfadoxine/pyrimethamine use upon the Plasmodium falciparum population in Malawi. Malar J (2016) 15(1):575.
- The impact of drug treatment on parasite resistance gene frequencies
-
Looking across different transmission seasons, and on parasite density dynamics within an individual patient:
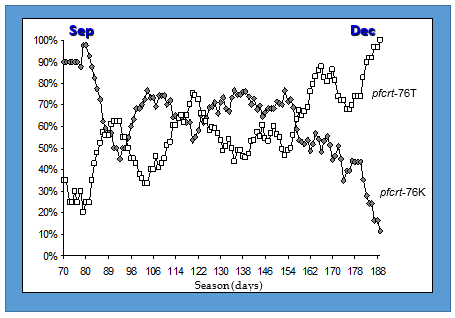
- Ord R, Alexander N, Dunyo S, Hallett RL, Jawara M, Targett GAT, Drakeley CJ & Sutherland CJ. 2007. Seasonal carriage of pfcrt and pfmdr1 alleles in Gambian Plasmodium falciparum imply reduced fitness of chloroquine-resistant parasites. J. Infect. Dis. 196: 1613–1619.
- Beshir K, Hallett RL, Eziefula AC, Bailey R, Watson J, Wright SG, Chiodini PL, Polley SD, Sutherland CJ. 2010. Measuring the efficacy of anti-malarial drugs in vivo: quantitative PCR measurement of parasite clearance. Malaria J. 9: 312.
- Beshir KB, Sutherland CJ, Sawa P, Drakeley CJ, Okell L, Mweresa CK, Omar SA, Shekalaghe SA, Kaur H, Ndaro A, Chilongola J, Schallig HD, Sauerwein RW, Hallett RL, Bousema T. 2013. Residual Plasmodium falciparum parasitemia in Kenyan children after artemisinin-combination therapy is associated with increased transmission to mosquitoes and parasite recurrence. J Infect Dis. 208: 2017-2024.
- Griffin, J.T.; Cairns, M.; Ghani, A.C.; Roper, C.; Schellenberg, D.; Carneiro, I.; Newman, R.D.; Grobusch, M.P.; Greenwood, B.; Chandramohan, D.; Gosling, R.D.; Protective efficacy of intermittent preventive treatment of malaria in infants (IPTi) using sulfadoxine-pyrimethamine and parasite resistance. PLoS One (2010) 5(9):e12618.
- Chico, R.M.; Cano, J.; Ariti, C.; Collier, T.J.; Chandramohan, D.; Roper, C.; Greenwood, B.; Influence of Malaria Transmission Intensity and the 581G Mutation on the Efficacy of Intermittent Preventive Treatment in Pregnancy: Systematic Review and Meta-analysis. Trop Med Int Health (2015) 20(12):1621-33.
- Mapping the continental and inter-continental dispersal of parasite resistance
-
Mapping from a single mutational event using resistance markers and linked polymorphic flanking sequences:
- Roper C, Pearce R, Bredenkamp B, Gumede J, Drakeley C, Mosha F, Chandramohan D, Sharp B. 2003. Antifolate antimalarial resistance in southeast Africa: a population-based analysis. Lancet 361: 1174-1181.
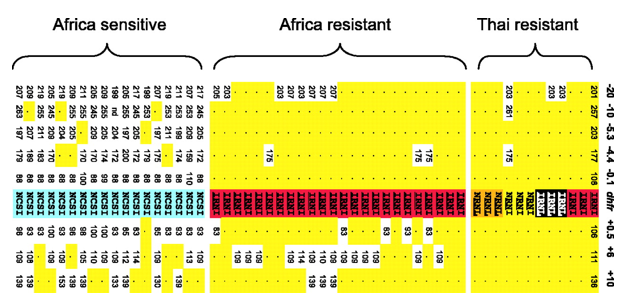
- Roper C, Pearce R, Nair S, Sharp B, Nosten F, Anderson T. 2004. Intercontinental spread of pyrimethamine-resistant malaria. Science 305: 1124.
- Pearce RJ, Pota H, Evehe MS, Bâ el-H, Mombo-Ngoma G, Malisa AL, Ord R, Inojosa W, Matondo A, Diallo DA, Mbacham W, van den Broek IV, Swarthout TD, Getachew A, Dejene S, Grobusch MP, Njie F, Dunyo S, Kweku M, Owusu-Agyei S, Chandramohan D, Bonnet M, Guthmann JP, Clarke S, Barnes KI, Streat E, Katokele ST, Uusiku P, Agboghoroma CO, Elegba OY, Cissé B, A-Elbasit IE, Giha HA, Kachur SP, Lynch C, Rwakimari JB, Chanda P, Hawela M, Sharp B, Naidoo I, Roper C. 2009. Multiple origins and regional dispersal of resistant dhps in African Plasmodium falciparum malaria. PLoS Med 6: e1000055.
- Corredor, V.; Murillo, C.; Echeverry, D.F.; Benavides, J.; Pearce, R.J.; Roper, C.; Guerra, A.P.; Osorio, L.; Origin and dissemination across Colombian Andes mountain range of Plasmodium falciparum Sulfadoxine-Pyrimethamine resistance. Antimicrob Agents Chemother (2010) 54(8):3121-5.
- Alifrangis, M.; Nag, S.; Schousboe, M.L.; Ishengoma, D.; Lusingu, J.; Pota, H.; Kavishe, R.A.; Pearce, R.; Ord, R.; Lynch, C.; Dejene, S.; Cox, J.; Rwakimari, J.; Minja, D.T.R.; Lemnge, M.M.; Roper, C. Independent Origin of Plasmodium falciparum Antifolate Super-Resistance, Uganda, Tanzania, and Ethiopia Emerging Infectious Diseases (2014) 20(8):1280-1286.
- Lynch, C.; Pearce, R.; Pota, H.; Cox, J.; Abeku, T.A.; Rwakimari, J.; Naidoo, I.; Tibenderana, J.; Roper, C.; Emergence of a dhfr Mutation Conferring High-Level Drug Resistance in Plasmodium falciparum Populations from Southwest Uganda. J Infect Dis (2008) 197(11):1598-1604.
- Lynch, C.A. ; Pearce, R. ; Pota, H. ; Egwang, C. ; Egwang, T. ; Bhasin, A. ; Cox, J. ; Abeku, T.A. ; Roper, C. ; Travel and the emergence of high-level drug resistance in Plasmodium falciparum in southwest Uganda: results from a population-based study. Malar J (2017) 16(1):150.
- Menegon, M.; Pearce, R.J.; Inojosa, W.O.; Pisani, V.; Abel, P.M.; Matondo, A.; Bisoffi, Z.; Majori, G.; Ord, R.; Warhurst, D.C.; Roper, C.; Severini, C.; Monitoring for multidrug-resistant Plasmodium falciparum isolates and analysis of pyrimethamine resistance evolution in Uige province, Angola. Trop Med Int Health (2009) 14(10):1251-7.
- Ndiaye, D.; Daily, J.P.; Sarr, O.; Ndir, O.; Gaye, O.; Mboup, S.; Roper, C.; Wirth, D.F. Defining the origin of Plasmodium falciparum resistant dhfr isolates in Senegal Acta Tropica (2006) 99(1):106-111.
- Systematic review and geo-referencing of resistance surveillance data
-
Systematic review and geo-referencing of resistance surveillance data to create publically accessible maps to inform malaria control policy:
- Naidoo I, Roper C. 2013. Mapping 'partially resistant', 'fully resistant', and 'super resistant' malaria. Trends Parasitol 29: 505-15.
- Naidoo, I.; Roper, C.; Drug resistance maps to guide intermittent preventive treatment of malaria in African infants. Parasitology (2011) 138(12):1469-79.
- Okell LC, Griffin JT, Roper C. 2017. Mapping sulphadoxine-pyrimethamine-resistant Plasmodium falciparum malaria in infected humans and in parasite populations in Africa. Sci Rep 7: 7389.
- The association between parasite genotype and in vitro drug susceptibility
-
The association between parasite genotype and in vitro drug susceptibility as an approach to validate potential resistance markers and test novel antimalarial compounds:
- Duraisingh MT, Roper C, Walliker D, Warhurst DC. 2000. Increased sensitivity to the antimalarials mefloquine and artemisinin is conferred by mutations in the pfmdr1 gene of Plasmodium falciparum. Mol Microbiol 36: 955-61.
- Omar SA, Bakari A, Owiti A, Adagu IS, Warhurst DC. 2001. Co-trimoxazole compared with sulfadoxine-pyrimethamine in the treatment of uncomplicated malaria in Kenyan children. Trans R Soc Trop Med Hyg 95: 657-60.
- Fivelman QL, Butcher GA, Adagu IS, Warhurst DC, Pasvol G. 2002. Malarone treatment failure and in vitro confirmation of resistance of Plasmodium falciparum isolate from Lagos, Nigeria. Malar J 1: 1.
- Fivelman QL, Adagu IS, Warhurst DC. 2004. Modified fixed-ratio isobologram method for studying in vitro interactions between atovaquone and proguanil or dihydroartemisinin against drug-resistant strains of Plasmodium falciparum. Antimicrob Agents Chemother 48: 4097-102.
- Fivelman QL, Adagu IS, Warhurst DC. 2007. Effects of piperaquine, chloroquine, and amodiaquine on drug uptake and of these in combination with dihydroartemisinin against drug-sensitive and -resistant Plasmodium falciparum strains. Antimicrob Agents Chemother 51: 2265-7.
- Van Schalkwyk DA, Burrow R, Henriques G, Gadalla NB, Beshir KB, Hasford C, Wright SG, Ding XC, Chiodini PL, Sutherland CJ. 2013. Culture-adapted Plasmodium falciparum isolates from UK travellers: in vitro drug sensitivity, clonality and drug resistance markers. Malaria J. 12: 320.
- Van Schalkwyk DA, Moon RW, Blasco B, Sutherland CJ. 2017. Comparison of the susceptibility of Plasmodium knowlesi and Plasmodium falciparum to antimalarial agents J Antimicr Chemotherapy 72: 3051-3058.
Our postgraduate taught courses provide health practitioners, clinicians, policy-makers, scientists and recent graduates with a world-class qualification in public and global health.
If you are coming to LSHTM to study a distance learning programme (PG Cert, PG Dip, MSc or individual modules) starting in 2024, you may be eligible for a 5% discount on your tuition fees.
These fee reduction schemes are available for a limited time only.