If you have been watching the hit television show ‘The Last of Us’ and have a new-found appreciation of the human health risk posed by fungal infections, you are not alone. In October 2022, the WHO released its first ever fungal priority pathogens list (FPPL) which included 19 species categorised as critical (n=4), high (7) and medium (8) priority. Priority species were categorised based on public health importance and research and development needs, with experts ranking antifungal resistance as the single most important R&D consideration.
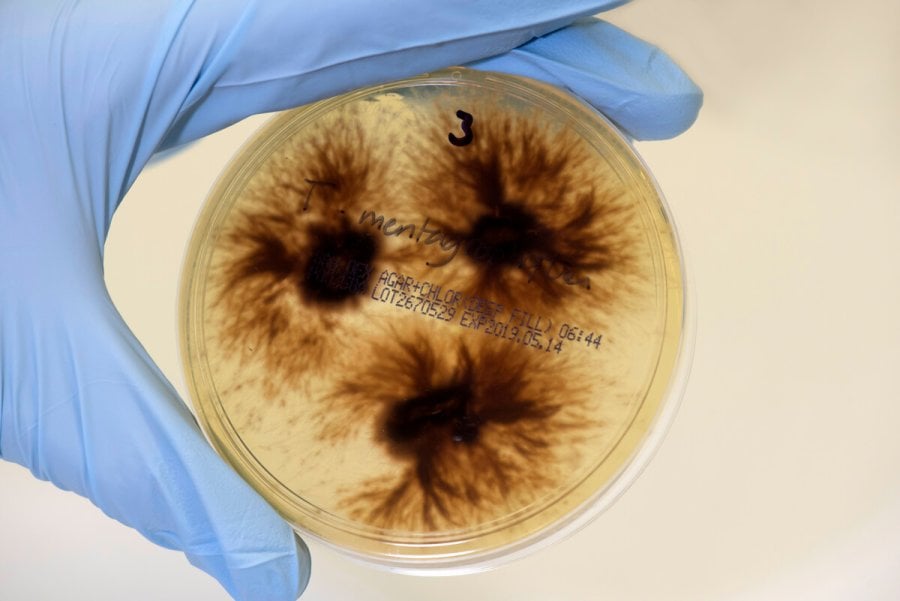
The WHO is not the only public health institution raising the alarm about the threat posed by fungal infections and antifungal resistance recently. This week, the US Centers for Disease Control published an article detailing a worrying rise in Candida auris cases during the COVID-19 pandemic. Between 2019 and 2021, annual clinical case counts reported to CDC tripled, with cases reported in 11 new states during this period. C. auris is in the critical priority group on WHO’s FPPL due to its potential to cause outbreaks, high mortality rate, and its intrinsic resistance to most available antifungal treatments. Further, antifungals that are currently effective in treating invasive candidiasis are unavailable in many countries. Over 80% of the C. auris isolated tested during 2020 were resistant to azoles, a common class of antifungal drug, representing a 7% increase in resistance between 2019 and 2020. CDC also noted an increase in the number of cases with reported resistance to echinocandins, the most frequently used first line antifungal used to treat C. auris infections, during the pandemic, though the overall prevalence of resistance remained low (<5% of all infections).
To address the growing threat posed by fungal infection and antifungal resistance, the WHO FPPL has identified three areas of action: (1) improve clinical and laboratory surveillance for fungal infections; (2) fund and support R&D initiatives, including for treatment and new diagnostics; and (3) enhance public health interventions, including to raise awareness of fungal infections.
Our postgraduate taught courses provide health practitioners, clinicians, policy-makers, scientists and recent graduates with a world-class qualification in public and global health.
If you are coming to LSHTM to study a distance learning programme (PG Cert, PG Dip, MSc or individual modules) starting in 2024, you may be eligible for a 5% discount on your tuition fees.
These fee reduction schemes are available for a limited time only.
