The COVID19 pandemic has had a huge impact on healthcare globally. The local impact on antimicrobial usage and resistance is evident in the English surveillance programme for antimicrobial utilisation and resistance (ESPAUR) 2020-2021 report, which was released on November 17.
Notably, data from the pandemic period show 2020 saw reductions in the incidence of blood stream infections with key AMR bacterial pathogens; reductions in the rate of resistance among E. coli and K. pneumoniae infections; and reductions in deaths attributable to AMR bacteria. There are many factors contributing to these macro-trends, including reduction in opportunities for person-to-person transmission and reduction in healthcare activities and procedures. Given recent data showing that overseas travel very frequently results in colonisation with AMR E. coli and Klebsiella, it is interesting to speculate that the huge reduction in overseas leisure and business travel may also have contributed to lower levels of AMR in the English community, and subsequently amongst opportunistic infections with E. coli and K. pneumoniae in hospitalised patients.
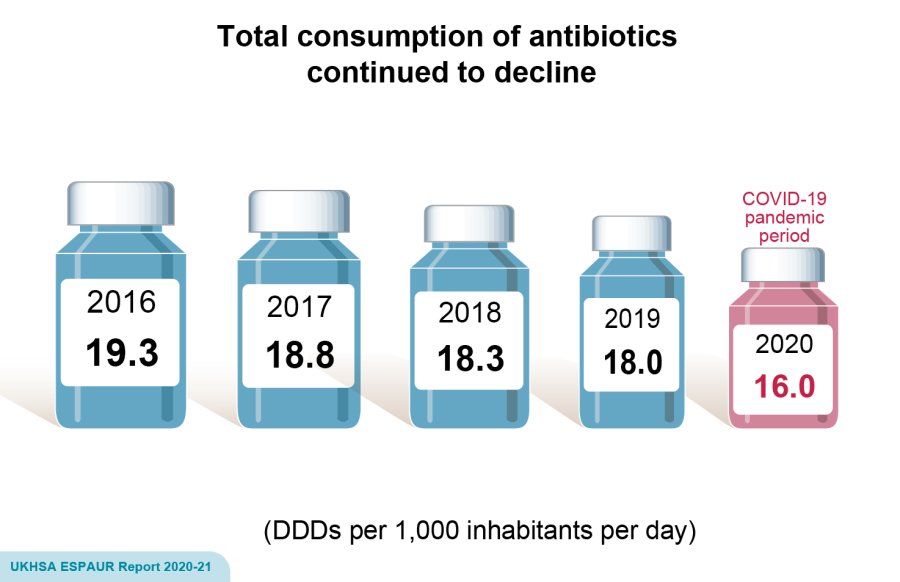
Usage data for 2020 show an accelerated decline in antimicrobial prescriptions by GPs (whom remain the leading prescribers), with the biggest change seen in children under 5 years of age (40% decrease) and those aged 5-9 years (26% decrease). However, for the first time, declines in usage were also observed in other community settings (24% decrease) and in hospitals (26% decrease for inpatients, 10% for outpatients). The usage of last-resort (reserve list) antibiotics increased by 16%, which could be explained by the dramatic shift in the make-up of inpatient populations.
Our postgraduate taught courses provide health practitioners, clinicians, policy-makers, scientists and recent graduates with a world-class qualification in public and global health.
If you are coming to LSHTM to study a distance learning programme (PG Cert, PG Dip, MSc or individual modules) starting in 2024, you may be eligible for a 5% discount on your tuition fees.
These fee reduction schemes are available for a limited time only.
