LSHTM research played a key role in supporting efforts towards global elimination of congenital syphilis and putting this neglected disease firmly on the agenda. During the REF period, the sustained impact of this research resulted in syphilis screening as part of antenatal care in all low- and middle-income countries, ensuring diagnosis and treatment of more pregnant women, fewer infant deaths attributed to syphilis, and elimination of mother-to-child transmission of syphilis in 13 countries. LSHTM studies in Africa provided key evidence of the health burden arising from pregnant women passing the infection to their babies while in the womb, and demonstrated the effectiveness of benzathine penicillin treatment. Further research evaluated new point-of-care tests (POCTs) for screening pregnant women for syphilis, as well as the feasibility and cost-effectiveness of these rapid diagnostics, leading to World Health Organization prequalification of POCTs and wide commercial availability.
Underpinning research
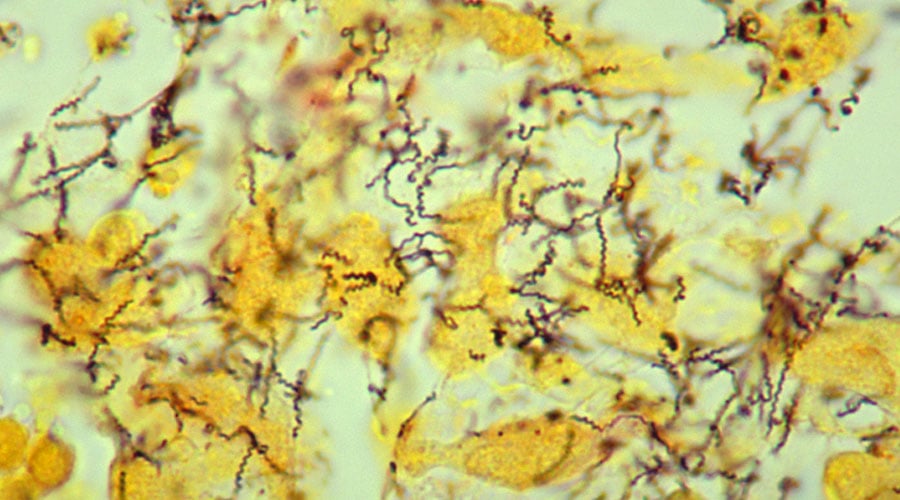
Syphilis was thought to be a disease of the past, but it remains a very common infection, with significant burden associated with mother-to-child transmission. There are approximately six million new cases each year and an additional risk of congenital transmission to babies by infected pregnant women who do not receive early and effective treatment. In 2004 it was estimated that, if stillbirths were included, 492,000 infants died of congenital syphilis each year in sub-Saharan Africa alone. Globally, approximately 460,000 abortions or stillbirths, 270,000 low birth weight babies and 270,000 cases of congenital syphilis are included in the burden of maternal infection attributable to syphilis each year. Research by LSHTM put congenital syphilis back on the global agenda, leading the way on evaluating and disseminating effective screening and treatment programmes.
Between 2001 and 2002, Professor Dr Deborah Watson-Jones carried out two landmark studies in Mwanza, Tanzania, documenting, for the first time since the 1950s, the incidence of adverse pregnancy outcomes in women with untreated syphilis. 380 previously unscreened women were recruited into a retrospective cohort and tested for syphilis. Results showed that in this setting, syphilis was responsible for 50% of stillbirths. A second study, a comparison of birth outcomes for 1,688 women, showed for the first time that single-dose treatment of benzathine penicillin before 28 weeks’ gestation prevented adverse pregnancy outcomes attributable to maternal syphilis. Subsequent research led by Dr Fern Terris-Prestholt compared the cost-effectiveness of on-site antenatal syphilis screening and treatment in Mwanza with other antenatal and child health interventions. Screening was found to be a highly cost-effective health intervention at USD10.5 per disability adjusted life year saved, if stillbirths are included.
In 2004 these studies were heavily cited in a special issue of the Bulletin of the WHO (Vol. 82-6, June), stimulating a resurgence of interest in congenital syphilis and shifting the research focus to barriers to effective control and treatment of the disease – the subject of concurrent research from LSHTM researchers. Their 2006 review of antenatal screening services in developing countries highlighted the poor integration of HIV and syphilis programmes and lack of access to treatment in remote settings. The tests used then required laboratory equipment and time to produce results. Interviews with stakeholders revealed that many women, particularly in remote areas, who tested positively for syphilis, never received treatment as they did not return for test results.
Following these findings, Professor David Mabey and Professor Rosanna Peeling led an evaluation of four new rapid serological tests, including the SD Bioline Syphilis 3.0, in 4 countries: Brazil, China, Haiti and Tanzania. They found that these POCTs were an acceptable alternative to conventional laboratory tests to diagnose syphilis. In addition, because POCTs did not require laboratory equipment or electricity, and could be performed on a finger-prick blood sample with results in 15 minutes, treatment could be administered at the first clinic visit, enabling increased coverage of syphilis treatment.
Between 2008 and 2012, the LSHTM team, in close collaboration with country programmes, led further research to assess the feasibility, cost and cost-effectiveness of scaling up the use of the rapid diagnostic tests in rural health facilities in China, Brazil, Tanzania, Uganda, Zambia, Peru and Haiti. Their findings indicated POCTs could be used in the most remote settings at an affordable cost.
In 2015, laboratory evaluations led by LSHTM in collaboration with the World Health Organization (WHO) demonstrated that the first dual POCT for HIV and syphilis showed optimal sensitivity and specificity for HIV diagnosis, and good sensitivity (between 89% and 100%) and specificity (between 91% and 100%) for syphilis (3.6). As a result, this POCT received WHO prequalification, but uptake was slow. The systematic review published in 2017 including these studies led WHO to commission workshops in 25 African countries and 8 countries in the Western Pacific Region to identify reasons for the testing gap and opportunities for increasing syphilis screening and treatment in pregnancy.
Details of the impact
LSHTM research underpinned the global strategy for the elimination of congenital syphilis, which saw worldwide rollout and success during this REF period. It brought this previously neglected disease on to the agenda through burden studies, and paved the way for an ambitious and effective programme of research on solutions. Progress in elimination has been accelerated via further pioneering LSHTM research on POCTs and tireless advocacy leading to declining syphilis rates (at a time when rates of other sexually transmitted infections have increased and greater access to and distribution of POCTs.
Input to target-setting, guidance and strategy
Following the dissemination of LSHTM’s 2002 Mwanza research, international momentum to eliminate congenital syphilis gained pace. This was underpinned by Watson-Jones’ findings on rates of adverse outcomes of untreated maternal syphilis, leading the WHO to launch a major new initiative for the global elimination of congenital syphilis in 2007. Her work subsequently informed, and was heavily cited in, the 2010 Centres for Disease Control and Prevention (CDC) and WHO ‘road map’ for the global elimination of syphilis, the 2012 WHO Investment Case for Eliminating Mother-to-child Transmission of Syphilis and the WHO Global Health Sector Strategy on Sexually Transmitted Infections, 2016-2021. While publication of some of these examples precede the current REF period, the impact of these programmes, guidance and strategies was wide-ranging and extended until 2020. Indeed, the last document called for a reduction of the congenital syphilis rate to less than 50 per 100,000 live births in all countries by 2030.
In 2017, WHO published guidance on the use of dual HIV/syphilis rapid diagnostic tests as interim advice for countries planning to introduce them in antenatal services and other testing sites. This guidance was also informed by Mabey and Peeling’s work. In 2019, the WHO released a policy brief recommending the rapid dual HIV/ syphilis test for pregnant women, including a checklist of issues to consider when implementing dual testing in order to maximise its benefits.
Increased testing and treatment
Following the LSHTM team’s rapid diagnostics evaluation study and their publication of the Lancet comment on ‘Avoiding HIV and dying of syphilis’, the Global Fund for AIDS, TB and Malaria announced it would fund country programmes to buy syphilis point of care tests, starting in 2007 and 2008. This was supported by the Global Congenital Syphilis Partnership, established in 2012 by Peeling at LSHTM. The partnership included global leaders in health and development such as the Bill and Melinda Gates Foundation, Save the Children, WHO and CDC, which provided technical support for the use and evaluation of dual HIV/syphilis POCTs.
In 2015, the SD BIOLINE HIV/syphilis dual test was accepted on the list of prequalified in vitro diagnostics based on laboratory evaluations of rapid tests led by LSHTM and WHO. The simple test required only a drop of blood from the patient’s finger and gave results in 15 minutes. It was offered to women at their first antenatal check-up. In 2019, a second test was awarded prequalification status after field studies showed optimal sensitivity and specificity for HIV diagnosis and good sensitivity and specificity for syphilis.
In collaboration with UNICEF and WHO, Peeling organised the 2018 workshops for maternal and child health programmes in 25 countries. They identified reasons for the gap in testing services and opportunities for increasing syphilis screening, and promoted policies for the use of diagnostics to eliminate mother-to-child transmission of HIV/syphilis. These workshops led to many countries, with donor and partner support, identifying reliable and predictable sources of additional funding. This allowed them to supplement existing HIV prevention of mother-to-child-transmission programmes to include dual HIV/syphilis testing and ensure a reliable supply of benzathine penicillin for treatment of syphilis. Following the workshops, countries including Uganda, Kenya and Nigeria updated their testing algorithm in 2018 to include the dual HIV/ syphilis POCT as the first routine test for pregnant women attending antenatal care services. The 2019 WHO progress report states that ‘strong progress had been made in reducing vertical transmission of syphilis during pregnancy through antenatal care programmes,’ and treatment coverage for syphilis among pregnant women was estimated to have increased to nearly 90% in 2016 and 2017 in the Americas region, a major success of the Global Health Strategy.
Major steps towards global elimination
In 2015, Cuba became the first country to be validated by WHO as having achieved the elimination of mother-to-child-transmission of HIV and syphilis, and in 2016, Thailand, Belarus and Moldova joined the list. In 2017, Anguilla, Antigua & Barbuda, Bermuda, Cayman Islands, Montserrat, St Christopher & Nevis were also validated as having achieved elimination, joined by Malaysia in 2018 and the Maldives and Sri Lanka in 2019.
A 2019 WHO publication reviewed changes in the global burden of maternal and congenital syphilis associated adverse birth outcomes between 2012 and 2016. The estimated total number of congenital syphilis cases was reduced by 12% over this four-year period, reflecting the progress made in a previously neglected area. The authors concluded that the decrease in congenital syphilis cases was due to increased access to syphilis screening and treatment in antenatal clinics worldwide. The WHO stated in their Progress report on HIV, viral hepatitis and sexually transmitted diseases that in 2017, 100% of low- and middle-income countries included syphilis screening in their antenatal care package. This, plus increased attendance at antenatal appointments, increased syphilis testing coverage among pregnant women at their appointments, and increased syphilis treatment coverage to save babies’ lives, can be significantly attributed to the extensive LSHTM research which evaluated POCTs and demonstrated their low cost and accessibility.