Tricky one to start, can you summarise the paper in one sentence?
There’s some uncertainty and confusion around the effects statins may have on general muscle symptoms.
The key finding and the summary of the paper is that that statins have no overall effect on the frequency or severity of muscle symptoms compared to placebo in people who had previously reported that they had muscle symptoms from statins.
Why are statins important, what do they do?
Statins work to lower certain types of cholesterol in the bloodstream. Not all cholesterol is bad - there was this mid-90’s popular idea that, ‘all cholesterol is horrendous, and that we should egg-white omelettes only’. That wasn’t a complete picture – we do need some types of cholesterol in our bodies.
But, there are certain types of cholesterol that can be harmful and can build up and cause narrowing of the arteries. What statins do is control that harmful cholesterol. Because of this, they’re important in reducing heart attacks, strokes, other serious cardiovascular disease.
And the really great thing about statins is that they work across all age ranges, genders – a wide demographic – and have been shown to be effective at reducing the risk of a serious cardiovascular event in all of these people.
And do you have any figures for how many people are on statins in the UK currently?
The British Heart Foundation estimates that between seven and eight million people in the UK are currently on statins. It’s one of the most commonly, if not the most commonly prescribed medication in the UK. There are a few different types of statins, but as a class of medication, statins are well up there.
Is this research only related and applicable to this specific statin you looked at?
We focused on one specific statin called atorvastatin at a 20mg/day dose.
It’s the most common statin to be prescribed in the UK and the dose we used is the standard preventative dose most people are given. With the caveat that following significant cardiovascular events, for example heart attacks, you may see higher doses used. We wouldn’t expect the result of the study to change with different statins because the differences in the medications aren’t significant. But it may be a different case with the dosing, a higher dose may produce different results. This is a known limitation of our study and area for future research.
And you were looking at one of the reported side effects – muscle symptoms. What do you mean by muscle symptoms, and why was it important to study this?
We left muscle symptoms intentionally broad as an outcome and measurement. One of the important features of the study is that it’s driven by patient reported outcomes. Meaning we leave the interpretation of ‘muscle symptom’ up to the patient. It can mean very different things to different people. If we clarified it by saying, ‘we mean muscle pain’, people may think, ‘oh but its not pain, its stiffness… I don’t know if I report that?’.
It is broad, but that’s because we’re including muscle pain, stiffness, tenderness, weakness, aches and things like that.
This is important because muscle symptoms are the typically assumed, known about, side effect that leads people to discontinue statins.
The focus on the muscle is targeted for the study and relevant. When we were recruiting people into the study, one of the criteria they had to meet was that they either had stopped, or were considering stopping, their statins because of muscle symptoms. In other words – we enriched the patient population in the study with people who had concerns about this specific side effect.
Why did you pick people who already had concerns around muscles?
The study would have been feasible with a broader population. But from a scientific perspective, having people who were already aware of the muscle-symptoms related to their statin use was important.
Sometimes in clinical trials we think we need thousands of people, but what we actually need are events, people who have the thing you’re looking to study. This is a focussed study on people who had muscle symptoms.
But it is important to note that people who agreed to join the study had an open mind about exploring their muscle symptoms. People who are strongly convinced about the link are not going to be re-willing to go back on stains for the study, and those people can be hard to reach. But we’re hoping this research can help to reassure some of those people.
Where did the belief that statins are associated with these symptoms originate?
I’ve been thinking about this. And like many of these complex issues, it’s probably hard to pinpoint a single ‘original sin’ so to speak. There were some unblinded observational studies that suggested a link and this was exacerbated by media outlets around the world who reported the idea that statins were causing muscle symptoms. And that’s why I think we needed the methodology we used. To really interrogate the question more closely and try and understand why this belief has seeped into the public consciousness.
Okay, to the paper – how did you test the theory?
Yes! I love this bit – this is the methodology side of things and I think it’s really cool!
The classical clinical trial is that you get a bunch of people, you split them in half. Half get treatment, half get a placebo or control, and you don’t tell them which is getting which. Then they get followed up. Now, this is a great straightforward way of running a clinical trial. But it didn’t make sense in this context. There could be ethical concerns about taking people off statins who were already on statins and it would be expensive.
In this case we used an N-of-1 trial. N is the sample size. And usually if you have an N-of-1, people might be a bit dismissive of it – ‘you only looked at one person’. But in this case, it’s what made the trial so powerful.
You have one person. You get to compare within that person the impacts of statin versus placebo on muscle symptoms. And you get to do that multiple times. It’s a direct comparison, as all of the other variables are controlled for – it’s not attempting to compare two disparate groups of people.
But then we also get to compare all of these individual trials into one big analysis. StatinWISE is a series of 200 N-of-1 trials, which we then combine to make broader conclusions.
An important thing to note is that we double blinded it – the participant didn’t know what they were receiving (either atorvastatin or placebo), we didn’t know as a co-ordinating team, and the doctors and nurses at their GP practice didn’t know.
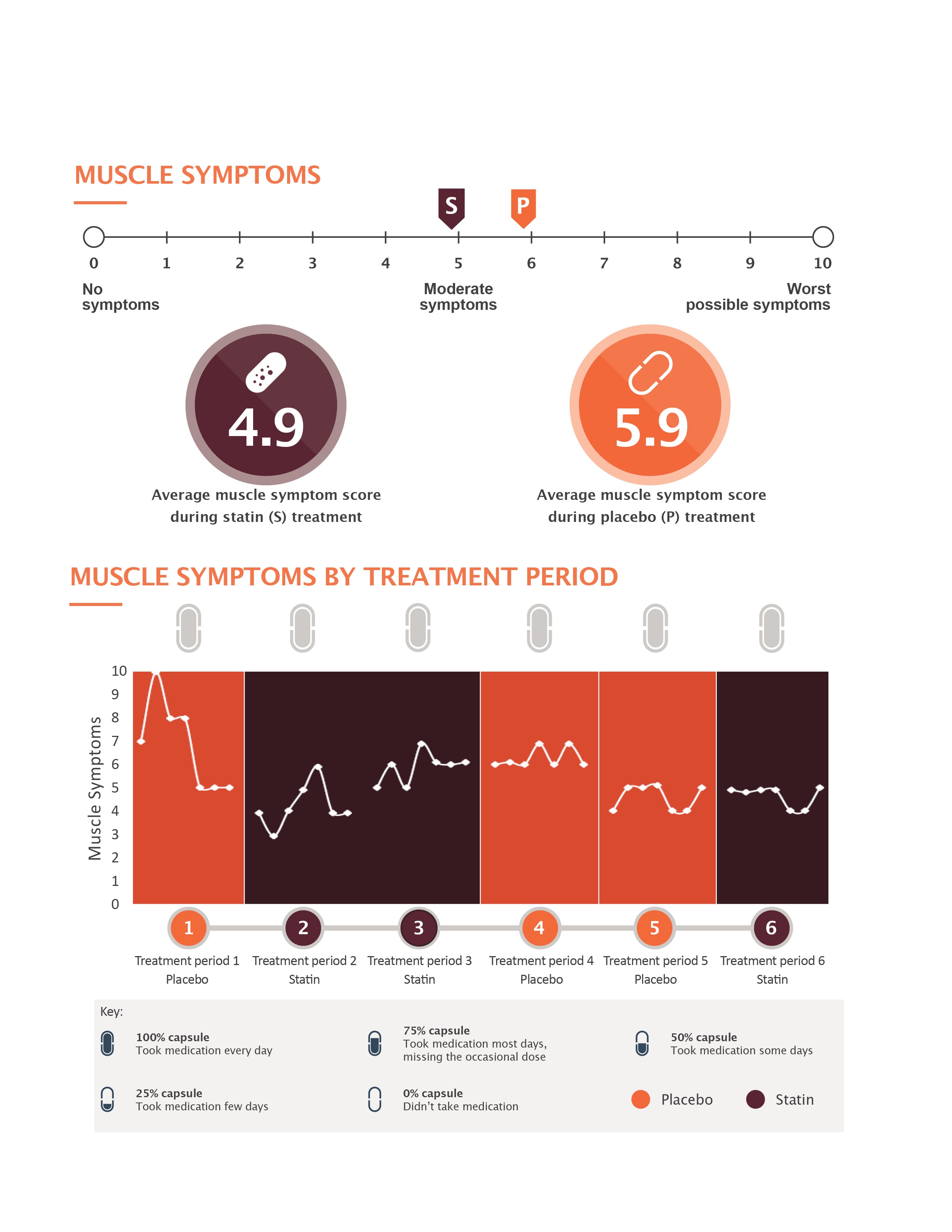
We posted out the packs every two months, and they had six treatment periods. They were randomly split up as to which was one going to be statin and which one was going to be placebo.
This is a powerful research design – we went back and forth within each patient for a whole year in two-month periods which gave us a really strong internal comparison. But then also different treatment periods among all participants to put into the main combined analysis.
Aside from the methodology, one of the coolest things about the trial was the team effort. We work together across LSHTM and participating research sites - this collaboration is vital for success.
And your key findings were…?
The key finding is that we found no difference in muscle symptoms in patients whether they were on statin or placebo.
Beyond muscle symptoms, we also asked patients about impact on other parts of their life. Mood, ability to walk, work, sleep, general activity, enjoyment of life, and interpersonal relationships. We scored these as well, and found the same as with muscle symptoms– that statins had no impact on.
We provided individual results to everyone who completed the trial. They reported that it was helpful information, and two-thirds planned on restarting the statin. Given the benefits we know about statins, and from a public and individual health perspective, this is a very positive thing.
How would you advise this data is used by patients and medical professionals?
As a group of researchers, we hope that the combined analysis will be taken forward by patients as reassurance. We hope health care providers can use this to help explain that the benefits far outweigh the risks, and that the statins are not the cause of the muscle symptoms they may be experiencing.
A note of caution here though – there is a very rare side effect, about 1 in every 10,000 people may experience with statins is very severe muscle pains. But that is a different thing to the more generalised symptoms.
StainWISE trial results explained
You said that people who took part found seeing their results helpful in decision making, could we be using this more in clinical settings?
Yes, another really beneficial side to this type of study, is that the individual results of each N of 1 trial are really useful for guiding the treatment of each individual person. We shared the results with the people involved so they could take that to their healthcare providers and use it to discuss whether they wanted to go back on statins.
I think this kind of study could play an important role - clinical care and research are different fields but could be more closely aligned. This would make research more generalisable and easier to conduct. Learning more about the best way to treat people and how people need and want to be treated is vital.
But we don’t want the research to slow down the care. So this particular methodology could at some point be used to help medical professionals and their patients better interrogate the question – ‘is this working for you?’.
Unfortunately right now, it’s not available on the NHS – but who knows in future?
And what about people who have experienced muscle symptoms – are we saying this doesn’t actually happen? Or is there another explanation?
That really is the crux of it. Its key to stress that the aches, pains and symptoms people are experiencing are real. We’re definitely not saying ‘it’s all in your head’. The symptoms are there but we’ve shown that they aren’t caused by statins.
It’s a fact that as people get older, aches and pains become more frequent. It may be that statin use happens to coincide with a time in life when muscle symptoms become more common. And it may be hard to specifically determine where those pains come from – but what we can say from this study, is that they’re not being specifically caused by statin use.
I guess in its own way that’s quite important. By demonstrating that statins aren’t the root cause of these symptoms, it then gives people the opportunity to explore other avenues?
That’s true! And it also could be that patients get put in an impossible dilemma – they’re told statins are good for them and help prevent cardiovascular disease, but they also think they cause muscle pain. There’s the worry that coming off of them may lead to a stroke or heart attack, but staying on them might lead to pain.
In a broad sense, this should reassure people that they’re safe taking statins, statins aren’t causing their muscle symptoms, and they can continue to have the benefits!
What’s next for you in this work?
In terms of this work, we have more data to look at and think about. Long term, we plan to bring this N of 1 methodology into clinical practice! And then, personally, there have some other trials in UK cardiovascular care that I’m quite excited about running and reporting.
Our postgraduate taught courses provide health practitioners, clinicians, policy-makers, scientists and recent graduates with a world-class qualification in public and global health.
If you are coming to LSHTM to study a distance learning programme (PG Cert, PG Dip, MSc or individual modules) starting in 2024, you may be eligible for a 5% discount on your tuition fees.
These fee reduction schemes are available for a limited time only.