There is little research on informal health care providers and their role as sellers of antibiotics. We investigated invisible medicine sellers (IMS) in Cambodia, seeking to better understand the health system gaps they fill, features that allow them to become trusted health providers, and their knowledge of antibiotics. This project is funded by a MRC Joint Health Systems Research Initiative Foundation Grant.
What were our research questions?
1. Which providers do communities in peri-urban Phnom Penh buy medicines from & what influences their choice of provider?
2. Do people buy antibiotics from unlicensed/invisible drug sellers?
3. What drives irrational use of antibiotics by different healthcare providers?
4. What are policymakers’ views on addressing irrational use of antibiotics by private drug sellers?
What is an invisible medicine seller (IMS)?
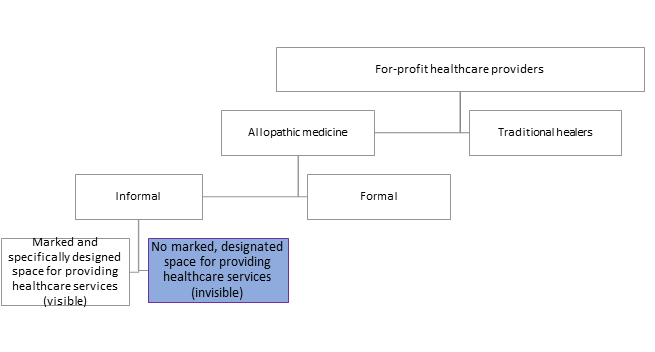
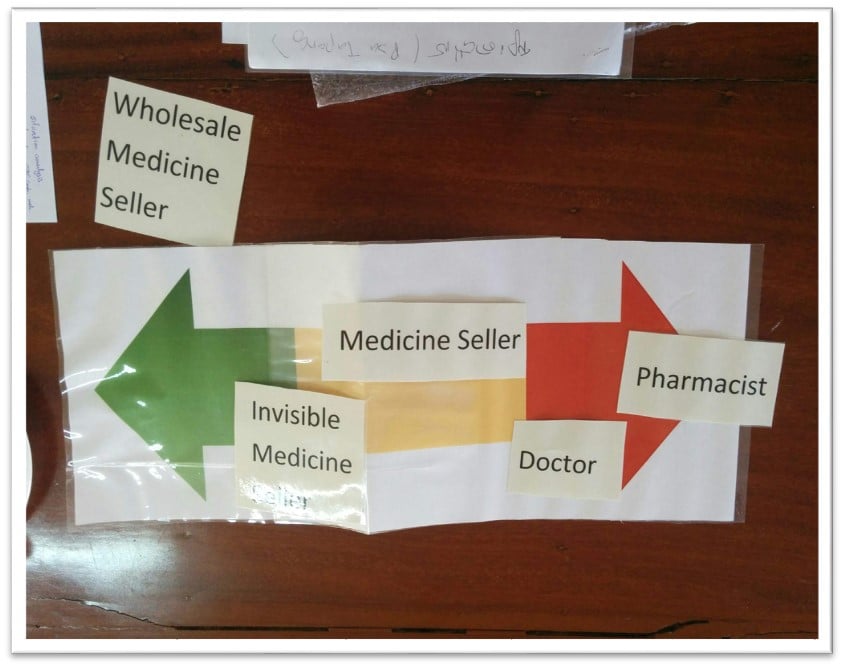
Within the private sector, there are formal and informal providers: visible health care providers (HCPs), who provide health services within in a physical space that is signposted and designed for health services, and invisible HCPs, who provide health services without having a marked and specifically designated outlet for this purpose. We define the latter as IMS.
Why do they matter?
Dispensing of medicines without establishing clinical need poses a risk to patients- and this inappropriate provision of antibiotics is of major global concern due to the scale of morbidity and mortality that is predicted to be caused by antimicrobial resistance (AMR).
Thought there are clear laws in Cambodia surrounding the distribution and dispensation of medicines, antibiotics are often readily available and used without a prescription (and are sometimes counterfeit). This is a major challenge in combating AMR in Cambodia- and across the globe.
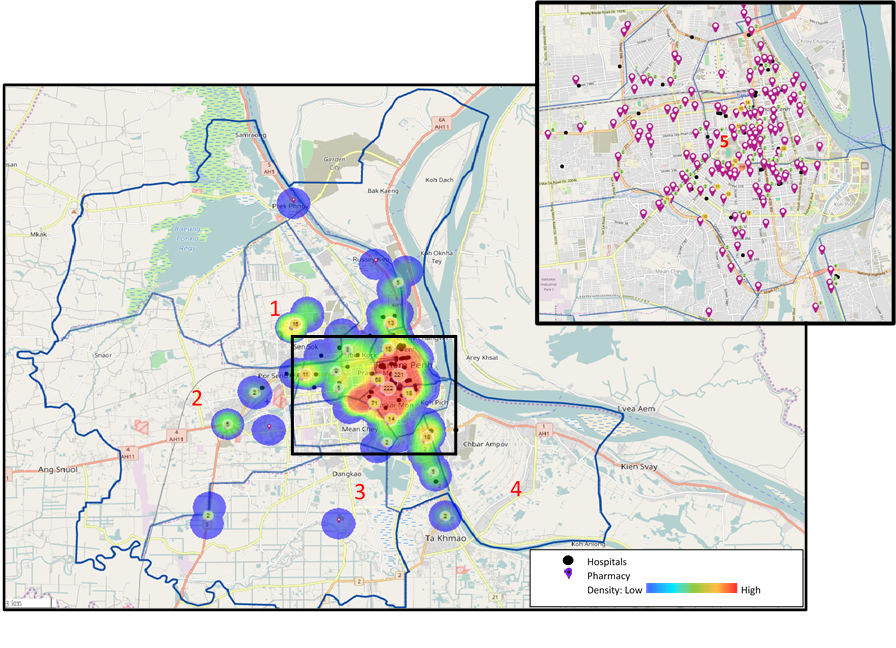
Our work mapping all the registered pharmacies and hospitals across the 12 districts of Phnom Penh reveals stark geographical inequalities in the distribution of pharmacies. The peripheral districts have a much lower density of registered pharmacies and hospitals compared with the central districts. For example, only seven registered pharmacies are located in the Por Senchey district despite this area having a population of approximately 185 000 people; each pharmacy in Por Senchey must serve approximately 26 000 people and cover 23 square kilometres. In contrast, the centrally located district of Prampir Meakkakra has 18 registered pharmacies, with one pharmacy every 0.1 square kilometres.
We are a team of collaborators from the London School of Hygiene & Tropical Medicine, and the University of Health Sciences who share a passion for reducing health inequalities in Cambodia, and across the globe. We bring together an array of diverse skills and experience, across the fields of public health, health systems, pharmacy, and health policy.
Dr. Saphonn Vonthanak
Rector (MD, PhD)
Prof. Vonthanak is the first Cambodian to earn a Ph.D. in epidemiology, and is the rector of the University of Health Sciences in Phnom Penh, Cambodia. This project could not have been done without his great support and expertise.
Dr. Sothavireak Bory
(PharmaD, MSc, PhD)
Sovanthida Suy
( MAppStat, MSc)
Ms. Sovanthida Suy is the head of the Public Health Department at the University of Health Sciences.
Dr. Helena Legido-Quigley
Associate Professor
Prof. Helena Legido-Quigley is an associate professor at the National University of SIngapore's Saw Swee Hock School of Public Health
The ultimate impact of our work will be on populations living in low and middle income countries (LMICs) who will bear the major social and economic consequences of growing antimicrobial resistance (AMR). Inappropriate dispensing of antimicrobial drugs by for-profit healthcare providers in LMICs contributing to AMR is a health systems challenge that is difficult to tackle owing to the number and complexity of stakeholders involved who have conflicting interests, as well as the critical role of how the problem is framed in driving responses.
Conferences and Seminars
We have presented our work at:
2nd Scientific Conference of University of Health Sciences
~ 300 national and international researchers, UHS lecturers and students
(27 to 28 February 2019)
Private Sector Interest Group at the London School of Hygiene and Tropical Medicine
(April 2019)
Media Coverage
Our work was recently covered by the Bureau of Investigative Journalism, as part of their antimicrobial resistance coverage.
Scientific Papers
On September 23, 2019, we conducted a dissemination event at the University of Health Sciences in Phnom Penh. The half-day event was attended by policymakers, policy actors, and university students.
The event was opened by Cambodia's Minister of Health, Mam Bun Heng, who spoke on the importance of AMR, and was chaired by Professor Vonthanak Saphonn. After our team shared our results, there was a panel discussion on AMR and Cambodia, where panelists shared their thoughts, then opened the floor up for questions.
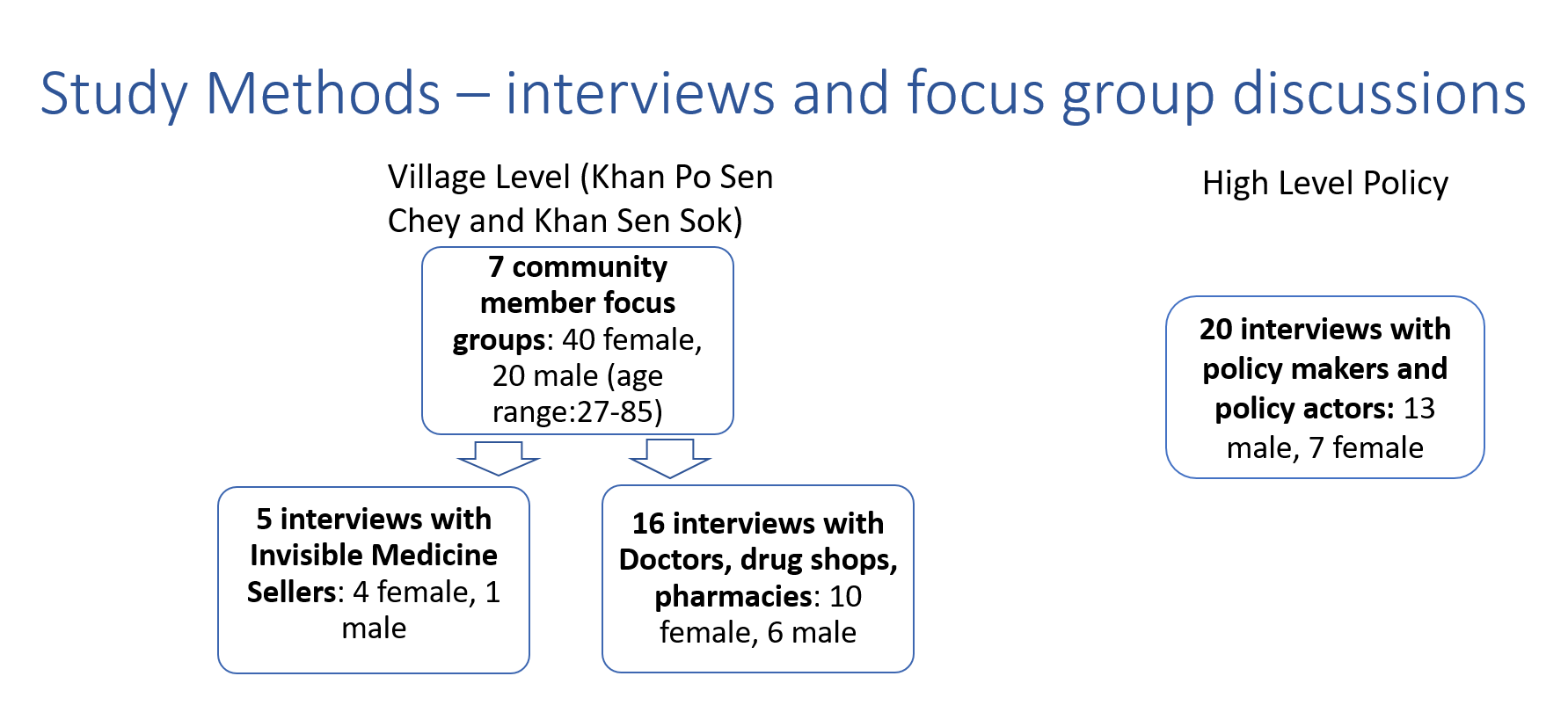
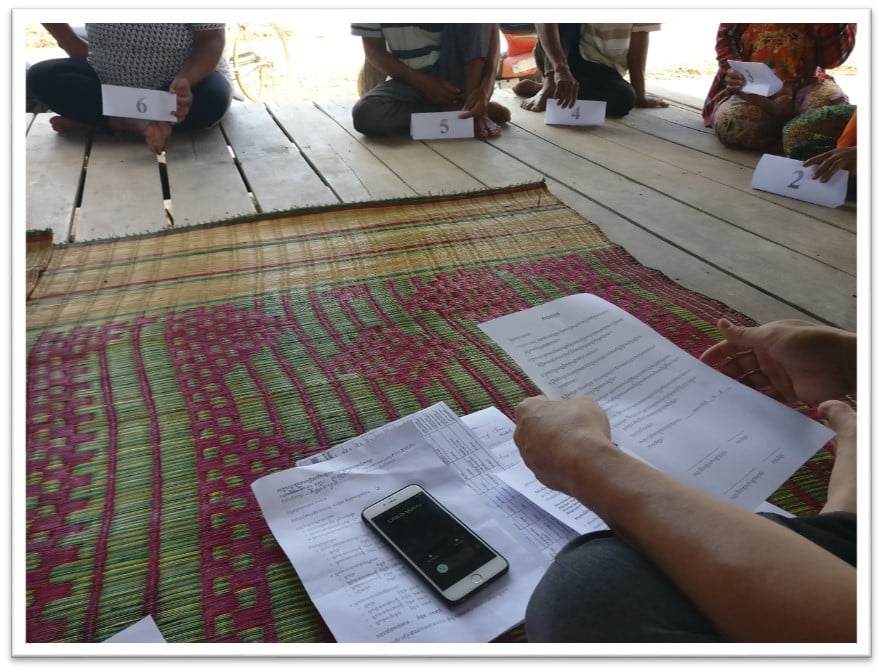
Following a rapid assessment of community healthcare seeking behaviour across two districts, we conducted Focus Group Discussions (FGDs) with community members from 7 selected villages, led by an experienced bilingual facilitator in Khmer.
The research team worked with the village leaders to select participants, aiming for an even distribution of age and sex, and these participants were approached by the village leaders. The FGDs were conducted in an open, centrally located space within each village, typically the main community building in a village, or an outdoor wooden platform used for important meetings. After the discussion, every medicine seller mentioned in the discussion was sought.
We also conducted Interviews with policy makers and policy actors.
The FGDs and interviews were audio-recorded following consent.
Developments and News on AMR in Cambodia and the Southeast Asian Region
Multidisciplinary Fight Against AMR (March 2019)
World antibiotic awareness week in Cambodia: handle food safely and combat AMR (January 2019)
Cambodia joins World Antibiotic Awareness Week Celebrations aiming to prevent misuse of antimicrobials (November 2018)
When “Healing Medicine” Is Bad for Public Health (September 2018)
High antibiotic resistance in Cambodia's pig production (July 2018)
Cambodia’s antibiotic resistance high: study (December 2017)
Ministry bans buying, selling of antibiotics without prescription (November 2017)
Antibiotic Resistance Sparks New Health Policy (February 2015)