World Hypertension Day: Unravelling the Complexity of Hypertension and Shaping a Healthier Future
3 May 2024 London School of Hygiene & Tropical Medicine London School of Hygiene & Tropical Medicine https://lshtm.ac.uk/themes/custom/lshtm/images/lshtm-logo-black.png
What is hypertension?
Hypertension, or high blood pressure, is a condition where blood pressure levels consistently exceed the normal range. Defining hypertension is essential to determine who should receive treatment, yet the threshold for hypertension is often considered debatable. Like BMI, different populations may have different thresholds for hypertension. This includes variations among ethnic groups and individuals with comorbidities like arrhythmia and type 2 diabetes.
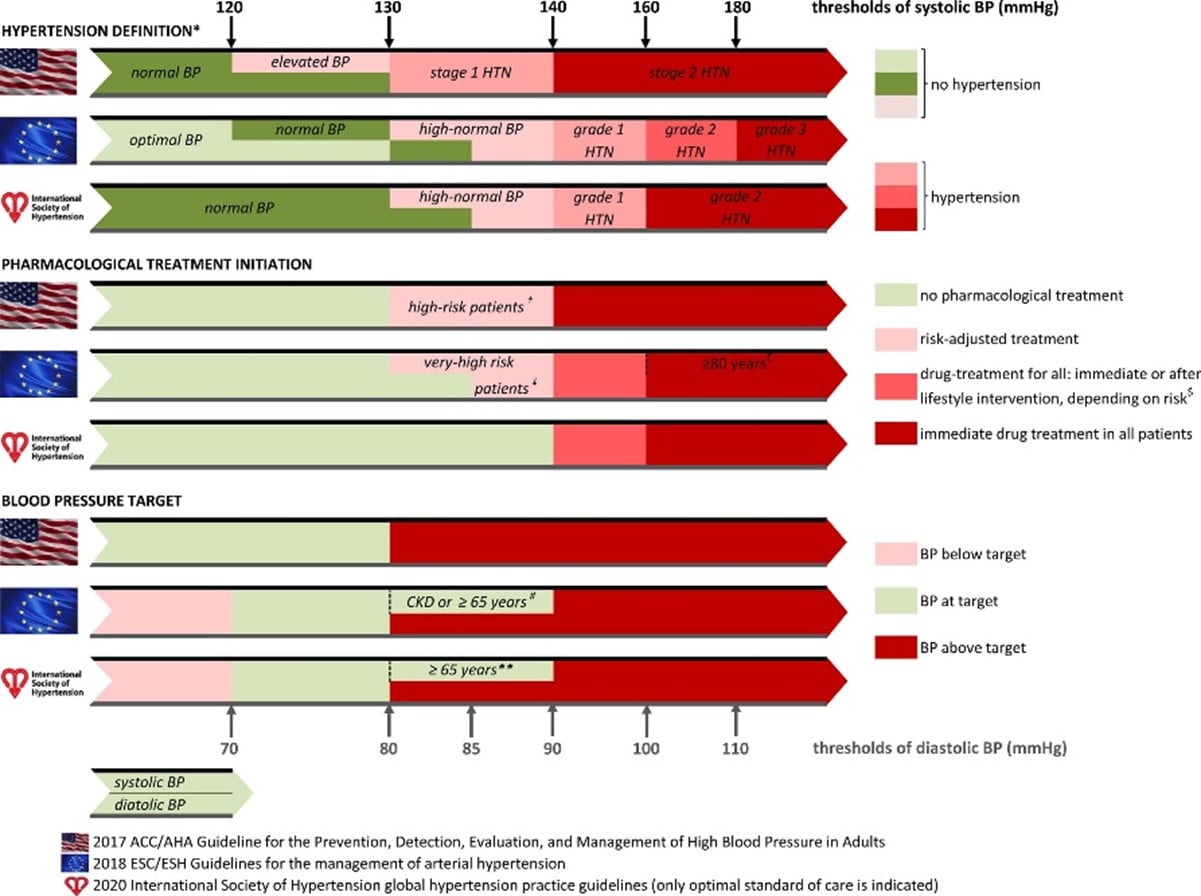
The 2017 American College of Cardiology/American Heart Association (ACC/AHA) guidelines define SBP of 130 to 139 or diastolic BP of 80 to 89 mm Hg defined stage 1 hypertension, whereas any values >140/90 mm Hg defined stage 2 hypertension. The 2018 European Society of Cardiology/European Society of Hypertension (ESC/ESH) guideline maintained the 140/90 mm Hg threshold and hypertension classification from the previous 2013 guideline, whereas the International Scoiety of Hypertension was overall closer to the ESC/ESH than the ACC/AHA guideline.
However, regardless of the threshold for hypertension, there remains a dose-response relationship with cardiovascular risk, even within the normal range. This means that an increase in blood pressure at any range will increase cardiovascular risk. One of the most important trials within the field of hypertension, SPRINT, showed that targeting systolic blood pressure (SBP) <120 mm Hg in patients at high cardiovascular risk resulted in lower rates of cardiovascular events and mortality compared with standard treatment (<140 mm Hg).1 Most studies on hypertension and treatment decisions, such as SPRINT, are based on high-income countries, so applying those findings to regions like sub-Saharan Africa is uncertain. Further research is required to understand the specific risks and optimal management of hypertension in diverse populations globally.
Why do we need to care about hypertension?
Hypertension poses significant dangers to our health, making it a condition that demands attention and care. The consequences of uncontrolled high blood pressure can be severe. Firstly, hypertension puts excessive strain on the blood vessels, leading to their thickening and narrowing, impairing blood flow throughout the body. This can result in serious complications such as heart attacks, strokes, and heart failure. Hypertension also increases the risk of developing kidney disease, as the kidneys are responsible for filtering waste products from the blood. Over time, uncontrolled hypertension can damage the delicate blood vessels in the kidneys, leading to impaired kidney function. Moreover, hypertension is a major risk factor for cardiovascular diseases, including coronary artery disease, peripheral artery disease, and aortic aneurysms. These conditions can have debilitating consequences and significantly reduce the quality of life. By recognizing the dangers of hypertension and taking proactive steps to manage it, we can reduce the risk of these devastating complications and safeguard our long-term health.
Where is HT prevalent?
Hypertension, a global health concern, exhibits varying prevalence rates across different regions. Notably, those of black ethnicity tend to have higher blood pressure levels compared to their Caucasian counterparts beginning in childhood.2–4 Understanding the factors contributing to early hypertension and the disparities between African and Western populations remains a subject of ongoing research.
Among specific populations, there is a growing concern regarding the rise of hypertension among the youth. For example, a study conducted in Zimbabwe highlighted the high prevalence of elevated blood pressure among adolescents, suggesting a potential upward trend in the next five to ten years. This rise in systolic and diastolic hypertension in young individuals is particularly alarming due to its association with future cardiovascular diseases (CVD) and potential of early organ damage in the youth.5 However, existing international guidelines for screening and treatment focus on older adults but overlook the growing evidence that hypertension starts earlier in life and affects youth. More recent evidence emphasizes the need for further research on causes of early onset hypertension, impact on organs in young individuals, and strategies to prevent cardiovascular disease. Urgent attention is required to address whether screening for hypertension should be implemented, what are effective interventions to prevent hypertension among young people and whether the youth should be treated and if so, which treatment regiments are likely to be effective. Additionally, there is a need to establish standardized measurements for borderline high blood pressure and hypertension in adolescents. By addressing these research gaps, we can gain valuable insights into the prevalence, causes, and consequences of hypertension, especially among the younger population, ultimately enabling the development of effective prevention and management strategies.
Holistically preventing hypertension
Individuals can prevent hypertension through the following but not limited ways:
- Maintain a healthy weight.
- Follow a balanced diet, low in sodium and saturated fats.
- Engage in regular exercise.
- Limit alcohol intake.
- Quit smoking.
- Manage stress effectively.
- Monitor blood pressure regularly.
However, preventing hypertension requires strategies that go beyond individual-level determinants, as the condition has a complex and multifactorial etiology. Focusing solely on individual-level factors is unlikely to be sufficient in effectively reducing hypertension at the population level. Urban areas, for instance, face higher rates of hypertension due to factors like combustion and air pollution, which necessitate policy-making decisions to mitigate their effects. Additionally, urban regions often have easier access to ultra-processed foods with high salt content, contributing to hypertension.6,7 Genetic drivers also play a role, with certain ethnic groups and genes having a polygenic association with hypertension. Addressing hypertension requires incorporating these determinants into the health system and collecting data on how these exposures lead to disease states. This information can inform policy decisions and guide government actions, such as regulating food environments and implementing measures similar to those seen in the West with regards to smoking, such as marketing restrictions and bans in public spaces, to reduce exposure to harmful substances. Population-wide approaches are needed, including policies targeting marketing practices and improving access to healthier lifestyle interventions, such as smoking cessation programs, exercise promotion, and weight loss initiatives. Furthermore, considerations around health system capacity, availability of drugs, and affordability for patients must be considered, particularly in regions like Sub-Saharan Africa and Asia. By adopting a comprehensive approach that encompasses individual and societal factors, we can effectively prevent and manage hypertension on a population scale.
What does the future hold?
Future research should prioritize identifying concrete risk factors for hypertension and their impact on public health. This includes investigating the influence of policies and effective government responses to reduce hypertension burden. For example, studying the connection between environmental exposures (e.g., air pollution, unhealthy food environments) and hypertension can inform evidence-based policies. Evaluating population-wide interventions like marketing regulations, public health campaigns, and improved healthcare access is crucial. By generating robust evidence and evaluating policy outcomes, governments can make informed decisions and implement targeted strategies for hypertension prevention and management, leading to better population health.
Written by MSc student Ho Ying Edwina Sze, who is currently studying on the MSc Nutrition for Global Health, with special thanks to Dr Anoop Shah. Dr Anoop Shah is a clinical cardiologist and epidemiologist at the London School of Hygiene & Tropical Medicine and the Imperial College NHS Trust.
References
- Vidal-Petiot E. Thresholds for Hypertension Definition, Treatment Initiation, and Treatment Targets: Recent Guidelines at a Glance. Circulation. 2022;146(11):805-807. doi:10.1161/CIRCULATIONAHA.121.055177
- Suvila K, Lima JAC, Cheng S, Niiranen TJ. Clinical Correlates of Early-Onset Hypertension. Am J Hypertens. 2021;34(9):915. doi:10.1093/AJH/HPAB066
- Justin Thomas S, Booth JN, Dai C, et al. Cumulative incidence of hypertension by 55 years of age in blacks and whites: The cardia study. J Am Heart Assoc. 2018;7(14). doi:10.1161/JAHA.117.007988
- Nkeh-Chungag BN, Stewart S. Review of elevated blood pressure in sub-Saharan Africa. Lancet Glob Health. 2023;11(8):e1148-e1149. doi:10.1016/S2214-109X(23)00283-8
- Sabapathy K, Mwita FC, Dauya E, et al. Prevalence of hypertension and high-normal blood pressure among young adults in Zimbabwe: findings from a large, cross-sectional population-based survey. Lancet Child Adolesc Health. 2024;8(2):101-111. doi:10.1016/S2352-4642(23)00287-0
- Sani RN, Connelly PJ, Toft M, et al. Rural-urban difference in the prevalence of hypertension in West Africa: a systematic review and meta-analysis. Journal of Human Hypertension 2022 38:4. 2022;38(4):352-364. doi:10.1038/S41371-022-00688-8
- Ranzani OT, Kalra A, Di Girolamo C, et al. Urban-rural differences in hypertension prevalence in low-income and middle-income countries, 1990–2020: A systematic review and meta-analysis. PLoS Med. 2022;19(8). doi:10.1371/JOURNAL.PMED.1004079
Our postgraduate taught courses provide health practitioners, clinicians, policy-makers, scientists and recent graduates with a world-class qualification in public and global health.
If you are coming to LSHTM to study a distance learning programme (PG Cert, PG Dip, MSc or individual modules) starting in 2024, you may be eligible for a 5% discount on your tuition fees.
These fee reduction schemes are available for a limited time only.