The Lancet Global Health Commission on Financing for Primary Health Care report is now available, providing evidence-based recommendations for low- and middle-income countries to design their health financing arrangements in ways that place people at the centre and address inequities first.
Research and technical briefs, videos, translations and more from the Commission.
Funder
The Commission
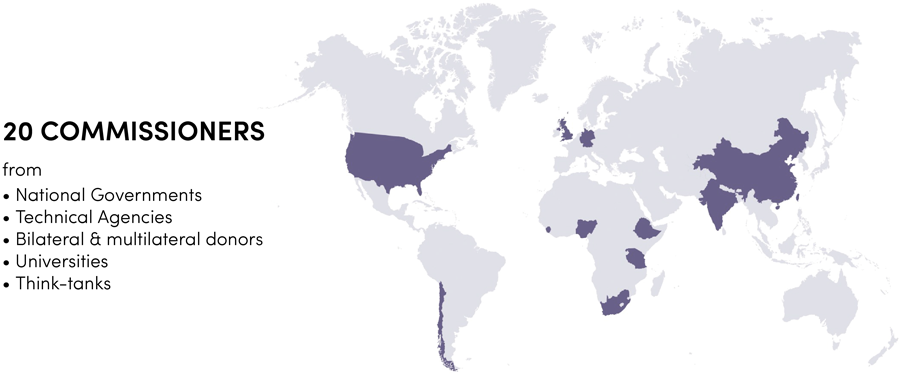
The Lancet Global Health Commission on Financing for Primary Health Care (PHC) convened in April 2020 and met monthly online for over a year. The 22 expert members, representing 19 nationalities, have experience working in national governments, technical agencies, bilateral and multilateral donors, universities, and independent think tanks.
After agreeing on an overall framing for its work, the Commission solicited syntheses of existing evidence and new analyses related to PHC financing in LMICs. Assisted by a technical team of 5 academics based at the London School of Hygiene & Tropical Medicine, its activities and products included:
- Literature reviews, including systematic and scoping reviews, of existing knowledge on financing PHC
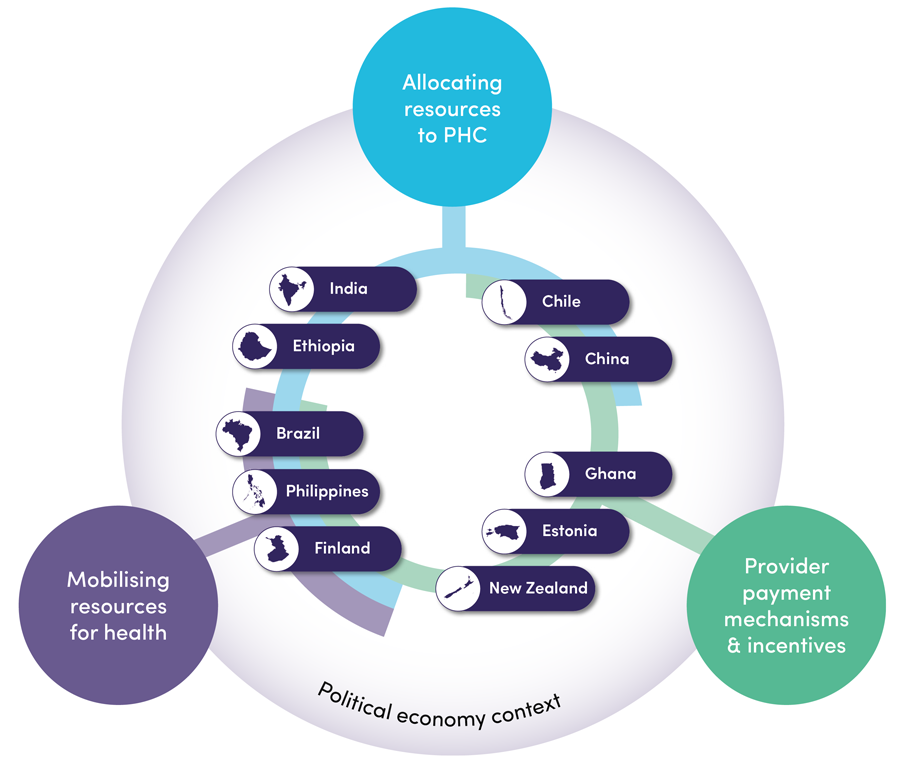
- Case studies prepared by national consultants on innovations in PHC financing in seven LMICs (Brazil, Chile, China, Ethiopia, Ghana, India, Philippines) and three high income countries (Estonia, Finland, New Zealand)
- A survey of PHC organisation and provider payment in LMICs
- Analyses of secondary data on PHC expenditure, using data pooled from the OECD PHC Expenditure Database and WHO Global Health Expenditure Database
- An Expert Roundtable on digital technologies and PHC financing
The report and associated publications were published on 5th April 2022 and are available on the Lancet website.
Aims of the commission
The objectives of the Commission were to identify effective, proven ways of strengthening financing for PHC, and to explore new ideas and approaches.
The Commission has achieved the following:
- Presented new evidence on levels and patterns of global expenditure on PHC, including describing how PHC is currently organised and paid for
- Analysed key technical and political economy challenges faced in financing PHC
- Identified areas of proven or promising practices that effectively support PHC across the key health financing functions
- Identified actionable policies to support LMICs in raising, allocating, and channelling resources in support of the delivery of effective, efficient, and equitable, PHC
Technical team
- Kara Hanson
-
Team leader on the overall project, leading the ‘Revenue mobilisation and allocation’, and ‘Organisation of services’ streams.
Kara is Professor of Health System Economics and Dean of the Faculty of Public Health and Policy at the London School of Hygiene & Tropical Medicine (LSHTM). She has worked in a range of settings in sub-Saharan Africa and Asia, since her first job, which was as ODI Fellow in the Ministry of Health, Swaziland, in 1988. Kara did a doctorate at the Harvard School of Public Health and joined LSHTM in 1997. She is interested in the role of the private sector in health systems, and in identifying the opportunities and limitations of the private sector in improving the efficiency, quality and responsiveness of health systems. This includes a particular interest in novel approaches to regulation, particularly in relation to market disruptions such as provider consolidation and e-pharmacy. Amongst many other areas, Kara also works on health financing reforms, particularly the way that strategic purchasing can help to improve health system outcomes.
- Dina Balabanova
-
Dr Dina Balabanova leads the ‘Foundation’ stream.
Dina is an Associate Professor in Health Systems and Policy in the Department of Global Health and Development at the London School of Hygiene & Tropical Medicine (LSHTM), with over 20 years of experience in health systems and policy research across a range of low and middle income countries (LMICs). She currently leads a research portfolio on anti-corruption (SOAS-ACE and others).She co-leads research on barriers to hypertension control among poor populations in Malaysia and the Philippines (RESPOND) using surveys and a digital diary platform, building on previous work on diabetes. She was a Health Systems Global board member (2012-18) and is a Section Editor for the BMC Health Services Research for LMICs. She has developed and runs the LSHTM Health Systems taught modules. Dina has mentored, and is engaging with, a broad network of researchers, policy makers and practitioners worldwide to support effective health systems development.
- Timothy Powell-Jackson
-
Timothy Powell-Jackson leads the ‘Incentives stream’.
Tim is an Associate Professor in Health Economics in the Department of Global Health and Development at the London School of Hygiene & Tropical Medicine (LSHTM) and a member of the Centre for Health Economics in London (CHIL). He has 15 years of research experience working in low and middle income countries (LMICs), applying empirical methods to better understand how health systems function and how they can improved. Tim first developed an interest in health economics while working at the Ministry of Health, Rwanda, on a two-year placement with the Overseas Development Institute Fellowship Scheme. He did a doctorate at LSHTM, spending two years in Nepal carrying out research as part of a UK government funded project.. His work on topics ranging from health financing and provider payment reforms to management practices and the private sector have been published in medical journals as well as health and development economics journals. He currently works on projects in Brazil, Tanzania, and Malawi, all of which have a strong focus on quality of care.
- Nouria Brikci
-
Nouria Brikci is a research fellow on this project.
Nouria holds a MSc in Development Studies at SOAS and a MSc in Health Policy, Planning and Financing at LSHTM/ LSE. Nouria has over 17 years’ experience working as a health financing and health policy specialist across Africa and Asia. Amongst other roles, she was team leader and lead consultant on the development and implementation of health financing strategies in Sierra Leone, Ethiopia, Swaziland and Morocco; fiscal space analysis for Universal Health Care (UHC) in Togo, Ethiopia, Morocco, DRC and Cameroon; evaluations of financing approaches such as the Free Health Care Initiative in Sierra Leone or Community Based Health Insurance (CBHI) in Burkina Faso and Rwanda, and has supported the Global Financing Facility as team leader across 7 western African countries. Nouria was previously a senior consultant and Health Portfolio leader at Oxford Policy Management (OPM), a senior health policy adviser at Save the Children UK, and a research adviser for Médecins Sans Frontieres (MSF UK).
- Darius Erlangga
-
Darius Erlangga is a research fellow on this project.
After working as a general practitioner for two years in Indonesia, he took an interest in the economics aspect of medicine. He holds a Master’s in Public Health and in Health Economics from Tulane University and a PhD in Health Sciences from the University of York. His thesis evaluated the impact of an expanded national health insurance programme in Indonesia, focusing on three outcomes: access to health care, financial protection, and health status. He previously worked as a research fellow at the University of Warwick to develop a health economics model for emergency transportation in low and middle income countries. His research interests cover health financing in developing countries, impact evaluation studies using randomised or non-randomised study design, systematic/scoping review to address non-interventional health topics, and economic evaluation of public health programmes.
- Brigid Strachan
-
Brigid Strachan is Commission Manager of this project
Brigid has diverse academic training in African Area Studies (MA, SOAS), human resource development and affirmative action (PhD from Open University); health policy planning and financing (MSc LSHTM) and organisational management & leadership (PG Dip in Organisational Leadership Said Business School University of Oxford). Brigid worked first as an academic, then as a consultant with her own company in South Africa, Impact Health Management Solutions. The areas Brigid has worked in as a consultant and project manager are health policy, health care financing and Human Resources for Health. She has also worked on the development of postgraduate programmes in management and leadership development for the University of Cape Town, the University of Stellenbosh and the National Department of Health South Africa.
- Ellen Nolte
-
Dr Ellen Nolte, Professor of Health Services and Systems Research at the London School of Hygiene & Tropical Medicine.
Ellen holds a PhD from London University and a Masters degree in public health (MPH). Her expertise is in health systems research, international health care comparisons and performance assessment. Over the past decade she has developed an internationally recognised research portfolio around innovative service models that seek to better meet the needs of people with complex and long-term health problems, with a particular focus on care coordination and integration within and across sectors. She is co-Editor-in-Chief of the Journal of Health Services Research & Policy. Ellen was previously head of London Hubs of the European Observatory on Health Systems and Policies and Director of the Health and Healthcare Policy programme at RAND Europe, Cambridge, UK. Ellen brings expertise on primary care systems across European countries.
- Haja Ramatulai Wurie
-
Dr Haja Ramatulai Wurie, College of Medicine and Allied Health Sciences (COMAHS) at the University of Sierra Leone (USL).
Dr Wurie is the Dean of the Faculty of Nursing and a Senior Lecturer in Biochemistry at COMAHS, and is involved in health systems research and capacity strengthening within Sierra Leone to deliver credible, relevant research for effective policy making and practice. She has conducted research on a number of health systems issues, in line with the national needs in Sierra Leone, generating evidence to inform government policy and donor strategies for building resilient and responsive health systems, thereby achieving universal health coverage for all. She also provided technical assistance to the health systems strengthening process in Sierra Leone post Ebola, working with the in-country and international teams on the development of the health sector recovery plan.
- Manuela De Allegri
-
Professor Manuela De Allegri, Leader of Research Unit Health Economics and Health Financing at the Heidelberg Institute of Global Health.
Manuela has a diverse academic training in Sociology, Health Economics, and Public Health. She joined the Heidelberg Institute of Global Health at the University of Heidelberg in 2002. She first took the lead of the Research Group in Health Economics and Financing in 2011, as Junior Group Leader (assistant professor equivalent), being promoted to Privat Dozent in 2014 (associate professor equivalent) and to Professor in 2019. Her areas of expertise include health financing, impact and process evaluation, and economic evaluation, with specific application to social health protection and provider payment mechanisms in low-and middle-income countries. Manuela brings to the team content-specific expertise in health financing and health system strengthening, having worked on a wide range of reforms across health financing functions, resource mobilization, pooling, and purchasing. She is particularly interested in understanding how resource allocation can be redirected, through organizational restructuring that carefully moderates incentives built within the health system, to maximize societal benefits, measured both in terms of improved efficiency and equity in access to service use.
- David Hipgrave
-
Dr David Hipgrave, Section Chief, Health and Nutrition at UNICEF Iraq.
David is an Australian paediatrician and global child health specialist with extensive country-level experience based on 25 years working in Africa and south and east Asia. David joined UNICEF Indonesia in October 2004 and managed its health and nutrition responses during several major natural disasters, a polio outbreak and many community-level maternal and child health and nutrition programs. From 2007 - 2011, David led UNICEF’s broad support for child public health in over 70 counties, and also worked closely with the Chinese national government on its health system reforms and maternal and child health and nutrition improvements. Now based at UNICEF’s New York Headquarters, David leads the team focusing on health systems strengthening and primary health care. David was a Commissioner on the recent Lancet Commission: A future for the world’s children.
- David Morgan
-
David Morgan, Head of Health Accounts/Senior Health Policy Analyst, OECD.
David has worked in the Health Division of the Directorate for Employment, Labour and Social Affairs for more than eighteen years. He has been Head of Health Accounts since 2011 and in recent years has had overall responsibility for OECD Health Statistics and the OECD Working Party on Health Statistics, governing statistical activities and data collection in the OECD relating to health and health systems. His focus has been in the development of global frameworks and standards, particularly in the domain of health financing and expenditure information. Since 2006, he was part of the international team of experts responsible for A System of Health Accounts, a book released in 2011. During his time in the OECD Health Division, he has led a number of studies and projects, in the areas of Expenditure by Disease, Age and Gender, Trade in Health Services and Health and Long-term Care Expenditure Forecasting, as well as a number of country studies. In recent years, he has been part of a team working with national and international experts to develop a methodology to produce comparable estimates of spending on Primary Health Care, which are now published on an annual basis for OECD countries.
- Rajeev Sadanandan
-
Rajeev Sadanandan, CEO of Health System Transformation Platform.
Rajeev is the ICMR Chair for Health Systems Research in the Department of Health Research, Ministry of Health and Family Welfare, Government of India. He is CEO of Health System Transformation System, a not-for-profit company engaged in Health Systems Research. Prior to this he was a member of the Indian Administrative Service. As health secretary of Kerala state, he initiated transformation of the health system in the state with a focus on primary care. He was the CEO of Rashtriy Swasthya Bima Yojana (RSBY), India’s national social health programme. Rajeev had been involved in developing and managing the TB control and HIV/AIDS programme at the national and state level. He worked for a brief stint in UNAIDS and has been a member of technical committees set up by UNAIDS and WHO.
- Hong Wang
-
Dr. Hong Wang, Senior Program Officer at the Bill & Melinda Gates Foundation.
Hong has over 30 years of experience in health policy, with a focus on health economics, financing, and systems in developing countries. His responsibilities include taking leading intellectual and implementation roles in the formulation of the Gates Foundation position on the critical issues in health economics, financing, and systems, particularly related to primary health care development. He serves as an in-house expert and manages a grant portfolio focused on improving primary health care globally, including understanding how financial resources are mobilized, allocated, and spent in primary health care. Hong also holds a position of Affiliate Professor at the Department of Global Health, University of Washington. Before joining the Bill & Melinda Gates Foundation, he was an Assistant and a Clinical Associate Professor in the Global Health Division at Yale School of Public Health, an Associate Professor and Acting Director in the Health Economics Department at Beijing Medical University, China, and an Adjunct Professor and Deputy Director at National Health Economics Institute of Ministry of Health, China.
- Chima Ariel Onoka
-
Professor Chima Ariel Onoka, Community Physician and Health Systems Economist, University of Nigera Nsukka.
Chima is a fellow of the West African College of Physicians and holds a Ph.D. in Health Economics from the University of London. He has previously served as honorary consultant public health physician at the University of Nigeria Teaching Hospital. At the University of Nigeria, he has also served as associate dean of the faculty of medicine, pioneer associate director of the Institute of Public Health, and head of operations of the Health Policy Research Group. He has worked as a consultant to the Federal Ministry of Health, USAID, PATHS2 (Abt Associates) and Health Reform Foundation of Nigeria (HERFON). His research has focused on the policies and economics of universal health coverage initiatives in Nigeria, the role of public and private sector in health financing including the National Health Insurance Scheme (NHIS) and health maintenance organisations, as well as the systems for providing maternal and child health, HIV/AIDS and malaria services. He was a member of the secretariat for the National Council on Health for several years.He has also supported the Government of Nigeria by serving at the National Primary Health Care Development Agency of Nigeria as a Senior Technical Advisor on Primary Health Care Systems strengthening.
- Gemini Joseph Mtei
-
Dr. Gemini Joseph Mtei, Senior Director, Public Finance Systems under public sector Systems Strengthening Plus (PS3+) Project.
The PS3+ project is funded by the United States Agency for International Development and implemented by the Abt Associate Inc. Gemini is coordinating the implementation of interventions to strengthen cross-sector public financing systems including improving strategic purchasing, budgeting, planning and financial management to improve service delivery. Prior to this he worked with the Ifakara Health Institute as a researcher for over 10 years in the field of health care financing and social protection, including assessment of equity in financing and access to health care services, health insurance regulations, and financial risk protection.
- Christoph Kurowski
-
Christoph Kurowski, Global Lead for Health Financing at the World Bank Group.
Christoph has advised governments at all stages of development in the design and implementation of health financing and health system reforms. He spearheaded and co-led global health initiatives, among others, the Annual Health Financing Forum, the UHC Financing Initiative of the G20 Finance and Central Bank Track, the IMF/WB joint health financing program and the Global Financing Facility for Every Woman and Every Child. His current research interests include the resilience and sustainability of health financing and the use of technology and behavioural science to expand financial protection to low-income households. Prior to his career in international finance and development, Christoph gained hands-on experience in the delivery of health services working as a paediatrician for Doctors without Borders as well as at the Children’s Hospital of the University of Cologne/Germany.
- Cheryl Cashin
-
Cheryl Cashin, Managing Director, Results for Development in the global health practice.
Cheryl co-leads a portfolio of more than 20 projects and initiatives in global health systems, and she serves on Results for Development’s (R4D) executive team. She is a health economist specializing in the design, implementation and evaluation of health financing policy in low- and middle-income countries, with a particular focus on health purchasing and provider payment for universal health coverage (UHC). She has led several initiatives at R4D that aim to build new models of support for countries to address complex health system issues. She is a regular on the faculty of WHO’s Advanced Course on Health Financing for UHC and the World Bank’s Flagship Course on Health System Strengthening. She has held academic positions at Boston University’s School of Public Health and University of California, Berkeley’s Nicholas C. Petris Center on Health Care Markets and Consumer Welfare. She is the lead author of the books Paying for Performance in Health Care Implications for Health System Performance and Accountability and Health Financing: The Macroeconomic, Fiscal, and Public Finance Context.
- Karin Stenberg
-
Karin Stenberg, Health Economist, World Health Organization.
Karin’s areas of expertise include the development and application of methods and tools in the areas of costing, economic evaluation, technical efficiency and health systems strengthening for the United Nations’ Sustainable Development Goals (SDG). She has supported multiple global cost and impact projection analyses, including assessments of global investment needs for the health SDG targets and the relevant primary health care components. She is a member of the UN inter-agency working group that oversees the development of the OneHealth Tool for supporting country strategic health planning. She graduated from Lund University, Sweden, with a master’s degree in economics.
- Abebe Alebachew Asfaw
-
Abebe Alebachew Asfaw, Principal Partner of Breakthrough International Consult (BIC) PLC.
Abebe and has Master’s degree (M.Sc.) in Human Resource Economics (health, education and labor economics). Abebe has thirty-four years of working experience in health strategic planning and policy, health financing reforms and aid architectures. He was involved in the development of social sector policies, strategies, norms and standards, especially in the health sector when he was working in the Ministry of Economic Development and Cooperation (MEDAC). He was part of the team that initiated the health financing reform in Ethiopia) in the mid-90s which is still being implemented. He worked as a health system advisor in Kenya for five years which culminated in the development of an essential services package, development and implementation of sector-wide approach. He has led a number of long and short-term assignments for the last 13 years, most of them related to health financing, health system strengthening and governance. Together with the Harvard school of public health, he reviewed the health care financing strategy implementation, estimated the cost of primary health care provision in general and exempted services in particular, and estimated the potential sources of additional government financing. He also assisted in the revision of health financing strategy in Ethiopia with the vision of Universal Health Care. He has experience in undertaking efficiency and value for money analysis and has expertise in fiscal space analysis and the role of fiscal transfers in service delivery in the context of low income and desterilized context.
- Ina R. Kalisa
-
Ina R. Kalisa, Health Economist consultant at the WHO Rwanda Office.
Ina previously served as a WHO technical advisor to the community-based health insurance scheme at the Rwanda Social Security Board. She has also worked as a Lecturer and Head of Department of Health Policy, Economics and Management at the School of Public Health/University of Rwanda. She has several years of teaching and research experience in public health and health financing. Her professional interests include health financing, equity in health and health care, public health policy and health services costing. Ina is a medical doctor and has a master’s degree in Public Health majoring in Health Policy and Management from the Université Libre de Bruxelles.
- Mark Blecher
-
Dr. Mark Blecher, Chief Director, Health and Social Development, National Treasury of South Africa.
Mark has over 50 publications in the field of public health and health economics in a range of books and journals including the South African Medical Journal, SA Health Review, Vaccine, OECD book and others. His academic qualifications include a four year specialist degree in Community/Public Health at University of Cape Town and a PhD in an area of health economics. He supervises a team of ten in the National Treasury and has previously worked in Policy and Planning and Health Economics in the public sector. His work encompasses many areas including National Health Insurance research and development, putting in place health conditional grants like the HIV/AIDS grant, heading Health and Social Protection Function Committees which make recommendations on sectoral budget allocations. His section of the Treasury also works on social grant modelling and budgeting, ECD and other aspects of Health and Social Development. He has also worked on aspects of social security development. Dr. Blecher was co-chair of UNAIDS Economic Reference Group and works regularly with various global organisations such as WHO, GAVI, Global Fund, GFF and others. He is currently co-authoring several international cross-country studies on UHC.
- Alexo Esperato
-
Alexo Esperato, Senior Program Officer,Health Systems Design at the Bill & Melinda Gates Foundation.
Alexo’s experience spans healthcare delivery and financing. Currently in India, he is leading various technical assistance initiatives that focus on health insurance, primary care and health technology assessment. Prior to India, Alexo consulted with the World Bank on primary care and care integration in Costa Rica, Paraguay, Mexico and Jordan. He also provided technical advice to Bahrain’s government on health insurance, and worked on health financing in Haiti. Previously, Alexo had worked at the World Health Organization, where he managed quality of healthcare programs across Latin America and the Caribbean. Alexo has been also involved in various analytical studies, including economic and impact evaluations of health interventions. Prior to joining the Gates Foundation, Alexo obtained his PhD in health systems from Johns Hopkins University, and trained in economics, public policy and management.
- Jeanette Vega Morales
-
Dr Jeanette Vega Morales, Minister of Social Development and Family in Chile.
Jeanette is the Chief Medical and Innovation Officer at Red de Salud UC-Christus, the main private health provider in Chile. She holds MD from the Universidad de Chile and a PhD in Public Health from the University of Illinois at Chicago and has over 20 years of experience in international health. Her areas of expertise include social determinants of health, health equity, and health systems. She served in the World Health Organisation between 2003 and 2007 as Director of the Equity and Social Determinants of Health. She served as Vice-Minister of Health in Chile between 2008 and 2010 as part of President Bachelet´s first term. Between 2012 and 2014, she was the Managing Director of Health at the Rockefeller Foundation. She resigned to join President´s Bachelet second term team as Director of the National Health Fund. In March 2018, she joined Red de Salud UC CHRISTUS as Chief Medical Innovation and Digital Transformation Officer. Over the years, she has collaborated in several international advisory committees and boards, and with multiple international and national health organisations. In February 2022 Jeanette was appointed Minister for Social Development in Chile.
- Qingyue Meng
-
Professor Qingyue Meng, Professor in Health Economics and Policy, Dean of Peking University School of Public Health, and Executive Director of Peking University China Center for Health Development Studies.
Before taking his current position, Qingyue was the Dean of Shandong University School of Public Health and Director of Shandong University Center for Health Management and Policy. His research interests include health financing policy. He has led a team doing dozens of research projects supported by both domestic and international funding sources. He has been Member of the Expert Committee on Health Policy to China National Health Commission. He is the founding Board Member of Health Systems Global elected from the Asia and Pacific Region. Qingyue holds his degree in medicine from Shandong Medical University (now Shandong University), a master’s degree in public health from Shanghai Medical University (now Fudan University), a master’s degree in economics from University of the Philippines, and a PhD in health economics and policy from Karolinska Institute in Sweden.
- Martin Roland
-
Professor Martin Roland, Emeritus Professor of Health Services Research at the University of Cambridge.
Martin qualified as a doctor at Oxford University in 1975, then trained as a general practitioner. He was appointed as Professor of General Practice at the University of Manchester in 1992 where he was Director of the National Primary Care Research and Development Centre from 1994 to 2009. In 2009 he moved to Cambridge to the inaugural Chair in Health Services Research which he held until 2016. Professor Roland’s research focuses on developing ways of measuring and improving the quality of primary medical care including evaluation of pay for performance schemes. His previous areas of research include back pain, specialist referrals, out of hours care, and nurse practitioners in primary care.
A frequent contributor to health policy debates in the UK and abroad, in 2015 Professor Roland chaired a commission for the NHS in England which produced the report ‘The Future of Primary Care: Creating Teams for Tomorrow” which included recommendations for an expanded multi-disciplinary primary care workforce, expansion of GP federations and networks to enable general practice to operate at larger scale, closer relationships with specialists, and expanded IT links between primary care, community care and specialists. These were largely taken up in NHS England’s 2016 ‘General Practice Forward View’. He was a member of the Commonwealth Fund of New York’s Expert Working Group on developing health systems to meet the needs of patients with complex conditions. He is an International Member of the National Academy of Medicine.
- Brazil
- Chile
- China
- Estonia
- Ethiopia
- Finland
- Ghana
- India
- New Zealand
- Philippines
Overarching brief
Technical brief 1 - Mobilising and pooling funds for primary health care
Technical brief 2 - Allocating resources to primary health care
Technical brief 3 - Getting incentives right for primary health care
Technical brief 4 - Harnessing the political economy factors at the core of primary health care financing
Ethiopia policy dialogue
LSHTM worked with the Ministry of Health and Ethiopian Health Insurance Services (EHIS) to translate the findings of the Lancet Commission into Ethiopia specific policy recommendations. Read the briefings produced for this dialogue. View the presentation summarizing the discussions.
Review of the role of digital technology for health financing
LSHTM undertook a systematic review of the literature investigating the impact of digital technology on health financing. Read the working paper.
Film for launch of Lancet report: Overview of the Commission and presentation of results
The Lancet Global Health Commission on Financing Primary Health Care is excited to be featured at this year’s Annual Health Financing Forum. The event, organised by the World Bank, USAID and the Global Financing Facility, aims to convene key actors from the health and financing sectors to discuss pressing health financing concerns.
This year's Forum will focus on approaches to mobilizing and pooling funds to pay for primary health care. Despite more than 50 years of global attention to PHC, the COVID-19 pandemic has revealed how health systems in many low- and middle-income countries remain focused on delivering secondary and tertiary care. Frequently, only limited health services and medicines are available at the first point of contact, often of poor quality and requiring considerable out-of-pocket costs. The result is that many people choose to bypass this care altogether. In response to the COVID-19 pandemic, countries may also have invested more in tertiary care with the sudden need for increased intensive care to the detriment of PHC.
The forum will be hosted in Washington, DC and online. Six plenary sessions will explore opportunities at the boundaries, that is, areas where the way forward remains controversial or unclear. The Forum will build on the work of the Lancet Commission on Financing Primary Health Care and feature Professor Kara Hanson as a speaker during its introductory session.
Find out more information.
The People’s Health Movement have provided some commentary on the report of The Lancet Global Health Commission on Financing for Primary Health Care. Our response is below:
"The Lancet Global Health Commission on Financing PHC does not take a pro-private sector position. In the report we assert the need for greater public funding of PHC, with specific recommendations on how these funds can be mobilised and allocated through the public finance system. We also recognise the political challenges of raising money for health and PHC through taxes.
"Our primary focus is on how to make financing arrangements work better for public providers as we recognise the public sector is key for inclusive PHC. In examining how to strengthen PHC financing, we identify a number of policy levers to increase allocation of public budgets, and changes to how providers are paid - all of which are directed at spending resources better in the public sector. We cannot ignore the presence of the private sector in providing PHC and the enormous role it continues to play in some countries. In some settings it may be possible to channel public funds to private providers (as in the UK, for example). But we argue in the report that in low income settings without capacity to manage effective strategic purchasing the priority should be to invest in the provision of good quality and affordable services in the public sector.
"The central role of people and communities is present in the notion of the community platform through which essential services and public health functions are enabled and shaped, as envisaged in the Astana declaration. However, we found little evidence specifically on financing of the community components of PHC. More evidence is needed on how countries can reduce their dependence on external financing for their community health systems, on what budget practices can direct and protect resources destined to community level providers, and on how best to pay CHWs in ways recognise their critical inputs.
"The role of social struggles and political movements are an integral part of the Commission report. Our core political argument is that equitable and inclusive PHC financing reform are often driven by grassroots social movements representing a broad range of often poor and marginalised groups (as in Brazil and Costa Rica). The mechanisms through which this contestation is resolved and entitlements claimed is achieved though specific social contracts or through the right to essential PHC enshrined in Constitutions. This analysis informed the key message that achieving effective and equitable people-centred PHC requires recognising the politics (power, representation, and societal movements) that shape what is possible within each country context."
On 24 May 2022 at 12:00 BST, the Lancet Global Health Commission on Financing PHC will be participating in a webinar organised by the Overseas Development Institute (ODI).
The event will discuss the overall findings of the commission and explore the country case-studies we drew on, exploring two key themes: how budget and public finance systems can support the vision of PHC the commission outlined, and how PHC financing functions in multi-level systems of governance.
Speakers:
- Eugenia Amporfu, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana
- Kara Hanson, LSHTM, UK
- Tom Hart, ODI, UK
- Leizel Lagrada-Rombaua, GECC Development Services, Pasic City, Phillipines
- Adriano Massuda, Getulio Vargas Foundation, Rio de Janeiro, Brazil
- Fiona Samuels, ODI, UK
Find out more information and register.
Find the recent research and technical briefs from the Commission on our Resources page.