Got your underwear, bed sheets and vaccination? Why freshers could help eliminate measles
London School of Hygiene & Tropical Medicine https://lshtm.ac.uk/themes/custom/lshtm/images/lshtm-logo-black.png Wednesday 21 September 2016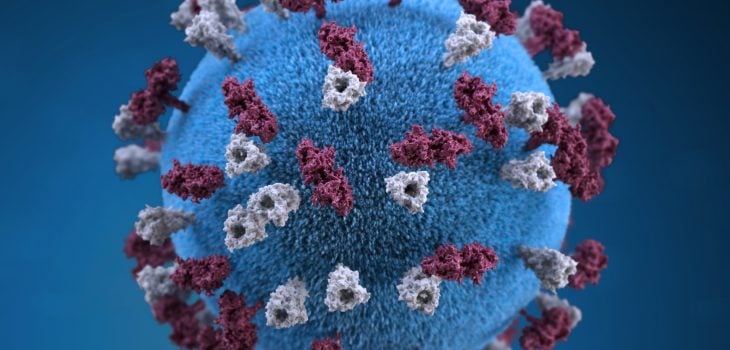
It’s the time of year when hundreds of thousands of teenagers are beginning an exciting new chapter in their lives. Freshers’ week will see friendships fostered for life, but for some unfortunate students it will also mean experiencing something not quite as welcome. Close contact between large groups of young adults is the perfect breeding ground for infectious disease. Perhaps surprisingly, measles is one of them.
Fifty years ago measles affected virtually every child in the world. In the UK alone this resulted in hundreds of thousands of cases and hundreds of deaths every year – even today about one in 2000 reported measles cases results in a death.
The US introduced measles vaccination in the mid 1960s – almost certainly one of the most effective and cost-effective medical interventions of all time. European countries followed shortly afterwards – Russia in 1967, the UK in 1968 and the Netherlands in 1976.
Although spectacular declines in measles incidence followed, the disease remained endemic in most countries with epidemics occurring every few years. This was because countries were offering just a single dose of measles vaccine – about 90% of children vaccinated will become immune so even if vaccine coverage is 100% then this still leaves 10% unprotected allowing measles to circulate among ‘susceptibles’.
The introduction of the triple-jab measles, mumps and rubella vaccine (MMR) and the second dose early in childhood, which occurred in the 1980s and early 1990s led to increases in vaccine coverage and further declines in measles incidence. By the mid 1990s, measles was becoming very rare and elimination of the disease (along with rubella) became a very real possibility…but then the spectacular gains started to unravel.
Almost 20 years ago a little-known gastroenterologist called Andrew Wakefield published a paper claiming a link between the MMR jab and autism. Although the scientific basis for this claim was almost non-existent he began an increasingly embattled campaign against the vaccine which became front page news. The result? Parents and even some health-care professionals became confused about the risks and hesitant about vaccinating their children and coverage rates dropped. In England MMR coverage at two years of age fell to 80% by 2003, and was 10% lower still in London.
Measles did not immediately bounce back. This was largely because a successful campaign had been conducted just prior to the controversy in which school aged children were offered the measles-rubella (MR) vaccine.
Gradually, carefully conducted studies were published that failed to show a link between autism and MMR (the best that scientists can do, as you can’t prove a negative). The tide slowly turned but the controversy left its mark. It was not until 2010 that MMR coverage in England exceeded 90%. Confidence is easily lost, but it takes a long time to regain.
Over the last 10 years measles has gradually crept back into our society. Outbreaks have been occurring in groups which are more difficult to reach and spilling over into wider society – particularly in areas with lower levels of coverage, such as London.
The disease has started to catch up with the ‘Wakefield cohorts’ who are now in their teens, mopping up susceptibles in other age groups as it goes. A disease that was typically spread in nurseries and schools is now one that hops between summer festivals and freshers’ fairs.
So what will happen in the future? Are we content to allow this virus that can cause pneumonia, brain inflammation, deafness and occasionally death to linger in our society? Two doses of vaccine can prevent it but the epidemiology has changed. It is no longer sufficient to just vaccinate in early childhood. If we want to eliminate the disease we also have to reach the other susceptible groups. Increasingly this also includes adults but they, particularly young men, tend to have much less contact with the health services.
So what can we do? The first and most important thing is to maintain very high levels of two-dose coverage in infants and young children. This will get tougher as the incidence of measles will go down – we need to anticipate and prepare for this. Monitoring mothers’ attitudes to immunisation programmes, and research into what influences their decisions, will be critical.
We also need to be more creative about reaching older unvaccinated individuals. At every major life event – primary school, secondary school and college – parents should ask themselves if their child is fully protected against not just measles but other infectious diseases too.
And as for new university students – well ensuring you are vaccinated is as important as bringing enough underpants.
The next steps in the fight against measles and rubella in Europe were the subject of a special event hosted by The London School of Hygiene & Tropical Medicine and the World Health Organization on 20 September 2016.
Image: 3D representation of measles virus particle studded with glycoprotein tubercles. Credit: CDC/Allison M. Mauri & Alissa Eckert
Our postgraduate taught courses provide health practitioners, clinicians, policy-makers, scientists and recent graduates with a world-class qualification in public and global health.
If you are coming to LSHTM to study a distance learning programme (PG Cert, PG Dip, MSc or individual modules) starting in 2024, you may be eligible for a 5% discount on your tuition fees.
These fee reduction schemes are available for a limited time only.