HIV patients showing signs of multidrug resistance in Africa
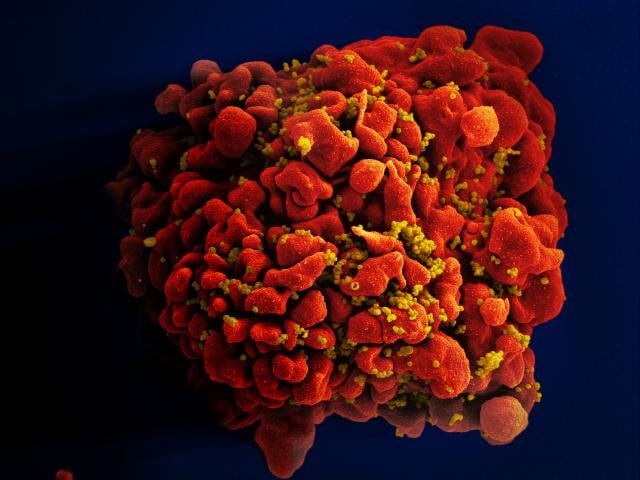
2 December 2016 London School of Hygiene & Tropical Medicine London School of Hygiene & Tropical Medicine https://lshtm.ac.uk/themes/custom/lshtm/images/lshtm-logo-black.pngSignificant numbers of patients whose HIV strains developed resistance to older generation drugs are also resistant to modern drugs, finds a new study published in The Lancet Infectious Diseases.
Conducted by the London School of Hygiene & Tropical Medicine and UCL, and funded by Wellcome, the research analysed 712 HIV patients across the world whose HIV was not controlled by antiretrovirals.
The study found that 16% of people who stopped responding to modern first-line treatments had HIV mutations associated with resistance to an older generation of drugs called thymidine analogues. Among patients with a thymidine analogue mutation, 80% were also resistant to tenofovir, the main drug in most modern HIV treatment and prevention strategies.
Resistance to a drug typically occurs when a patient doesn't take their medication regularly enough, and for first-line treatments to work, patients generally need to take their medication 85-90% of the time. When treatment is not taken as advised the virus can develop a resistance to the drugs, and the latest study shows that HIV can be resistant to many different drugs simultaneously.
John Gregson, co-lead author from the School who worked on the statistical analysis, said: "Our study examined the level of resistance to tenofovir and an older generation of drugs called thymidine analogues, amongst patients failing tenofovir therapy in sub-Saharan Africa. Surprisingly we found that patients who had resistance to thymidine analogues were also more likely to have resistance to other drugs, including tenofovir."
If a patient's virus becomes resistant to first-line drugs, the next stage is expensive second-line treatment with greater side effects. Many rural patients do not have access to such drugs, so it is important to try to preserve the effectiveness of first-line treatments.
Professor Ravi Gupta, UCL Infection & Immunity, Honorary Consultant in Infectious Diseases at The Hospital for Tropical Diseases, UCLH NHS Foundation Trust and study co-author, said: "Mutations for thymidine analogue resistance were previously thought to be incompatible with mutations for tenofovir resistance, but we now see that HIV can be resistant to both at once. This emphasises the need to check the genetic profile of patient's virus before prescribing first-line treatments, as they may have already developed resistance to other treatments that they did not mention having taken."
"To prevent these multi-resistant strains from developing, we need cheap, reliable systems to assess people before treatment. Ideally, we need simple resistance testing kits to help screen for drug resistance before giving treatment. This would also help us to monitor HIV drug resistance globally more effectively. However, until such kits are widely available, we could test the amount of virus in the bloodstream before and after giving treatment. Although not as precise as resistance testing, this could help us to detect treatment failure earlier and switch patients to second line drugs."
Publication
- John Gregson, Pontiano Kaleebu, Vincent C Marconi, Cloete van Vuuren, Nicaise Ndembi, Raph L Hamers, Phyllis Kanki, Christopher J Hoffmann, Shahin Lockman, Deenan Pillay, Tulio de Oliveira, Nathan Clumeck, Gillian Hunt, Bernhard Kerschberger, Robert W Shafer, Chunfu Yang, Elliot Raizes, Prof Rami Kantor, Prof Ravindra K Gupta. Occult HIV-1 drug resistance to thymidine analogues following failure of first-line tenofovir combined with a cytosine analogue and nevirapine or efavirenz in sub Saharan Africa: a retrospective multi-centre cohort study. The Lancet Infectious Diseases. DOI:10.1016/S1473-3099(16)30469-8
Our postgraduate taught courses provide health practitioners, clinicians, policy-makers, scientists and recent graduates with a world-class qualification in public and global health.
If you are coming to LSHTM to study a distance learning programme (PG Cert, PG Dip, MSc or individual modules) starting in 2024, you may be eligible for a 5% discount on your tuition fees.
These fee reduction schemes are available for a limited time only.