LASER aims to facilitate the design, implementation and evaluation of effective disease control programmes. LASER combines expertise in the fields of spatial statistics and GIS technology, quantitative epidemiology and operational research.
The latest news, tools and research findings from the TUMIKIA project. A large scale trial evaluating different targeted interventions to control STH infections in Kenya.
LASER's research portfolio focuses on community and school health, malaria and Neglected Tropical Diseases (NTDs) - in particular, soil transmitted helminths, schistosomiasis, lymphatic filariasis and trachoma.
LASER places a strong emphasis on developing an evidence base that can be used to inform policy and practice. It publishes a wide range of peer reviewed articles and publications in leading science journals.
To help build the capacity of in-country teams LASER have developed a suite of free-to-access training resources including manuals, guidelines, practicals, etc.
Working closely with national and international partners, LASER's research aims to facilitate the design, implementation and evaluation of effective disease control programmes. LASER place a strong emphasis on developing an evidence base that can be used to inform policy and practice.
LASER's research portfolio focuses on community and school health, malaria and Neglected Tropical Diseases (NTDs) - in particular, soil transmitted helminths, schistosomiasis, lymphatic filariasis and trachoma. Generally affecting the very poor, these diseases are termed ‘neglected’ due to their lack of visibility and recognition. Yet they have a devastating impact on millions of people worldwide.
Our research includes:
- The Global Atlas of Helminth Infections (thiswormyworld.org), an open access resource mapping the geographical distribution of NTDs transmitted by worms.
- The TUMIKIA project, a large-scale impact evaluation investigating deworming strategies in Kenya.
- The Learner Treatment Kit Project, evaluation of school-based malaria diagnosis and treatment by teachers in Malawi.
The London Applied & Spatial Epidemiology Research Group (LASER) combines expertise in the fields of spatial statistics and GIS technology, quantitative epidemiology and operational research to build the evidence-base around diseases of poverty and the communities they affect.
Katherine
Halliday
Assistant Professor
Stefan
Witek-McManus
Research Fellow
Hope
Simpson
Research Fellow

Samantha
Owen
Project Manager
LASER’s research portfolio focuses on community and school health, malaria and Neglected Tropical Diseases (NTDs) – in particular, soil transmitted helminths, schistosomiasis, lymphatic filariasis and trachoma.
Generally affecting the very poor, these diseases are termed ‘neglected’ due to their lack of visibility and recognition. Yet they have a devastating impact on millions of people worldwide.
Key research projects include:
- The Global Atlas of Helminth Infections, an open access resource mapping the geographical distribution of NTDs transmitted by worms.
- The TUMIKIA project, a large-scale impact evaluation investigating deworming strategies in Kenya.
- The Learner Treatment Kit Project, an evaluation of school-based malaria diagnosis and treatment by teachers in Malawi.
LASER’s research portfolio - four main themes
-
Spatial epidemiology of NTDs
-
LASER's early research in this area quantified the environmental conditions associated with the large-scale distribution of helminth infections at national and regional scales. This work has employed a variety of analytical approaches, including the use of Bayesian model-based geostatistics. This work has led to a number of insights into the ecology of infection at multiple spatial scales.
This early work also led to the creation of the very first risk maps of the distribution of helminth infection in sub-Saharan Africa and demonstrated that GIS/remote sensing can provide an effective methodology for targeting NTD parasite control at realistic geographical scales.
As interventions are being implemented at scale, LASER are increasingly interested in the spatiotemporal distribution of NTDs. Understanding such distributions can assess the degree to which changes are related to the scaling up of interventions or other factors and can identify factors that contribute to the persistence or cessation of transmission. Better knowledge of the spatiotemporal distribution can also inform the design of optimal surveillance strategies.
Main areas of research include:
- Defining the global climatic limits of STH and LF
- Estimating the population at risk of infection and morbidity caused by STH
- Estimating the global distribution of trachoma
- Defining the pre-intervention distribution of NTDs, including STH, LF and trachoma
- Understanding the factors associated with changes in infection and with the persistence of transmission
- Modelling the contextual factors influencing the transmission of NTDs, including access to water and sanitation
LASER have also worked with the Task Force for Global Health to develop the NTD Mapping Tool, and the International Trachoma Initiative to develop the Global Atlas of Trachoma.
-
Evaluating targeted interventions
-
School-based deworming in Kenya as part of the TUMIKIA trial School-aged children experience some of the greatest burdens of parasitic infections of all age groups, including helminths and malaria, often simultaneously. As well as contributing to ill-health, these parasites can impair cognitive performance and education and are also a source of transmission to other community members.
LASER is interested in identifying possible interventions which could be delivered through schools and are committed to conducting large-scale randomised evaluations of new school-based health interventions and alternative delivery strategies of such interventions. Through conducting multi-sectoral research involving both the health and education sectors, we aim to evaluate the potential impact of school-based programmes to provide policy-relevant guidance.
Main areas of research include:
- Evaluating the relative impact of school-based and community-based deworming on the transmission of STH in Kenya. Learn more about our ongoing TUMIKIA trial.
- Impact and cost-effectiveness of a school-based programme of malaria diagnosis and treatment on school attendance in southern Malawi. Learn about our ongoing Learner Treatment Kit Project.
- Impact of school-based intermittent screening and treatment for malaria in low-moderate transmission settings in Kenya.
- Impact of intermittent preventive treatment with dihydroartemisinin-piperaquine on malaria in Ugandan schoolchildren.
- Effect of intensive deworming on the risks of clinical malaria among Kenyan school children.
-
Optimising surveillance and M&E
-
Data collection in Kenya Once control has been implemented, a key question is: how do we best track changes in infection levels over time?
Any identified surveillance approach will need to take into account the spatial heterogeneity of infection as this will influence the sampling design but also the costs of conducting the surveillance and the administrative unit for which decisions are required. A further consideration is the choice of diagnostic method used to detect infection and how the appropriate method varies according to transmission setting.
We have previously used a combination of computer simulation, geostatistics and cost analysis to evaluate the cost-effectiveness of alternative mapping survey designs for STH and schistosomiasis, and have contributed to the practical targeting of control efforts.
LASER are currently evaluating the cost-effectiveness of alternative diagnostic and sampling methods for the surveillance of NTDs in differing transmission settings. In this work we use a combination of computer-based simulation, fieldwork, statistical analysis and cost-effectiveness analysis.
Main areas of research include:
- Estimating the cost-effectiveness of alternative diagnostic methods for detection of NTDs.
- Evaluating the cost-effectiveness of alternative survey and surveillance strategies for NTDs.
- Evaluating the usefulness of the LF transmission assessment survey (TAS) used for assessing STH infection levels.
- Quantifying the performance of common diagnostic tests for STH and influencing factors, using Bayesian latent class analysis
-
Understanding the context of control
-
Better appreciation of contextual factors is crucial to achieving effective control.
LASER conducts research into the degree by which specific contextual factors, including water and sanitation, impact upon the rate at which individuals become reinfected after treatment, and are working to identify factors that contribute to the persistence or cessation of transmission.
Working with collaborators within LSHTM and at the Kenya Medical Research Institute (KEMRI), LASER are also interested in understanding the main determinants affecting community responses to control programmes with a focus on how health behaviours, including hygiene and drug uptake, can be increased and/or sustained. Its earlier work has provided insight into local perceptions of school-based malaria control, and our attention is now focused on consideration of factors influencing community perceptions and acceptability of community-wide deworming.
LASER are increasingly interested in the impact of helminth control programmes on community primary care structures and the broader health system, and understanding the role of such programmes in health system strengthening.
Main areas of research include:
- Modelling contextual factors influencing transmission of helminth infections, including access to water and sanitation.
- Developing standardised approaches to measuring water, sanitation and hygiene in helminth control programmes.
- Understanding the factors associated with changes in infection and with the persistence of transmission.
- Understanding community perceptions of community and school-based treatment programmes.
- Investigating how helminth control programmes interact with broader health systems.
Research in Focus: The Global Atlas of Helminth Infections
Launched in 2012 by LASER, GAHI provides NTD stakeholders with maps and data describing helminth (worm) infection distribution in 124 countries. All available information is collated into a single database on the prevalence soil-transmitted helminths (STH), schistosomiasis, and lympathic filariasis (LF).
Users are able to access over 950 ready-made maps, or create and download their own bespoke maps using a dynamic web app. Users can also query and download the 23,000+ data records drawn from 10,000 NTD surveys that are used to create the maps.
The data used by GAHI is sourced from exhaustive, structured searches of historical and contemporary formal and grey literature for rigorous and reliable NTD surveys. To ensure that only reliable surveys are included in GAHI, pre-determined inclusion criteria are applied to information identified through searches. Surveys are identified using a combination of approaches, including:
- Searches of electronic bibliographic databases
- Manual searches of local archives and libraries
- Direct contact with researchers and institutions
GAHI only uses data for which is it has release permissions or that which is already published elsewhere. The geographical location – the longitude and latitude – of surveyed schools and communities is then determined to allow the mapping of data.
Users are able to access maps by geographical location, by worm and by the type of map. To find out more visit www.thiswormyworld.org.
The TUMIKIA Project aims to determine the most cost-effective treatment strategy and delivery system to achieve the ultimate goal of interrupting transmission of soil-transmitted helminths (STH or intestinal worms). TUMIKIA stands for 'Tuangamize Minyoo Kenya Imarisha Afya' this is Swahili for 'eradicate worms in Kenya to improve health'.
The two-year project brings together research expertise from the LSHTM, the Kenya Medical Research Institute, the Kenyan Ministry of Health and Ministry of Education, Science & Technology, Imperial College London and Deworm the World at Evidence Action.
The project implemented a large cluster randomised trial in Kwale county, Kenya to evaluate three different strategies:
- Annual school-based deworming: pre-school and school-age children receive deworming once a year as part of the national school-based deworming programme.
- Increased coverage: all community members (including adults) receiving deworming once a year delivered by community health workers.
- Increased coverage and frequency: all community members (including adults) receive deworming twice a year delivered by community health workers.
-
Research components
-
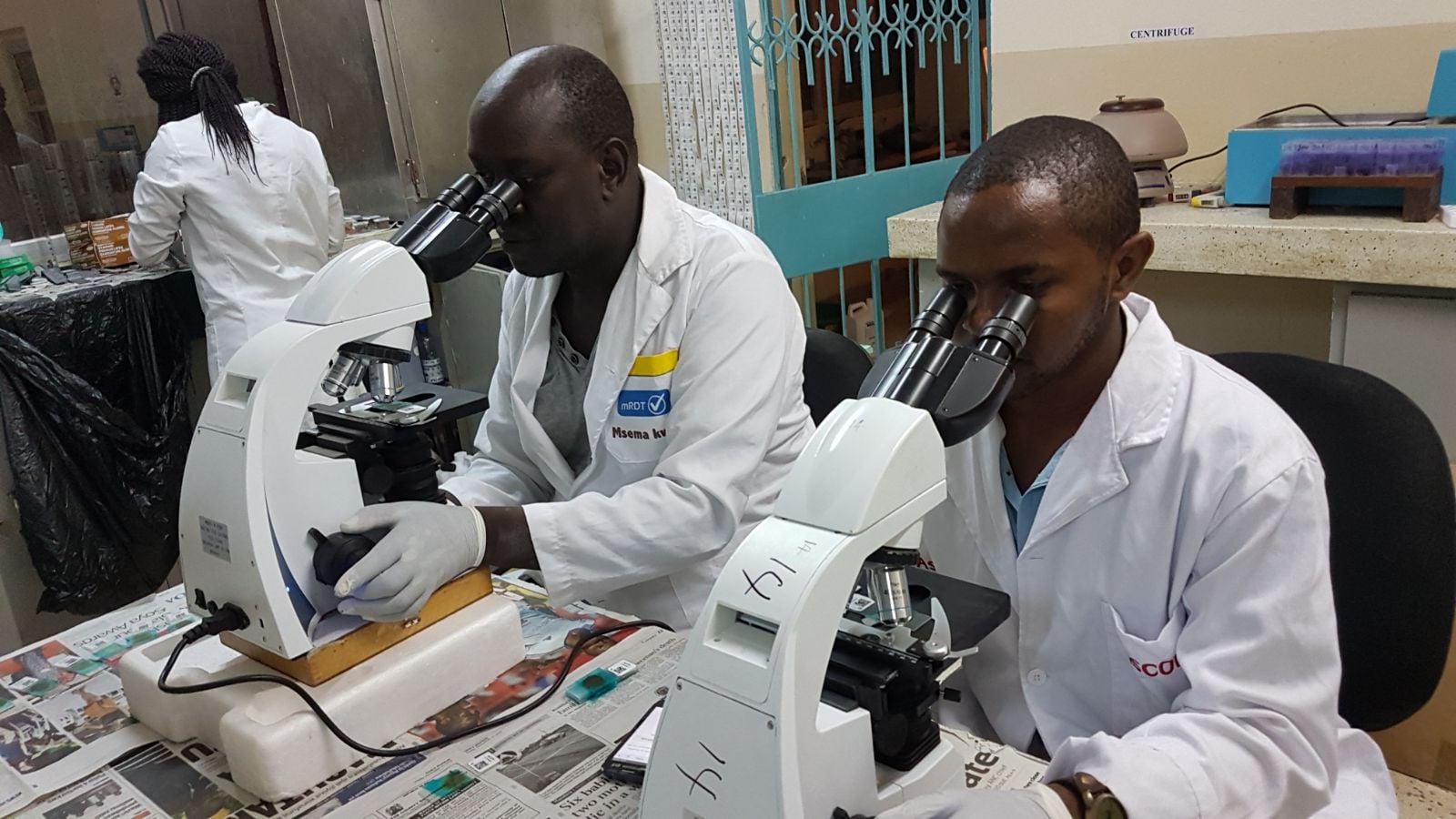
TUMIKIA laboratory technicians measuring STH prevalence The mainstay of STH control is school-based deworming (SBD), but mathematical modelling has shown that in all but very low transmission settings, SBD is unlikely to interrupt transmission, and that new treatment strategies are required.
The TUMIKIA project aims to evaluate the impact and cost-effectiveness of community-based versus school-based deworming on STH transmission in Kenya.
A range of quantitative and qualitative assessments are evaluating the impact, costs, cost-effectiveness, acceptability and feasibility of the different strategies and delivery systems.
The TUMIKIA project contains a number of research components:
Quantifying the impact of community-based deworming versus school-based deworming in reducing transmission of STH
The primary outcome measure of the TUMIKIA project is prevalence of hookworm, which is assessed during repeat cross-sectional prevalence surveys targeting 27,000 individuals across the 120 clusters. Secondary outcomes are prevalence of Ascaris lumbricoides and Trichuris trichiura and the intensity of infection with each species.
Investigating epidemiology and infection dynamics of STH infection
Detailed worm expulsion studies and longitudinal parasitological monitoring within a nested cohort of participants were conducted. Together with colleagues from Imperial College London, these data are being used to re-parameterise mathematical STH transmission models. In addition to informing the design of the DeWorm3 multicentre trial, these models are being used to estimate time-to-elimination under each treatment strategy.
Evaluating the costs and cost-effectiveness of alternative STH treatment strategies and delivery systems in reducing transmission and improving health outcomes
The optimal treatment strategy for STH will ultimately depend on their relative cost-effectiveness. A comprehensive ingredients-based costing framework was developed to enable the evaluation of costs from provider and societal perspectives. This framework will be used to estimate the cost-effectiveness of the trial arms, in addition to linking with STH transmission models to evaluate the cost-effectiveness of maintaining and scaling up strategies.
Evaluating the acceptability and feasibility of different treatment strategies and delivery systems
Partners from KEMRI and from the Department of Global Health and Development at LSHTM are seeking to identify key assumptions and conditions underlying the sustainability and scaling-up of the different strategies and delivery systems. A detailed qualitative analysis is being conducted that is focusing on community acceptability and feasibility, including evaluation of health system factors at local and national scales levels that enhance or constrain effective implementation.
Understanding coverage and compliance during community-based deworming
The TUMIKIA project has generated one of the largest longitudinal databases on anthelmintic treatment coverage and compliance. Household treatment records from consecutive rounds of community-based deworming will be used to identify determinants of compliance with deworming treatments, and understand its impact on the effectiveness of alternative control strategies.
-
Research tools and resources
-
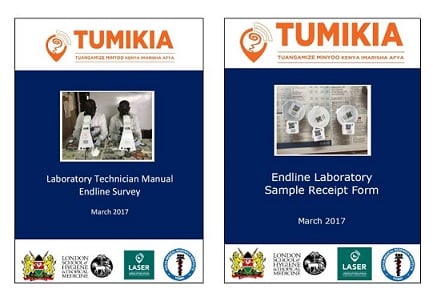
The TUMIKIA Project’s research and implementation activities were underpinned by electronic data collection using Android smartphones. All data collection forms used in the field and laboratory were developed by the project team and programmed by Dr William Oswald, Stefan Witek-McManus, and Stephen Okiya for use with the SurveyCTO (Dobility, Inc.) mobile data collection platform. Manuals, printable copies of forms, and the respective xlsforms (programmed for use with SurveyCTO) are provided here.
Household Questionnaire and Stool Sample Collection Form
This form was used by TUMIKIA field officers during cross-sectional parasitological surveys and includes a census, sociodemographic questions, and reported and observed measures of water & sanitation access. A randomisation function selects a household member to answer individual-level behaviour questions and provide a stool sample. The form includes scanning of QR codes on sample pots, efficiently linking household and individual data with laboratory results.
The download includes:
- Field Officer Manual
- Household Questionnaire and Sample Collection Form - Includes a printable version and xlsform for use with SurveyCTO
Download the Household Questionnaire and Stool Sample Collection Form
Laboratory Kato-Katz Forms
A suite of forms covering the processes for stool samples in the laboratory, from sample receipt, slide reading and reporting, to quality control. All forms are centred on the unique sample QR code used in the field.
The download includes:
- Laboratory Technician Manual
- Laboratory Sample Receipt Form – Includes a printable version and xlsform for use with SurveyCTO
- Laboratory Kato-Katz Reporting Form – Includes a printable version and xlsform for use with SurveyCTO
- Laboratory Kato-Katz Quality Control Reporting Form – Includes a printable version and xlsform for use with SurveyCTO
-
News and blogs
-
Deworming 300,000 in Kenya - a photo essay Innovative TUMIKIA research project nears completion (May 2017) Following the completion of the TUMIKIA endline survey trial coordinator Dr Kate Halliday discusses the opportunities and challenges of surveying 24,000 households.
Deworming 300,000 in Kenya a photo essay - Feb 2017 - Documenting the training, community sensitisation and the people engaged in the deworming component of the TUMIKIA project.
How do women perceive the risks and rewards of deworming during pregnancy? (Dec 2016) Seeking to address the lack of information about how women perceive the risks and rewards of NTD treatment. Claire Gwayi assesses how women feel about deworming during pregnancy.
What 26,000 stool samples can tell us (Nov 2016) As the TUMIKIA project reaches its halfway point, Dr Kate Halliday and Dr William Oswald describe a recent midline survey conducted in households across Kwale county, coastal Kenya, as part of a large-scale cluster randomised trial.
WASH conditions in schools (June 2015) Discussing the relationships between water, sanitation, and hygiene (WASH) conditions and soil transmitted helminths LASER's Dr William Oswald shares preliminary observations made on primary school water, sanitation, and hygiene conditions in Kwale County, Kenya.
Worm expulsions (June 2015) An account of efforts to measure the actual burden of infection of people in Kwale by PhD student, Rita Oliveira, Imperial College London.
Developing effective trainings and materials (May 2015) Creating training materials for community health volunteers in our Tumikia Project, which is assessing different treatment strategies for control and elimination of soil-transmitted helminths.
-
Associated publications
-
Brooker et al, 2015 Interrupting transmission of soil-transmitted helminths: a study protocol for cluster randomised trail evaluating alternative treatment strategies and delivery systems in Kenya. BMJ Open 5:10
Funding
The TUMIKIA Project is possible thanks to generous funding from The Bill & Melinda Gates Foundation, with additional support from the Joint Global Health Trials scheme, Children's Investment Fund Foundation and the Wellcome Trust.
Improving programme implementation to achieve disease control goals is a multidisciplinary endeavour. Understanding the gap between the availability of evidence-based interventions for disease control and their actual implementation in a real setting warrants a pragmatic approach to scientific inquiry that brings together a variety of disciplines, including statistics, epidemiology, systems engineering, and social sciences. Integrating these approaches to plan, monitor and evaluate programmes can improve programme reach, treatment uptake, and the effectiveness of their delivery.
Recently, our research group has incorporated qualitative methods in its approaches to study the integrated control of skin neglected tropical diseases (NTDs). Integrated programmes, as opposed to disease-specific control programmes, are an emerging paradigm for the control of skin NTDs since they may improve effectiveness of resource allocation for case finding and management activities. Several arguments support programme integration beyond managerial or budgetary reasons, including similar disease presentations, co-endemicity, and shared need for case management strategies including long term chemotherapy, daily wound care, and physical rehabilitation. While international partners and academics alike have recommended integrated programmes for morbidity management, there are few reports on how people affected by these diseases experience being brought together in natural settings.
At the border between Liberia and Guinea, a rehabilitation centre has recently integrated care for Buruli ulcer (BU) with leprosy care activities. In 2018, as part of our work with Accelerating Integrated Management (AIM) and the Ministry of Health in Liberia, our research group conducted a qualitative study in this facility to understand experiences of integrated care for these two diseases. Specifically, we interviewed people affected with BU and multibacillary leprosy to understand their experiences of illness, their pathways to access care, and their experiences of receiving integrated case management.
We found that, while in their communities, both groups of patients experienced similar instances of stigma and disability associated with these skin diseases, leading to social isolation and limited economic productivity. Our study also contributed to understanding that folkloric beliefs on the cause of illness, use of traditional medicine, and the influence of others in health decision-making shaped the presence of people with BU and leprosy in the rehabilitation facility. These results can now be used to guide the development of innovative interventions for disease control, including exploring the opportunity of recruiting traditional practitioners to support case referral, and leveraging the role of skin NTDs survivors in the community to improve health-seeking behaviour towards biomedical services.
Our focus on how people experienced integrating care of these diseases identified that both groups perceive receiving their medications and wound care together favourably. However, we identified some negative experiences including unjustified fear of acquiring the other disease, intense pain during the process of wound cleaning, death among severe cases of BU, and permanent disability due to lack of physiotherapy. These results have been communicated to the Ministry of Health of Liberia with a set of recommendations to ensure their integrated control programme achieves its goal of mitigating the burden associated with skin NTDs.
Our work using qualitative methods in this rehabilitation facility in Liberia is being used to guide intervention development and suggest programmatic improvements. Our experience exemplifies how social sciences might support epidemiological approaches in understanding how pathogens distributed over populations interact with them, and the behaviours that perpetuate these infections.
We are looking to appoint a Project Coordinator (Maternity cover) to lead on the administrative and financial management of our projects. If you have experience in providing administrative support of academic research; are able to oversee large budgets; and can work to a high degree of accuracy with a heavy workload then this could be the role for you. Please see the full job advert for further details and guidance on how to apply.
Routine Surveillance Data as a Resource for Planning Integration of NTD Case Management
Integrated management of neglected tropical diseases (NTDs) has been recommended by the World Health Organisation as a way to tackle the burden of morbidity due to these diseases, which remains high as their transmission has been reduced. Ghana is an example of a country which has committed to finding innovative ways to integrate control and management of multiple NTDs. One approach is to integrate care for patients with leprosy, Buruli ulcer (a disease which destroys skin and bone tissue), and lymphatic filariasis (causing elephantiasis). To identify communities that may benefit from integration, we need to identify where these diseases co-exist. This is a challenge because data on NTDs is currently limited, and costly to collect.
We piloted a low-cost solution to this problem, working in collaboration with the Ministry of Health, the leprosy, Buruli ulcer and lymphatic filariasis programmes in Ghana, and the AIM Initiative, which supports these programmes. We collected data on leprosy and Buruli ulcer patients recorded in health facilities, and on cases of lymphatic filariasis found in mass drug administration campaigns. By mapping the communities of these cases, we identified districts and communities where two or more of the conditions occurred. These are targets for integrated NTD control and management.
We also used these maps to estimate the distance that patients would have to travel to a health facility. We speculated that patients making longer journeys may experience delays to diagnosis, potentially resulting in disease progression. To explore this, we categorised patients into groups with higher and lower levels of disability, and compared the average distance from their community to the nearest health facility. We found that leprosy patients living further from health facilities did have a higher risk of disability when they were diagnosed. Access to health facilities is therefore a potential driver of leprosy-related disability. This is an important finding, supporting investment in universal healthcare to improve access to health for all. Integration of NTD management is one way this situation may be improved.
This investigation does not show the whole picture- we only mapped cases that were already diagnosed and known to the health system. Undoubtedly, this only represents a fraction of the true burden of leprosy, Buruli ulcer and lymphatic filariasis in Ghana, and opportunities to integrate and widen access to care would be much greater if all patients could be mapped. In practice, this can only be achieved through an exhaustive survey, systematically reaching all communities to identify patients for whom access to health services is a barrier to diagnosis and treatment. To find out more how LASER is tackling this challenge in Liberia see our previous blog post titled "Case finding NTDs in Liberia's rainy season".
Over the past six months the LASER team have been working alongside the national Neglected Tropical Disease (NTD) programme of Liberia and the AIM Initiative to develop new case finding tools to find those suffering with a range of NTDs of the skin. Here, we report on just some of the challenges encountered by our field teams in rainy Maryland County.
Successful case finding is a cornerstone of many health programmes, irrespective of where you are or what resources you have. The ultimate goal is to identify everyone possible with the disease of interest. However, the diverse diseases and local situations that play out all over the world mean that case finding can look very different from one place to another. Offering mammograms to all UK women aged 50 to 70 in specialist breast screening units represents one example of case finding. Walking door-to-door through tropical Liberian forests showing pictures of skin NTDs is a very different approach. Yet both are striving towards the same goal.
Liberia is burdened by a number of long-lasting and disfiguring NTDs that affect the skin. Finding them, however, is difficult. Many of those affected live in remote communities who lack access to high quality health care, as well as most other things we associate with development. Some skin NTDs also occur most often during periods of rain and high humidity, so this can be a good time to look. This must be balanced against the additional logistical demands of the wet season, as the use of cars quickly becomes unfeasible, then, as rains intensify, even motorbikes stop being useful. At this point walking can become the only reliable way of reaching affected communities.
For our survey, the workforce given the task of door-to-door case finding during these long months is the local community health worker (CHW) cadre. Across Liberia, nearly all villages elect one or more CHWs as part of a national programme to improve access to healthcare in hard-to-reach populations. These are probably the only people with the combination of local knowledge and toughness to get this job done.
To ensure nobody was left behind during our case finding activities, each CHW was held responsible for visiting every last family in their community to look for skin NTDs. A team of nationally trained expert verifiers then had to visit the community of every potential case. This strategy entailed long periods of work in very remote areas with no electricity or network coverage. As the rivers swelled, moving people and equipment over large distances proceeded ever more slowly, and with greater risks. All this created serious challenges, as the project depended upon real-time mobile electronic data collection and GPS information to monitor every moment of field activities in fine detail.
To overcome these obstacles, the field teams were forced to come up with a number of both high and low-tech fixes. This included kitting out every field worker with high capacity power banks, so they can work unimpeded for extended periods in the bush. We also provided dry bags normally reserved for kayaking expeditions, so that even the CHWs who needed to swim across rivers to get home could do so without jeopardising their equipment. A lack of mobile data coverage presented an almost insurmountable challenge at times. An ad-hoc network of collection points, bike couriers and mobile hotspots did, however, facilitate a network of smartphones moving across the county that enabled regular data monitoring.
Despite these challenges, CHWs achieved laudable coverage of their communities. Their case-finding activities also provided an essential link between each newly identified patient and their local health facility, ensuring that patients were able to receive appropriate treatment. Through their tireless efforts, the CHWs have helped ensure that their remote communities are one (rain-booted) step closer to achieving the ultimate goal of Universal Health Coverage.
In 2013, analysis by the World Health Organisation (WHO) showed that in Myanmar over 42 million people were at risk of infection from at least one neglected tropical diseases (NTDs) including soil transmitted helminths (STH), leprosy, lymphatic filariasis (LF) and trachoma.
When trachoma was taken on its own, 18 million people lived in areas where trachoma was a known risk and approximately 66,000 were suffering from the advanced stage of the disease leading to visual impairment and permanent blindness (Global Atlas of Trachoma, 2013).
To support national programmes in countries such as Myanmar to control and eventually eliminate NTDs as a public health issue, the WHO’s Regional Office for South East Asia developed the Regional Strategic Plan for Integrated NTD control in South-East Asia Region.
This strategic plan identified four main intervention packages:
- Mass drug administration for LF, STH, Schistomsomiasis and trachoma;
- Integrated vector management for vector-borne NTDs (LF, kala-azar, dengue and Japanese encephalitis);
- Case-finding and treatment for leprosy, kala-azar, trachoma and yaws; and
- Integrated disability prevention and care for LF and leprosy.
Recent years have seen remarkable progress in the control of NTDs, with increased availability of funding and the establishment of national NTD control programmes. As countries develop their programmes, data on the geographical distribution of NTDs are required to target treatment to areas of greatest need and to estimate drug and resource requirements. In addition, as interventions are scaled-up, national governments and donors require clear information on the progress in control efforts.
In line with this approach, the Ministry of Health in Myanmar is working to integrate NTD data from a range of different sources, to develop a national geodatabase of NTDs. This is intended to make surveillance more efficient, and help to target integrated control and case-management of NTDs.
In support of this work, representatives from across Myanmar’s NTD community are undertaking an intensive 5-day training course to develop the necessary skills and tools they need to be able to collate, analyse and utilise this NTD data.
With a focus on the mapping of leprosy, lymphatic filariasis and trachoma, the course is designed to provide them with the skills and the tools needed to design, implement and evaluate targeted and effective NTD control programme.
As well as creating integrated maps to show where these diseases overlap in Myanmar, participants will be mapping disease-specific indicators to track progress against WHO targets for NTD control. Participants will also build general skills in data management and analysis, which will further strengthen Myanmar’s NTD control programmes.
The course is being taught by researchers from the London Applied & Spatial Epidemiology Research (LASER) group based at the London School of Hygiene & Tropical Medicine, in partnership with the AIM initiative.
Further resources
The training manual including all of the practical tutorials developed by LASER for this workshop are freely available to download from the GAHI training page.
The Mapping of Intensified Case Management NTDs using Quantum GIS 2.18.9
Practical 1: Becoming familiar with Quantum GIS interface and GIS features (pdf)
Practical 2: Managing data tables and creating spatial data sets (pdf)
Practical 3: Creating your map layouts using the print composer in QGIS (pdf)
Practical 4: Approaches to geo-referencing locations (pdf)
Practical 5: Basic GIS geoprocessing (pdf)
Download the complete Modern Tools for NTD Control Programmes: Practicals 1- 5 (pdf)
Data
Data for practicals 1-5 (zip)
Translations
Download the French translation: Outils modernes pour les programmes de contrôle des MTN (pdf)
Cameroon’s Ministry of Public Health recently hosted an innovative disease mapping training course to equip public health specialists with the skills needed to map and manage the incidence and treatment of six neglected tropical diseases.
The 4 day course was taught by researchers from the LASER group (London Applied & Spatial Epidemiology Research) based at London School of Hygiene & Tropical Medicine, in partnership with the AIM initiative and representatives from the Ministry of Public Health.
Attendees, including medical practitioners, field workers, data and programme managers, were trained in integrating case-management and NTD morbidity data (CM-NTDs) for Leprosy, Yaws, Lymphedema, Cutaneous Leishmaniasis, Trachoma and Buruli Ulcer into a mappable format using QGIS software.
These skills are a vital component of the Ministry’s efforts to support the design and targeting of Cameroon’s national NTD control programmes through the development of a national GIS health database of disease-specific indicators for Leprosy, Yaws, Lymphedema, Cutaneous Leishmaniasis, Trachoma and Buruli Ulcer.
The course trained stakeholders to convert this NTD data into maps and visual representations that can be used to guide their efforts for NTD case management and control.
The course included an overarching introduction on how to manage CM-NTDs within a QGIS’ interface and techniques to display the geographical distribution of incident cases and morbidities for varies illnesses. The tutorial also included methods to utilise online resources (e.g. OpenCage Geocoder) for geolocating point data with missing coordinates and geoprocessing tools for complex spatial queries and analyses.
The tutorial practical and manuals (and accompanying datasets) developed by LASER for this training are free to download from the thiswormyworld.org training pages.
Practical downloads:
- Practical 1: Becoming familiar with QGIS interface and GIS features
- Practical 2: Managing data tables and creating spatial data sets
- Practical 3: Creating your map layouts using the print composer in QGIS
- Practical 4: Approaches to georeference locations
- Practical 5: Basic GIS geoprocessing
Download the French translation
Additional Training Resources
LASER have developed a series of free to download GIS practicals to build capacity in NTD mapping.
Download the Practical Guidelines for Users of Quantum GIS 2.
A major challenge facing mass drug administration (MDA) programmes targeting the control and elimination of lymphatic filariasis or onchocerciasis is the serious adverse - sometimes life threatening - reactions that this treatment can have on people who are also infected with loisasis. Commonly known as Eye worm, loisasis is caused by the parasitic worm Loa loa and is mainly found in forested regions in Africa and India. Those individuals with high levels of co-infection are the most likely to experience adverse reactions to ivermectin, the deworming drug used to target lymphatic filariasis and onchocerciasis.
The risk of severe adverse reactions is such that MDA isn’t recommended by the WHO in onchocerciasis-endemic communities that are likely to have a large number of highly infected individuals with loiasis. It is very important, therefore, to assess the level of loiasis endemicity in a community before initiating mass treatment.
To better quantify the burden of Loa loa infections in Western Africa, LASER's and CHICAS’s Emanuele Giorgi, together with colleagues from Lancaster University, have developed a new methodology to analyse the prevalence and intensity of infections in communities (measured by microfilia load per ml blood) alongside their spatial distribution.
This approach is highlighted in a recently published paper “Giorgi E, Schlüter DK, Diggle PJ. Bivariate geostatistical modelling of the relationship between Loa loa prevalence and intensity of infection. Environmetrics. 2017;e2447”.
One feature of the data analysed in the paper, is the high number of zero counts, which makes the use of standard geostatistical methods for prevalence data inappropriate. This phenomenon, also known as zero inflation, is typical of count data from neglected tropical diseases, whose endemic boundaries are often unknown, thus leading to the inclusion of disease-free communities in the sampling frame.
The paper introduces a bivariate geostatistical model in order to study the relationship between the distributions of prevalence and intensity of Loa loa infections at the community level. It shows through a simulation study that the spatial model leads to more precise predictions of the proportion of individuals in a village with more than 8000 microfilia per ml of blood, than previous non-spatial approaches and accordingly provides a geostatistical reanalysis of the Loa loa data.
This work shows how geostatistical methods allow public health researchers to make the best possible use of data on disease rates by exploiting their spatial correlation (“close things in space are more related than distant things”). This has the potential to improve the effectiveness of control programs by targeting more precisely communities that are likely to include individuals at high risk of experiencing a serious adverse reaction to ivermectin.
Over the past two years, researchers from London School of Hygiene & Tropical Medicine and the Kenya Medical Research Institute have been conducting one of the largest research project of its type to answer the question of how best to treat the world’s most common neglected tropical disease - soil transmitted helminths (STH).
As the TUMIKIA project nears completion, the trial coordinator Dr Kate Halliday outlines the opportunities and challenges of surveying 24,000 households in Kwale County, Kenya.
Strengthening the evidence base
More than 1.5 billion people globally are infected with at least one species of STH (intestinal worms, which include roundworm, whipworm and hookworm). As diagnosis of STH is relatively expensive, mass treatment for STH in ‘high-risk’ groups – such as school-age children - in the form of a deworming tablet once a year is a safe, efficient and cost-effective method of reducing levels of STH infection. This strategy has been recommended by the World Health Organisation for almost two decades.
Despite the successful scale-up of school-based deworming programmes, in many communities the highest levels of STH continue to be found in adults, who are not routinely treated. As a result, re-infection with STH occurs rapidly, requiring indefinite annual re-treatment of all school-children in endemic areas.
Recent mathematical modelling has predicted that broadening mass treatment for STH to all individuals – not simply those at highest risk - may potentially be a more effective way to reduce STH infection across the entire community. To address this knowledge gap and advise policy makers both nationally and globally, the TUMIKIA research project has set out to evaluate whether community-based deworming is more effective at controlling – and ultimately eliminating – STH.
What's the optimal approach?
The two-year TUMIKIA project brings together research expertise from the LSHTM, the Kenya Medical Research Institute, the Kenyan Ministry of Health and Ministry of Education, Science & Technology, Deworm the World at Evidence Action and Imperial College London to evaluate the effectiveness of three different approaches to tackling STH;
- Annual school-based deworming: where only pre-school and school-age children receive deworming once a year
- Increased coverage: where all community members (including adults) receiving deworming once a year
- Increased coverage & frequency: where all community members receive deworming twice a year
In early 2015, an initial baseline survey of 24,000 households drawn from villages and communities across Kwale was conducted to measure the levels of STH infections and collect data on factors which could influence STH infection. Participant communities were then split up into 120 clusters of about 1000 households, and randomly assigned to one of the three treatment approaches under investigation.
Following two years of school-based and/or community-based deworming the survey teams have now returned to conduct a final endline survey to evaluate the effect of these different strategies on STH infections in each participant community. The endline survey began in mid-March, running until mid-May.
The design of the endline survey mirrors that of the baseline survey. From each cluster, 225 households are selected at random to take part in a survey which records the size and composition of the household, their socio-economic status, and hygiene and sanitation practices. One family member is then selected at random to provide a stool sample for STH analysis.
Logistical challenges of research
To embark on a survey of this size is a considerable logistical undertaking. More than 110 field officers, 40 laboratory technicians and 30 data officers have been hired to collect, analyse and record the 24,000 surveys and stool samples collected.
At each household, field officers use a specially programmed smartphone to conduct a detailed questionnaire. As well as conducting a census, the questionnaire aims to builds a picture of each household by collecting data on a range of factors - from the number of livestock the household owns, to the sanitation practices of household members. At the end of each questionnaire the smartphone randomly selects one household member to provide a stool sample for analysis.
One of the key challenges facing the research project is the distance and terrain that each team has to cover. Some of the clusters are a 260 kilometre roundtrip from the study office, while others require the teams to use a combination of cars, motorbikes and boats to reach remote communities. Once teams arrive at their study cluster, field officers are often faced with dispersed communities requiring a long day of walking between households.
Teams of technicians set up the laboratory at local health facilities near each of the clusters being surveyed to analyse the day’s samples. Microscope slides created from these samples are read using the kato-katz technique to estimate the number of STH eggs present. Using this approach, researchers are able to estimate the number and intensity of STH infections in each community.
A proportion of samples are preserved and stored for subsequent molecular analysis.
A system of checks and measures
Smartphone data collection has not only improved the speed and efficiency of conducting a survey on this scale with the use of barcodes for samples scanned in the field and then again in the lab, but has also enabled the study team to develop thorough data monitoring processes that can be used in real time to ensure that data being collected is both accurate and representative.
For example, while each questionnaire is being conducted the smartphones collect and transmit a series of GPS coordinates, as well as measuring the time taken to complete each questionnaire. Once each completed questionnaire has been uploaded at the end of the day, the entire dataset can be reviewed immediately. This allows the TUMIKIA supervisors to closely monitor the work of all team members, ensuring the integrity of the final dataset.
What’s next?
The results of each stool examination - along with household and individual data collected by questionnaire - will be compared with results from the baseline survey to determine whether community-based deworming is a more effective approach than school-based deworming alone to control and eliminate STH infections.
The findings from this research will be announced by the end of 2017.
Additional reading
Business Daily Africa's Sarah Ooko highlights the work of Kenya's Ministry of Health and LSHTM researchers to tackle neglected tropical diseases.
Kenya's Ministry of Health is urging Kenyans to undergo regular deworming - at least once a year - so as to avoid complications brought about by intestinal worms.
The parasites deplete the body of vital nutrients or impede their absorption, leading to malnutrition that lowers an individual's immunity to infections.
In severe cases, thousands of worms can infest the body and clog intestines, causing bowel and stomach complications.
Without timely surgery to remove the worms, which usually resemble long entangled spaghetti strands, affected patients end up losing their lives.
According to Dr Sultan Matendechero, head of the Neglected Tropical Disease (NTD) unit at the Ministry of Health (MoH), most people tend to ignore these parasites as they lack awareness of the hazards they pose.
Pregnant women, children most affected
He said that children and expectant women are the most affected by intestinal worms which include roundworms, hookworms and whipworms - collectively referred to in medical terms as soil transmitted helminths (STH).
“But that doesn’t mean others are safe. We are all vulnerable since the worms are endemic to Kenya,” he said.
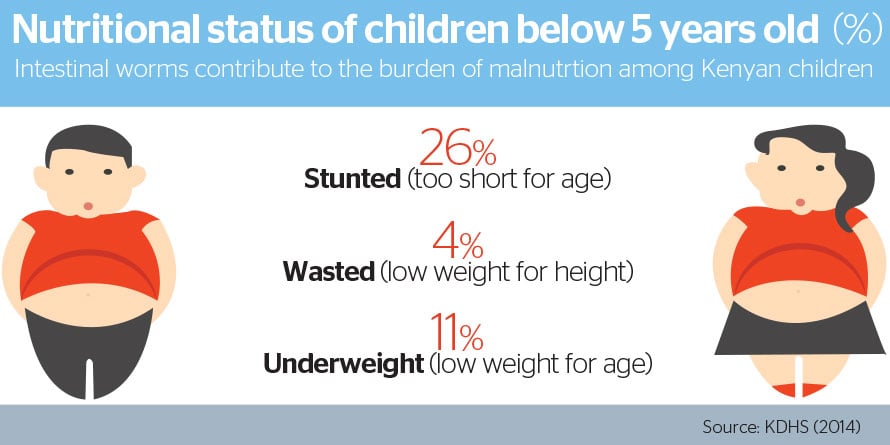
Aside from causing diarrhoea which is a leading cause of child mortality in Kenya, malnutrition caused by intestinal worms also impedes optimal mental and physical development in children.
In pregnant women, the parasites cause anaemia, which increases the risk of premature delivery and death resulting from excessive bleeding at birth.
Nyanza, Western, Costal and South Rift regions bear the highest burden of the intestinal worms in Kenya.
In these areas, the government has been conducting mass drug administration (MDA) campaigns where children of school going age (between 5 and 15 years) are given deworming tablets each year to treat and lessen the burden of the worms.
The World Health Organization and the Bill and Melinda Gates Foundation have supported deworming programmes in low-income countries, with previous studies indicating that treatment could help keep children in school.
Improving impact
Despite the successful scale-up of such programmes, in many communities the highest levels of infections continue to be found in adults, who are not routinely treated through mass deworming programmes. As a result, re-infection occurs rapidly, requiring the re-treatment of school-children to be conducted every year.
“We usually treat the children then they end up becoming infected again after some months. We suspect that they get the worms from other members of the community who weren’t treated,” said Dr Matendechero.
To address this challenge, the MOH - in collaboration with the London School of Tropical Hygiene and Medicine (LSHTM) and the Kenya Medical Research Institute (KEMRI) - is conducting a study to determine whether deworming campaigns targeting school children and other community members in high-risk regions can effectively lower the prevalence of intestinal worms.
The results of the research, which will be replicated in other African countries, are expected to inform WHO guidelines on the management of intestinal worms.
“Kenya is leading the way in this major research that will provide a way forward in the management of intestinal worms,” said Dr Katherine Halliday, assistant professor at LSHTM who is the coordinator of the TUMIKIA study.
She said as well as deworming campaigns, proper hygiene, safe water and good sanitation practices play a significant role in eradicating worms and preventing re-infection after treatment.
Intestinal worms are transmitted by eggs present in human faeces which contaminate the soil in areas where sanitation is poor.
People infested with this parasite can be effectively treated using a sweet flavoured deworming medicine known as Albendazole that is available in many public and private health facilities.
Intestinal worms contribute to the burden of neglected tropical diseases (NTDs) in the country that are hampering the nation’s development.
The above is adapted from an article posted on the Business Daily website on 11 May 2017 - Read the original article on the Business Daily website.
The World Health Organisation’s Expanded Special Project for Elimination of Neglected Tropical Diseases (ESPEN)* have launched a new open-access AFRO NTD portal mapping the prevalence of the five most common neglected tropical diseases (NTDs) in 37 African countries.
Launched at the Geneva NTD Summit in April 2017 the online portal provides prevalence maps and data downloads for the following diseases; lymphatic filariasis (LF), onchocerciasis, soil-transmitted helminths, schistosomiasis and trachoma.
The platform draws on data provided by the participant countries and is targeted at health ministries and their stakeholders. The portal enables them to make informed decisions on how best to design public health initiatives to control and eliminate NTDs.
London Applied & Spatial Epidemiology Research Group (LASER) through its Global of Atlas of Helminth Infections have been providing technical support for the development of the maps featured on the portal.
On announcing the launch Dr. Matshidiso Moeti, the WHO Regional Director for Africa, said, “As scaling up mass drug administration for the over 600 million people who need preventive chemotherapy remains one of the biggest challenges in the region, this NTD portal illustrates WHO AFRO’s bold ambition to take focused and unwavering action”.
Highlighting this collaborative approach for development of the ESPEN project Dr Magda Robalo, Director of the Communicable Disease Cluster at the WHO said, “The NTD portal illustrates our strong commitment to quality data. We will continue to work with all our country partners to collect quality data and continuously improve the functionality and accessibility of the platform.”
Support for the complete mapping of LF, onchocerciasis, soil-transmitted helminths and trachoma in Africa is provided by the Bill & Melinda Gates Foundation. The portal’s trachoma maps draw on data collected from the Global Trachoma Mapping Project supported by DFID and USAID.
Further Reading
Even amongst public health professionals podoconiosis (or endemic non-filarial elephantiasis) is one of the more neglected of the neglected tropical diseases (NTDs). But much like the better-known polio or guinea-worm disease, the elimination of this debilitating condition is within sight. This eradication is only possible if proper clinical management and preventative measures can be effectively targeted at the communities affected.
To enable this targeting, researchers from LASER are part of an international effort to develop the first Global Atlas of Podoconiosis.
Podoconiosis is a non-infectious geochemical disease caused by chronic exposure to red clay soils derived from volcanic rock. Irritant particles are absorbed through the feet and collect in the lymphatic vessels and nodes of the lower legs, causing swelling, pain, immobility and disfigurement. Sufferers are often misdiagnosed with lymphatic filarias which though caused by parasitic worms results in similar disfigurements.
It isn’t currently known exactly how many people suffer from podoconiosis, estimates put it at around 4 million people mainly in tropical countries of Africa, Central and South America, and southeast Asia.
In Ethiopia and north-west Cameroon podoconiosis is endemic affecting 4-8% of the population. At these levels of infection, alongside the debilitated clinical effects, the disease poses an immense economic burden, with estimated costs to Ethiopia’s economy of US$208 million per year.
Podoconiosis is one of the NTDs with a clear potential for elimination: it is easily preventable if shoes are consistently worn and early stages can be successfully treated. Currently, control efforts are hampered by a lack of information on geographical distribution. Maps have long been crucial in the planning of disease control. They help in identifying those populations most at risk from NTDs, ensuring they receive treatment, and helping track progress in control.
With funding from the Wellcome Trust, researchers from Ethiopia, Kenya, UK and the US will be pooling their expertise to develop the Global Atlas of Podoconiosis to better enable policy makers and public health implementers to target their control and elimination efforts.
Lead researcher for the atlas is Dr Kebede Deribe from Brighton & Sussex Medical School, “This collaborative effort will lead to an end to the neglect of podoconiosis. The much needed atlas will be used as an advocacy tool to develop an evidence-based global strategy and case for investment. I believe the atlas will provide an important basis for expanding prevention and treatment services of podoconiosis and complement the global elimination of lymphatic filariasis.”
Over the course of the next 5 years the atlas will define the epidemiology and distribution of podoconiosis globally. Working closely with endemic countries, the WHO and development partners, the project will collate all globally available epidemiological data. Through the application of cutting geostatistical models and machine learning approaches the global limits of the disease will be defined and the population at risk and burden of the disease estimated for the first time.
In-line with the WHO’s call for integration of NTD control efforts the project is integrating podoconiosis mapping with the ongoing mapping of other NTDs.
The benefit of this mapping on the diagnosis and treatment of other NTDs is emphasised by LASER’s Dr Jorge Cano, “Until very recently, most elephantiasis cases in Ethiopia were wrongly attributed to lymphatic filariasis. Analysis by Dr. Kebede Deribe, in collaboration with LASER , identified podoconiosis as the main cause. An open access map which enables users to identify disease hotspots will be an invaluable resource for the targeting of both podoconiosis and LF treatment and prevention programmes. ”
Once completed the atlas will provide vital evidence of the geographical distribution and burden of podoconiosis globally, and provide an important basis for expanding prevention and treatment services on the path towards a world without podoconiosis.
Further resources
- Mapping of lymphatic filariasis and podoconiosis in Ethiopia
- Deribe K., Cano, J., et al. (2017) The global atlas of podoconiosis. Lancet Global Health, Volume 5, No. 5, e477–e479, May 2017
Francis Peel, 03/05/2017
Globally, in 2010, an estimated 1.5 billion people were infected with at least one species of soil-transmitted helminth (STH), Ascaris lumbricoides, Trichuris trichiura and hookworm.
To control these infections, the World Health Organization recommends periodic mass deworming programmes of at risk populations including pre-school and school aged children. To support the long-term success of these deworming programmes it is widely accepted that communities need adequate sanitation, meaning access to and use of toilet facilities.
Newly published research led by Dr William Oswald from the London Applied & Spatial Epidemiology Research group (LASER), seeks to build the evidence-base around this relationship between higher community sanitation usage and lower STH infections.
The analysis draws on data collected from population-based surveys and stool samples collected over a three year period to look at the association between the proportion of households in a community with latrines in use and the prevalence of STH infection among school-aged children in Amhara, Ethiopia.
The dataset linked community, household and individual information from over 11,000 children with complete parasitological results.
The data showed that children in communities with lower sanitation usage were on average poorer, with less household education and access to health facilities, than those in communities with higher sanitation usage.
The analysis did not find evidence that increased community sanitation usage offered the children surveyed increased protection against STH infection. Indeed, in the case of Trichuris trichiura and Ascaris lumbricoides STH species, prevalence of infection was higher in communities where more latrines were in use.
These findings contrast with current understanding of the relationship between community sanitation and STH infections. Potential explanations for these findings range from the parasite infections pre-dating sanitation improvements to the impact of families sharing toilet and washing facilities.
The research highlights the complexity of the relationship between community sanitation and improved health outcomes and the need for continued investigation of the multiple factors impacting on infection rates.
Further information
- Download: Oswald et al. Association of community sanitation usage with soil-transmitted helminth infections among school-aged children in Amhara Region, Ethiopia. Parasites & Vectors (2017) 10:91
- This paper was published as part of Parasites & Vectors’ London Centre for NTD Research Article series
- Find and download LASER research from our publications library
A new paper published in Infectious Diseases of Poverty has identified that whilst more frequent deworming reduces infection amongst school-aged children, treatment programmes need to look beyond the school to achieve elimination.
School-based deworming is widely implemented in various countries to reduce the burden of soil-transmitted helminths (STHs), however, the frequency of drug administration varies in different settings.
A new study investigates the relative impact of a single annual treatment and 4-monthly treatment on STH prevalence rates amongst Kenyan school children. Using this information it also assesses whether school based deworming alone is enough to eliminate STH infections.
Results
In the 4-monthly treatment group, the proportion of children infected with hookworm decreased from 59.9 to 5.7%, while Ascaris lumbricoides infections dropped from 55.7 to 6.2%.
In the single treatment group, hookworm infections decreased over the same time period from 58.7 to 18.3% (12.6% absolute difference in reduction) and A. lumbricoides from 56.7 to 23.3% (17.1% absolute difference in reduction.
Residual hookworm infection among children on 4-monthly treatment were associated with male sex and baseline nutritional status, whereas A. lumbricoides infection was associated with individual and school-level infection at baseline, latrine cleanliness at schools.
Conclusions
The studies results show that 4-monthly treatments were more effective than a single annual treatment. Repeated treatments dramatically reduced the intensity of infections, but failed to completely clear STH infections among school children in Kenya.
This suggests that increasing the treatment frequency among school children alone may not be sufficient to interrupt transmission in such a community.
Such findings highlight the impact of periodic deworming for reducing the intensity of infections, but in order to reduce transmission in the community, the following should be emphasized:
- The need for integrating deworming with interventions that help reduce exposure to infections such as access to improved WASH at both school and household levels, and
- The value of expanding treatment to the entire community.
Visit our publications database to download 'Kepha, S. , Mwandawiro, CS., Anderson, RM., Pullan RL., Nuwaha F., Cano J., Njenga SM., Odiere MR., Allen E., Brooker SJ., Nikolay B., (2017) 'Impact of single annual treatment and four-monthly treatment for hookworm and Ascaris lumbricoides, and factors associated with residual infection among Kenyan school children' Infectious Diseases of Poverty2017 6:30 DOI: 10.1186/s40249-017-0244-z
Access and download a range of training materials to help users to plan, implement and evaluate evidence-based and cost-effective NTD control programmes.
GIS basic training
LASER have developed a series of GIS practicals to build capacity in NTD mapping. These tutorials use Quantum GIS, an open source mapping software which can be downloaded free of charge.
LASER have developed practicals in both English and French for versions 2.18.9 Quantum GIS (manuals for QGIS1.0 and 2.0 are also available in English and Spanish). The practicals are designed to be useful as stand alone resources.
The datasets have been created purely for the purposes of this tutorial and are not reflective of any real-life surveys or programmes.
Manuals to download
- Practical Guidelines for Users of Quantum GIS 2
-
- Practical 1: Becoming familiar with Quantum GIS interface and GIS features (pdf)
- Practical 2: Managing data tables and creating spatial data sets (pdf)
- Practical 3: Analysing spatial data sets (pdf)
- Practical 4: Processing GIS data (pdf)
- Practical 5: Data management for mapping (pdf)
Download the French translation: Outils modernes pour les programmes de contrôle des MTN (pdf)
- Quantum GIS 2 Appendixes
-
- Appendix 1: QuantumGIS main interface (pdf)
- Appendix 2: Vector properties dialog (pdf)
- Appendix 3: Downloading data points from a GPS device to QGIS (pdf)
- Quantum GIS 2 Data practicals
-
- Data for GIS practicals 1-3 (zip)
- Data for GIS practical 4 (zip)
- Data for GIS practical 5 (zip)
- The Mapping of Intensified Case Management NTDs using Quantum GIS 2.18.9
-
- Practical 1: Becoming familiar with Quantum GIS interface and GIS features (pdf)
- Practical 2: Managing data tables and creating spatial data sets (pdf)
- Practical 3: Creating your map layouts using the print composer in QGIS (pdf)
- Practical 4: Approaches to geo-referencing locations (pdf)
- Practical 5: Basic GIS geoprocessing (pdf)
Download the complete Modern Tools for NTD Control Programmes: Practicals 1- 5 (pdf)
Download the French translation: Outils modernes pour les programmes de contrôle des MTN (pdf)
- Quantum GIS 2.18.9 Data
-
- Data for practicals 1-5 (zip)
Standard operating procedures and data collection toolkits
The research team behind the TUMIKIA Project have made the standard operating procedures, training aids, case report forms, and consent forms that they used in the field and laboratory freely available for download.
The TUMIKIA Project’s research and implementation activities were underpinned by electronic data collection using Android smartphones.
All data collection forms used were developed by the project team and programmed by Dr William Oswald, Stefan Witek-McManus, and Stephen Okiya for use with the SurveyCTO (Dobility, Inc.) mobile data collection platform.
Manuals, printable copies of forms, and the respective xlsforms (programmed for use with SurveyCTO) are provided here.
- Household Questionnaire and Stool Sample Collection Form
-
This form was used by TUMIKIA field officers during cross-sectional parasitological surveys and includes a census, sociodemographic questions, and reported and observed measures of water & sanitation access. A randomisation function selects a household member to answer individual-level behaviour questions and provide a stool sample. The form includes scanning of QR codes on sample pots, efficiently linking household and individual data with laboratory results.
The download includes:
- Field Officer Manual
- Household Questionnaire and Sample Collection Form - Includes a printable version and xlsform for use with SurveyCTO
Download the Household Questionnaire and Stool Sample Collection Form
- Laboratory Kato-Katz Forms
-
A suite of forms covering the processes for stool samples in the laboratory, from sample receipt, slide reading and reporting, to quality control. All forms are centred on the unique sample QR code used in the field.
The download includes:
- Laboratory Technician Manual
- Laboratory Sample Receipt Form – Includes a printable version and xlsform for use with SurveyCTO
- Laboratory Kato-Katz Reporting Form – Includes a printable version and xlsform for use with SurveyCTO
- Laboratory Kato-Katz Quality Control Reporting Form – Includes a printable version and xlsform for use with SurveyCTO
GPS guidelines
Download a global positioning system (GPS) training manual, developed in collaboration with the Liverpool School of Tropical Medicine.
The GPS training manual has four appendixes with further information depending on your needs:
- Using a handheld GPS receiver (model GARMIN eTrexH) in field data collection
- Using a handheld GPS receiver (model GARMIN GPS MAP) in field data collection
- Download data points from a GPS device using EasyGPS software
- Download data points directly from a GPS device into a QuatumGIS framework
Please contact Jorge Cano Ortega if you have any questions about using these tools. As part of our ongoing efforts to improve our resources, we also welcome and value your feedback.
Tutorial Kato-Katz thick smear
The ongoing mass drug donations to control and eliminate neglected tropical diseases could prove uninteresting for research purposes if a problem of reproducibility arises. In order to improve standardization of operational procedures, scientists from Jimma University in Ethiopia and Ghent University in Belgium have developed seven visual tutorials focusing on schistosomiasis and soil-transmitted helminthiasis.
The first three tutorials provide detailed information on how to perform both traditional and newly developed methods to diagnose and quantify infections in stool, including Kato-Katz thick smear, McMaster egg counting method and Mini-FLOTAC: